|
 
 |
| REVIEW ARTICLE |
|
| Year : 2013 | Volume
: 1
| Issue : 1 | Page : 1-10 |
|
Abutment selection, designing, and its influence on the emergence profile: A comprehensive review
Sagar J Abichandani, Ramesh Nadiger, Abhishek S Kavlekar
Department of Prosthodontics, Sri Dharmasthala Manjunatheshwara College of Dental Sciences, Dharwad, Karnataka, India
| Date of Web Publication | 16-Aug-2013 |
Correspondence Address:
Sagar J Abichandani
Ashiyana, 105-B, 1st floor, Sindhi Society, Chembur, Mumbai-400 071
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.116586

The implant evolution has become a "restorative driven" field, and it is therefore important to know the designing principles of abutments and its connection to the implants and its rationale for use in clinical practice. The key is to have an optimum selection and designing of the implant to meet the implant position and angulation in the clinical scenario. A search was conducted both manually and electronically to find terms that included dental implants, dental abutments, custom abutments, cast abutments, abutment-implant interface, emergence profile, soft tissue profile, provisional restoration, CAD/CAM abutments, abutment innovations, abutment designing, abutment selection, and abutment materials. A total of 4332 English titles were obtained in various combinations and were repeated and duplicated due to multiple searching. Proper short-listing of the articles was done and a comprehensive review was formulated. This review article highlights various methods and rationale behind selection, designing of various abutments, its influence on emergence profile, and the newer advances and trends that have emerged in the field of implant dentistry. Keywords: Cement retained abutment, custom abutment, implant abutment, screw retained abutment
How to cite this article:
Abichandani SJ, Nadiger R, Kavlekar AS. Abutment selection, designing, and its influence on the emergence profile: A comprehensive review. Eur J Prosthodont 2013;1:1-10 |
How to cite this URL:
Abichandani SJ, Nadiger R, Kavlekar AS. Abutment selection, designing, and its influence on the emergence profile: A comprehensive review. Eur J Prosthodont [serial online] 2013 [cited 2018 Jul 12];1:1-10. Available from: http://www.eurjprosthodont.org/text.asp?2013/1/1/1/116586 |
| Introduction | |  |
Being functionally useful is the similarity between a natural tooth and endosteal dental implants, as they have to emerge into the oral cavity after piercing the oral mucosa. This trans-mucosal connection can be a pathway for toxic substances or organisms. Therefore, to protect the peri-implant structures, it is imperative to have a long-standing, effective barrier as otherwise there bacteria could penetrate, affecting the primary stability, initial healing, or long-term success of implant-supported restorations. [1],[2],[3],[4],[5],[6],[7]
About 2 mm biological width of the epithelial surface and connective tissue adhesion areas form an interface preventing the entry of bacteria and their by-products. Peri-implant sulcular epithelium is similar to junctional epithelium, [8],[9],[10] as per a general consensus drawn. However, on the other hand, difference is seen between the connective tissue components of the implant with respect to that of the tooth. [11],[12],[13] Instead of a true anchorage of the supra-alveolar connective tissue, only a brittle adhesion exists due to the lack of cementum and solid nature of the transmucosal components, [4],[6],[14],[15] thereby affecting the long-term prognosis of dental implants. Further damage can rise in the form of apical migration of the junctional epithelium, bone resorption, pocket formation, and gingival recession [16] if there is an occurrence of tearing at connective tissue-implant surface. Hence, for enhancing the quality of soft tissue interface, such as alterations in the micro design [17],[18] or changes in the macro design of transmucosal implant components, various methods have been postulated.
| Materials and Methods | |  |
A search was conducted both manually and electronically to find terms that included dental implants, dental abutments, custom abutments, cast abutments, abutment-implant interface, emergence profile, soft tissue profile, provisional restoration, CAD/CAM abutments, abutment innovations, abutment designing, abutment selection, and abutment materials. A total of 4332 English titles were obtained in various combinations and were repeated and duplicated due to multiple searching. Proper short-listing of the articles was done and the comprehensive review was formulated.
| Key to Diagnosis | |  |
Diagnostic aids in the form of a thorough clinical, diagnostic, and radiographic examination should be the gold standard for optimum success; hence, multi-disciplinary team approach is the key. At the implant site, the final outcome would be detrimental to both functionally and esthetic wise, hence adequate alveolar bone in terms of height, volume, and thickness of cortical bone shold be considered. Treatment modality should be decided on individual basis [19],[20],[21],[22],[23] in the form of immediate or delayed implant placement with provisionalization.
| Provisional Restoration and its Role in Esthetics | |  |
To shape, prepare, and stabilize the peri-implant soft tissues during the healing phase and after second-stage surgery in addition to providing an aid in esthetic evaluation before the finalization of the treatment are the various purposes that provisional restoration can serve, thus giving comfort and psychological advantage to the patient. [24] It can either be a provisional fixed partial dentures when adjacent teeth also require restorations [25] or removable partial denture, vacuum-formed matrices with denture teeth, and resin-bonded restoration. Formation of an optimum emergence profile [25],[26] is the only way to achieve natural appearance of the implant-supported restorations. The key for this emergence profile is the interdental papillae that itself depends on various factors including proper contouring of subgingival abutment component, position of the contact point of the restoration, and height of the bony crest at the neighboring teeth.
| Selection of the Implant Abutment | |  |
The following pre-requisites for optimum abutment selection should be as follows:
- Long-term stability [27]
- Accurate fit of the components to prevent screw loosening during function [28]
- Biocompatibility
- Esthetics [29]
| Material Selection | |  |
Titanium abutments and ceramic abutments [30],[31],[32] are the two things with which marginal bone stability and soft tissue responses have been favorably noted. Abrahammson et al. showed how the abutment material influenced height and quality of the tissues, whereby titanium and ceramic abutments caused formation of mucosal attachment and metal-ceramic abutments led to soft tissue recession and increased crestal bone resorption. [30] The use of all-ceramic components and restorations is increasing, despite superior fracture strengths of metal-ceramic crowns cemented on titanium abutments as compared with all-ceramic crowns cemented on ceramic abutments. [31] Excellent esthetic potential and biocompatibility along with long-term stability is offered by ceramic abutments.
Accumulation of fewer bacteria was seen on zirconia surface as compared to commercially pure titanium, [33] according to a recent in vitro and in vivo study. All ceramic abutments, [34],[35] wherein it was observed that the fracture strength of both materials far exceeded the maximum values for incisal loading, as reported in the literature though zirconia abutments, were twice as resistant to fracture as alumina abutments; this was seen in another in vitro study [36] that investigated the fracture resistance of implant.
| Designing Abutments | |  |
They can either by pre-fabricated or customized abutments. From the perspective of posterior restorations, although the standard dimensions are sufficient, optimum results may not be yielded from its usage in the anterior esthetic zone. [21] Hence, to cater to individual dentition when dealing with the esthetic zone customizing the abutments should be the objective. Direct porcelain application to a standard abutment or by using CAD-CAM techniques are the two ways in which customization can be achieved. Superior material homogeneity, custom designing, ease of fabrication in addition to supporting poor tissue contours, and eliminating compatibility concerns of dissimilar metal alloys are the various advantages being offered by CAD-CAM machines. [35]
| Screw-Retained Versus Cement-Retained Prosthesis | |  |
Whether to opt for cementation of the implant-retained crown to the abutment or whether the abutment-crown complex is screw retained depends on the clinician and the position of the implants. A screw-retained restoration may be fabricated if the screw access is favorable (long axis of the implant and screw access hole are located on the lingual of the incisal edge). First, the ceramic is directly fired onto the abutment and the abutment-crown complex can be easily screwed onto the implant. The possibility for retrieval or retightening and reassessing the abutment screw can be offered by this type of restoration. The absence of cement between the abutment and the crown is another advantage that this offers. Chipping of the veneering ceramic because of the discontinuous porcelain may be some possible complications of such restoration. Compensation of misaligned implants and can be treated like natural teeth are allowed by cement-retained restorations on customized ceramic abutments allow. A provisional crown can stabilize and help mature the surrounding and restoration tissues after insertion. Frequent removal and reinsertion of provisional restorations becomes unnecessary, [21] minimizing gingival trauma. The height of the interproximal crown margin should be located just below the gingival margin to allow for complete removal of cement, because the presence of cement may compromise soft tissue health [35],[36] if a screw-retained, customized abutment is selected.
| Recent Advances in the use of Material: Introduction of Acetal | |  |
To eliminate and minimize the grayish appearance of the gingiva resulting from the transmucosal path of the abutment, use of acetal has been introduced. [37],[38],[39] Acetal, which is polyoxymethylene, is a highly crystalline thermoplastic polymer that has a unique composition, and it can be used in applications where dimensional stability is important, even when the acetalic part is under continuous stress. Features of the material that are also predictable over a wide range of temperatures for long periods are the strength, stiffness, toughness, and resistance to fatigue under repeated stress. Acetals resist a wide range of solvents and are not hygroscopic. In harsh environments, they remain dimensionally stable. These features make acetals ideal for use as metal replacements. [40],[41],[42]
| Abutment Connections and the Recent Advances | |  |
Several externally hexed implants to restore fully edentulous arches, linking them together via a metal bar with a fixed prosthesis [43],[44] was the requirement of the original Branemark protocol. In this protocol, the external hex design was present to help screw the implant into place. The hex was not engaged as an antirotation device for the fully edentulous, fixed prostheses abutments that were screwed down onto the implants. [45] The hex had to be used to prevent rotation of the abutment and the single crown, when the implants were later placed in single-tooth or partially edentulous cases. This external hex, which was only 0.7 mm in height, was not designed to withstand the forces directed on the crowns intraorally. [46],[47],[48] Hence, changing the type of screw used (e.g., geometry, height, surface area), the precision of the fit over the hex, and the amount of torque used to secure the new screws were the ways in which implant manufacturers compensated. Although such efforts still require the clinician to radiographically verify that the abutments are fully seated, these changes have allowed externally hexed implants to be utilized with great confidence.
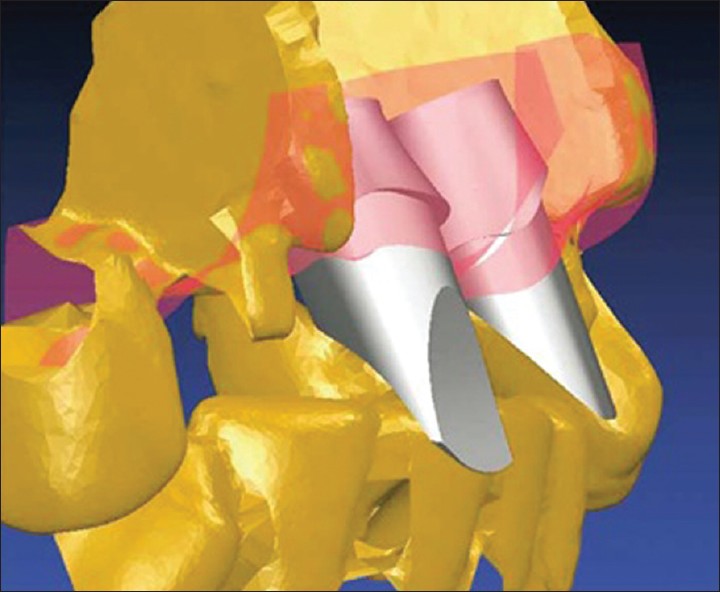
To improve the original external hex implant/abutment interface, new interface designs are utilized on a variety of implants. To improve connection stability throughout function and placement and to simplify the armamentarium necessary for the clinician to complete the restoration are some goals of the new designs. There are at least 20 different implant/abutment interface variations on dental implants that are cleared for marketing by the FDA [Figure 1]. Joint strength, stability, and lateral and rotational stability are determined by the implant/abutment interface. Different requirements are incorporated into the interface design as implant design evolves. One of the first internally hexed implants was designed with a 1.7-mm-deep hex below a 0.5-mm-wide, 45° bevel. [49],[50] To protect the retention screw from excess loading [50],[51] and to reduce the potential of microleakage [47] was the main intention to distribute intraoral forces deeper within the implant. Superior strength for the implant/abutment connection are also provided by internally connected implants. [52],[53],[54] Further design enhancements have been made in an attempt to enhance the implant/abutment connection [Table 1], since the introduction of the internal connection concept. [55],[56],[57],[58] A tapered abutment post is inserted into the non threaded shaft of a dental implant with the same taper, which is the "Morse" taper. [57],[58] Frequently, with variations in their use of joint designs (e.g., bevel, butt) or the numbers of "hexes" present for the restorative phase, other internal connection designs have followed. [56],[57],[58]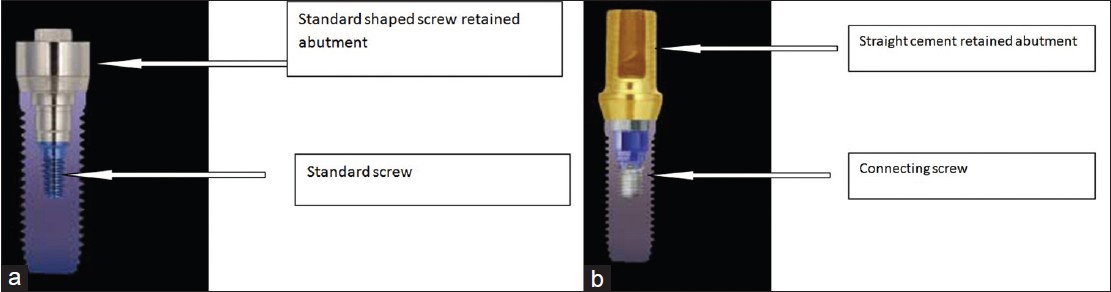 | Figure 1: (a) Standard abutment for a screw-retained abutment; (b) Abutment for a cement-retained restoration
Click here to view |
Clinicians have to be mindful of their application in the intraoral environment, an often challenging region due to the involved bone topography, soft tissue contours, rotational forces, and the requisite prosthetic components, particularly or aesthetic, single-implant restorations when using these implant/abutment connections. Demonstrating how interface design has continued to evolve a new internal connection implant design (e.g., Osseotite Certain, 3i Implant Innovations Inc., Palm Beach Gardens, FL) has recently been introduced to the profession. When the components are properly seated, the internal connection implant design incorporates an audible and tactile "click." This unique feature eases placement for the clinician and may reduce the need for radiographs following placement of the restorative components. With contact along a significant length that provides lateral stability from off-axis forces, the implant's internal connection allows 4 mm of internal engagement. [52],[53],[54],[55] The deep, 4-mm multilevel engagement zone of this internal connection achieves a precise, secure connection with low torque. No more than 20 Ncm is required to maintain screw retention without loosening. The design of the internal connection allows flexibility in abutment preparation without damaging the head of the screw, thereby allowing the height of the screw to be only 1.95 mm from the top of the screw to the seating surface. An internal connection with retentive features allows placement of transfer copings and abutments with secure seating and ease of use from a restorative perspective. The click allows the abutment to remain in place in the maxillary arch even prior to placement of the retaining screw and confirms positive seating. This internal connection design incorporates a 6-point hex and a 12-point double-hex internal design. A stable base for the use of straight abutments is provided by the 6-point internal hex. Also, 30° increments of rotational flexibility for placement of machined pre-angled abutments to correct the off-axis emergence of the implant [Figure 2], [Figure 3] and [Figure 4] is allowed by the 12-point double-hex of the internal connection. Flexibility for the restorative dentist and enabling the surgeon to place the implant in any rotational position without concern for orienting the flats of a hex during surgery is provided by this feature. The involved expenses for the case and the simplified laboratory and restorative procedures for an implant-supported prosthesis are decreased. The implant can be oriented by the hex flats on the implant placement driver tip. In addition, if a provisional crown is fabricated prior to implant placement for delivery at the time of implant surgery (i.e., in lieu of a cover screw). Abutments that provide a large variety of prosthetic options using the same implant for multiple clinical situations are adapted well by the internal connection. Ease of placement for the transfer copings and abutments are allowed by the audible and tactile confirmation of seating the components into the implant, combined with the 12-point double-hex design that enables simple alignment for angled abutments.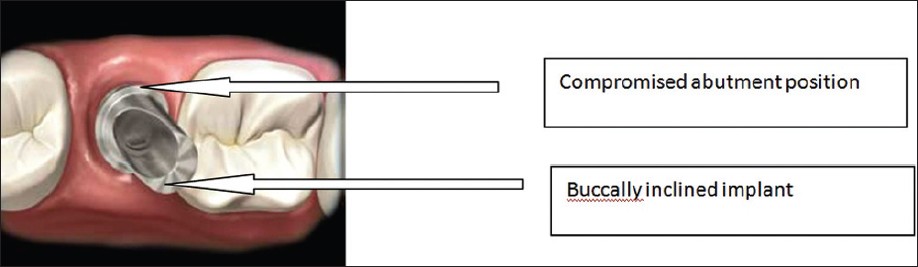 | Figure 2: Pre-machined abutments can have positioning limitations because of the number of rotational positions within the internal connection implant design
Click here to view |
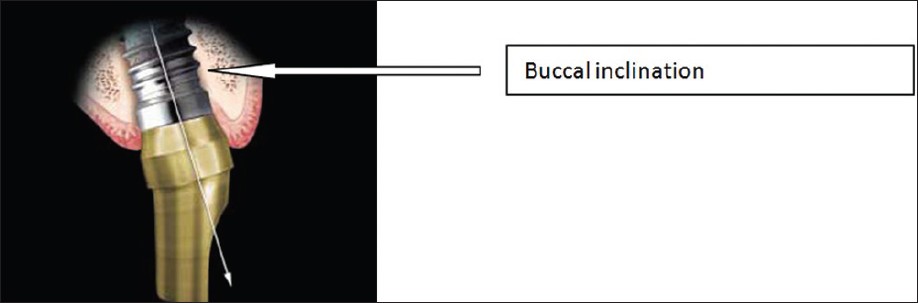 | Figure 4: Pre-angled abutment in place redirect the path of insertion for a bucally inclined implant
Click here to view |
| Cad Cam Abutments: An Overview | |  |
To shift from manufacturing systems designed for mass production of identical components (such as stock abutments and cast custom abutment platforms) to sophisticated systems that could deliver abutments specifically made for each individual restoration in a cost-efficient and timely manner, considerable technical innovation and financial investment have been required. [59] Several implant manufacturers now offer CAD/CAM patient-specific abutment systems as the hurdle of providing completely individualized abutments has been overcome. [60] To provide the advantages f both stock and laboratory processed custom abutments without the disadvantages are the potentials offered by custom abutments created with CAD/CAM technology [Table 2]. First, CAD/CAM abutments are specific for each patient, similar to laboratory made abutments. However, the results are much more consistent. The technician's learning curve is less steep than that for handmade components. The CAD software that incorporates parameters is used to control the abutment design by the technician. A CAM milling apparatus that creates the abutment from a block of the selected abutment material is electronically transferred by the virtually designed abutment. Most of the inherent dimensional inaccuracies of waxing, investing, and casting are eliminated. In a dental laboratory, casting of titanium, in particular, is complex. A homogenous mass of titanium with optimum material properties is a result of CAD/CAM machining. [61] CAD/CAM custom abutments are machined to the precision that immovable implants require. The abutment surfaces of CAD/CAM abutments are not subjected to the above-mentioned manipulation processes after machining, unlike stock or cast custom abutments. The abutment surface of a stock or cast custom abutment is not significantly affected when laboratory steps are meticulously followed, as shown by Vigalo et al.[62] Heat-induced changes of pre-machined abutment platforms during casting procedures reduced the contact between the abutments and corresponding retaining screws, as found by Byrne et al. [63] From a review of implant abutment preparation techniques, dentists and laboratories should select implant/abutment interfaces that demonstrate superior fit, and they should follow laboratory procedures that would not induce further discrepancies, as concluded by Wee et al. [27] CAD/CAM abutments have the potential to provide most accurate fit of any abutment type, because their interfaces do not require manipulation after machining. The accuracy of CAD/CAM abutments has increased having specific application to implant dentistry, where precision of components may affect implant longevity, prosthetic success, and ease of restoration. Hard ceramic materials used for abutment fabrication cannot be efficiently machined with conventional grinding tools, ideally ceramic implant abutments should be machined from completely sintered blocks of material. Hence, before firing, they are presently milled in the green body state. [59] The cost of a CAD/CAM implant abutment presently lies somewhere between the two when compared with a stock and cast custom abutment. As CAD/CAM systems for abutment fabrication become commonplace and the high initial capital outlays made by manufacturers are distributed over a growing number of abutments sold, this expense is likely to decrease over time. Conversely, costs of labor-intensive laboratory processes and manpower are likely to escalate, thereby increasing the cost of prepared stock abutments or handmade cast custom abutments. In addition, CAD/CAM manufacturing reduces the work needed to create implant abutments considering the shortage of qualified laboratory technicians. [64]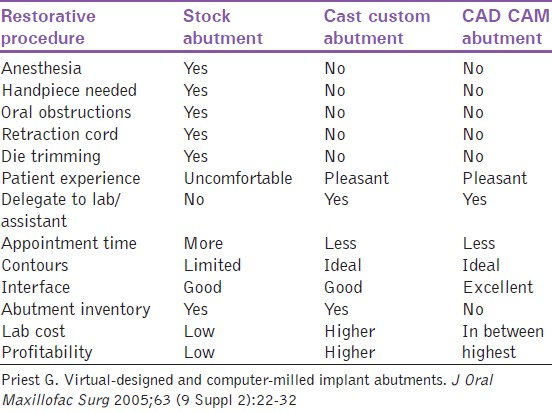 | Table 2: Comparison of the stock, cast custom and CAD/CAM implant abutments
Click here to view |
| Cad/Cam Abutments: Systems Available | |  |
Since the early 1990s, the Atlantis Abutment (Atlantis Components Inc., Cambridge, MA), milled in titanium alloy, has been commercially available. [65],[66] Fabrication and abutment design is outsourced to the Atlantis facility and may be prescribed by the implant surgeon, restorative dentist, or laboratory technician.
The option of placing a provisional crown on the first abutment and a definitive crown on the second is provided by Atlantis to give dentists a second duplicate abutment. [67] The second abutment may also be used as a laboratory die. To improve gingival tones and to impart more natural shades through all-ceramic restorations, gold-anodized coatings have been added. Excellent marginal detail and anatomic gingival contours are the things Atlantis abutments are purported to have. [68] An implant positioning index or single impression [69] can be made at the time of implant surgery. Hand modifications of the abutment margin before crown fabrication may necessitate for ensuing tissue recession during soft tissue healing. [68] Initially developed for titanium and aluminum oxide copings for conventional crowns, [40] Procera (Nobel Biocare, Yorba Linda, CA) has recently added implant abutments to their line of CAD/CAM components. [70] The abutment is virtually designed by the local laboratory using a Procera digital scanning system and software purchased from Nobel Biocare with this system. The information is electronically transmitted to a Procera facility, where the virtual abutment is milled and returned to the local laboratory. Both a CAD/CAM abutment and CAD/CAM titanium or ceramic coping using this same system are the options that the dentist can receive. Cast restorations have proven to be comparable with fit and marginal adaptation. [71],[72],[73] Procera ceramic abutments clinically perform as well as or better than other abutment types, as indicated by their short-term results. [74] A new line of CAD/CAM components under the umbrella of Architech PSR (for patient specific restoration) has been developed by Implant Innovations Inc. (Palm Beach Gardens, FL). The aptly named custom abutment segment of the system, Encode, incorporates codes or facets on the occlusal surface of the corresponding healing abutments [Figure 5]. Implant size, hex position, implant location, and soft tissue levels are determined by an optical scanner interprets these code. The surgeon may make an index of implant positions at the time of implant surgery or uncovering, similar to the Atlantis Abutment System protocol [Figure 6], [Figure 7] and [Figure 8]. The local laboratory later uses this index to make a cast for seating the final Encode abutments and fabricating the definitive restorations. The Encode healing abutments is then placed by the surgeon [Figure 9]. The restorative dentist makes only 1 impression of the Encode healing abutments in place, eliminating the need to make a restorative phase implant level impression, following implant integration and soft tissue maturation [Figure 9] and [Figure 10]. The entire Encode process is outsourced to Implant Innovations Inc. after the local laboratory technician pours and sections the cast [Figure 11]. The codes embedded in the healing abutments can be read and translated by an optical scanner [Figure 12]. This data is transferred to the CAD software, the implant abutments are virtually designed [Figure 13], and the CAM milling apparatus produces the final titanium abutments. Definitive restorations are made on a cast created from the surgeon's positioning index after the completed abutments are returned to the local laboratory [Figure 14] and [Figure 15]. The restorative dentist at delivery of the abutment and final prostheses removes the Encode healing abutments. Patient-specific final abutments are seated [Figure 16] and definitive crowns are placed [Figure 17]. A novice restorative dentist, who is not completely comfortable with implant procedures, is not required to make an implant level impression; this is a particular advantage provided by this approach. Minimizing the likelihood of modifications before crown fabrication is a possibility, because, as the restorative dentist makes a healing abutment level impression of mature soft tissue levels, marginal form and depth of the definitive Encode abutment is precise. To become the tool for design and creation of dental restorations, hand instruments will be replaced by computer keyboards. Outsourced CAD/CAM implant abutments will free qualified technicians to focus on their artistry rather than on labor-intensive procedures given the shortage of laboratory technicians. Overall turnaround time is decreased between the laboratory and restorative dentist as implant abutments are manufactured in a matter of minutes. Dental laboratories do not have to invest in sophisticated technology to provide this superior service because CAD/CAM abutment fabrication is outsourced to an authorized facility. Restorative clinicians will rely less on conventional dental techniques to restore implants using computer-generated implant abutments. Implant dentistry is made easier by simplified restorative protocols of CAD/CAM abutment systems, particularly for the novice restorative implant dentist. Greater stability and more consistent implant esthetics are provided by improved marginal fit and ideal contours of CAD/CAM custom abutments. The cost of custom abutment fabrication is reduced by CAD/CAM systems. The need for implant impressions will be eliminated by intraoral implant scanning technology, further distancing dentistry from outdated restorative procedures as they incorporate these systems into their routine implant protocols. As dentists embrace CAD/CAM innovations that simplify implant dentistry and create predictable and stable implant interfaces, they are more likely to recommend and deliver implants as their preferred option of tooth replacement for patients. | Figure 5: Unique encoded healing abutments are read by an optical scanner to determine the implant size, hex position, implant location, and soft tissue levels
Click here to view |
 | Figure 6: Both fractured maxillary central incisors is replaced with implant restorations
Click here to view |
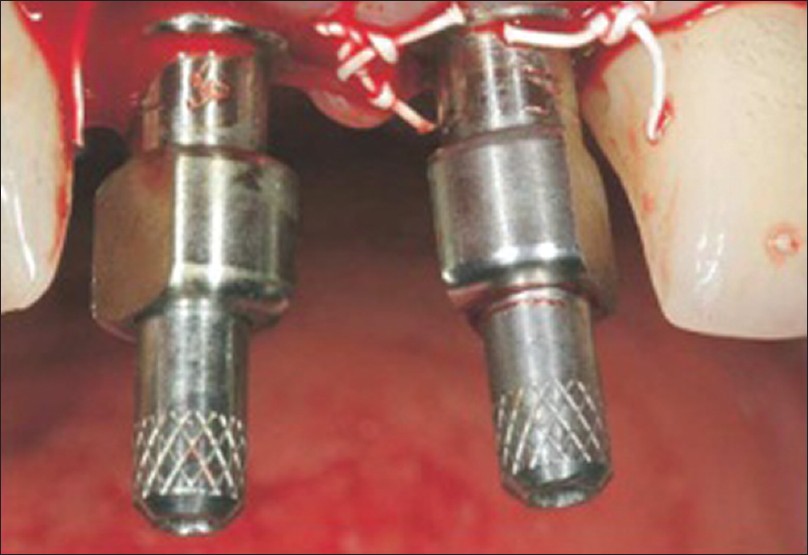 | Figure 7: After implant placement, the surgeon seats direct impression copings
Click here to view |
 | Figure 8: After removing the index, the surgeon places the encoded healing abutments
Click here to view |
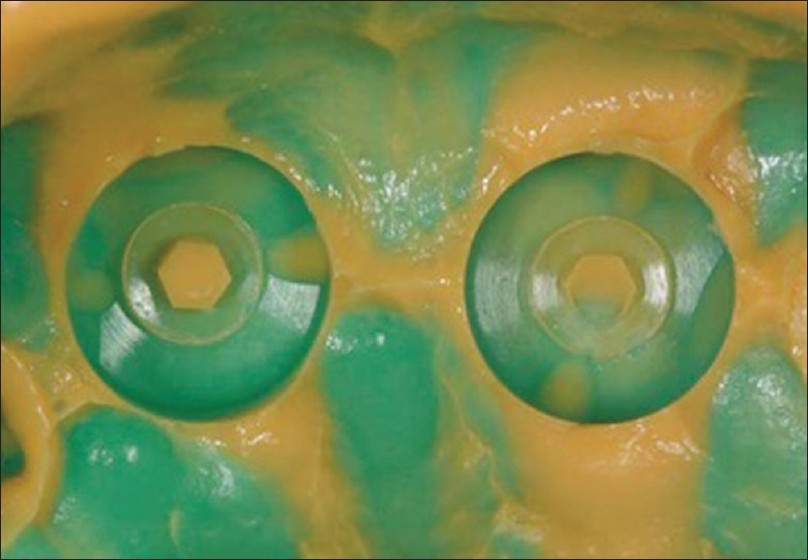 | Figure 10: A heavy body polyvinlysiloxane impression is made of the
encoded healing abutments by the restoring dentist
Click here to view |
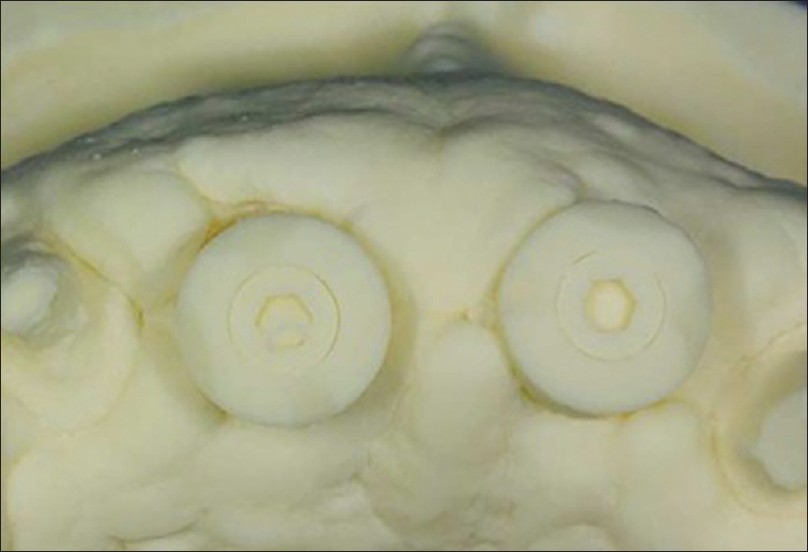 | Figure 11: Laboratory pours the cast in die stone and sections the encoded healing abutments
Click here to view |
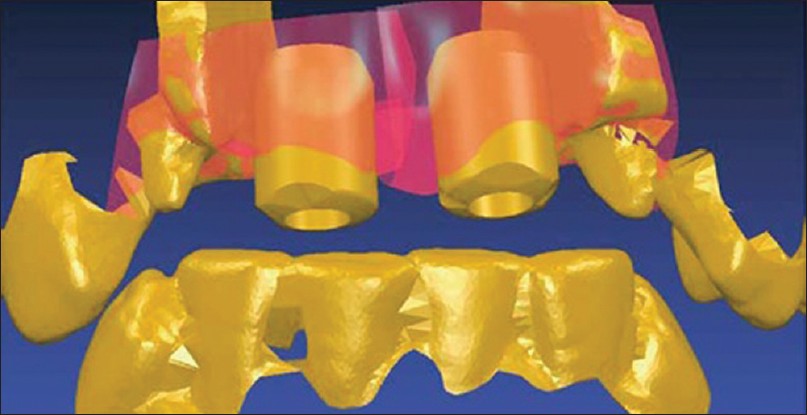 | Figure 12: An optical scanner translates the data to a virtual soft image of the encoded abutments, teeth, and the surrounding soft tissues
Click here to view |
 | Figure 13: Patient specifi c fi nal abutments are created virtually on a
computer monitor
Click here to view |
 | Figure 14: Completed titanium custom abutments are returned to the laboratory, where they are placed on the cast from the surgical implant positioning index
Click here to view |
 | Figure 15: Close examination of the abutments showa smooth marginal chambers and excellent abutment/analog interfaces
Click here to view |
 | Figure 16: Restorative dentist secures the Encode final abutment to specific torque
Click here to view |
| Novel Implants/Gap-Free Abutments | |  |
Dental implants fabricated with gap-free abutments, wherein a shape memory alloy has been used, shows a reduction in the bacterial leakage that could reduce the adverse effects of peri-implant, contributing to the long-term success of dental implants as previously shown. [28]
| Esthetic Titanium Abutments/Conical Abutments | |  |
The restoration is allowed to begin at a more subgingival level, and this is an advantage provided by the esthetic conical abutment. The restoration can begin just 1 mm above the implant, with the 1-mm conical abutment [75] . Thus, as the working distance has increased, a more gradual and natural emergence profile of the restoration can be produced. An opportunity to place porcelain at the gingival margin is provided by the conical abutment. Not only is the resulting porcelain restoration more esthetic as it emerges through the soft tissue than one used on a conventional abutment but also clinically porcelain appears to accumulate less plaque than machined titanium. The deeper the sulcus, the longer the collar may be. The titanium collar should be at least 1 mm below the gingival margin for best esthetic results, according to past experiences. The implant must be adequately countersunk so that the 1-mm abutment collar remains sufficiently subgingival in areas of extremely thin soft tissue. Just as with the conventional components, gold alloy cylinders seat on the abutment cylinders and get incorporated within the wax pattern and resultant casting. With the gold cylinder in place, the total height of a 1-mm abutment cylinder is 5.3 mm. When conventional l 3-mm abutments and gold cylinders are used, this compares to 6 mm [76] . The level at which the restoration begins is more important in achieving esthetics than the total height. The conical abutment has at least a 2-mm advantage over the conventional components. Upto a 30° mal-alignment of the implants can be accommodated without preventing seating of the restoration because of the 15° taper of the abutment and gold cylinders. The use of angled abutments will be required in case of discrepancies beyond that. The 0.2-mm collar at the base, which provides a finish line for laboratory procedures, is another design feature of the gold cylinder. With this finish line, designing and fabricating the metal substructures and applying porcelain are much easier. Plastic healing caps, tapered impression copings, square impression copings, laboratory brass analogs, gold alloy screws, and laboratory guide pins are some other related components similar to those used with conventional components, but somewhat different in design.
| Summary and Conclusion | |  |
Implants have become the prima dona of the treatment option for the restoration of the partially or completely edentulous arches. Use of CAD/CAM abutments have brought about a revolution in the field of implant dentistry, which has been a boon for dentists who are not very comfortable making implant level impressions or resorting to conventional techniques, thus making it a viable option for replacement of the traditional conventional techniques. Most of the clinicians desire to have a divergent profile for a wider emergence diameter, which can, in turn, create centrifuge pressure at the internal side of the soft tissues.
The ultimate goal should be to achieve a harmonious relationship between the soft tissues and the hard tissues, mimicking the natural appearance in color, form, size, texture, and optical properties.
| References | |  |
| 1. | Abrahamsson I, Berglundh T, Wennstrom J, Lindhe J. The peri-implant hard and soft tissues at different implant systems. A comparative study in the dog. Clin Oral Implants Res 1996;7:212-9. 
|
| 2. | Abrahamsson I, Berglundh T, Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol 1997;24:568-72. 
[PUBMED] |
| 3. | Abrahamsson I, Berglundh T, Moon IS, Lindhe J. Peri-implant tissues at submerged and non-submerged titanium implants. J Clin Periodontol 1999;26:600-7. 
[PUBMED] |
| 4. | Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res 1991;2:81-90. 
[PUBMED] |
| 5. | Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol 1996;23:971-3. 
[PUBMED] |
| 6. | Buser D, Weber HP, Donath K, Fiorellini JP, Paquette DW, Williams RC. Soft tissue reactions to non-submerged unloaded titanium implants in beagle dogs. J Periodontol 1992;63:225-35. 
[PUBMED] |
| 7. | Cochran DL, Hermann JS, Schenk RK, Higginbottom FL, Buser D. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol 1997;68:186-98. 
[PUBMED] |
| 8. | Carmichael RP, McCulloch CA, Zarb GA. Quantitative immunohistochemical analysis of keratins and desmoplakins in human gingiva and peri-implant mucosa. J Dent Res 1991;70:899-905. 
[PUBMED] |
| 9. | Mackenzie IC, Tonetti MS. Formation of normal gingival epithelial phenotypes around osseo-integrated oral implants in humans. J Periodontol 1995;66:933-43. 
[PUBMED] |
| 10. | Liljenberg B, Gualini F, Berglundh T, Tonetti M, Lindhe J. Composition of plaque-associated lesions in the gingiva and the peri-implant mucosa in partially edentulous subjects. J Clin Periodontol 1997;24:119-23. 
[PUBMED] |
| 11. | Gargiulo AW, Wentz FM, Orban B. Mitotic activity of human oral epithelium exposed to 30 per cent hydrogen peroxide. Oral Surg Oral Med Oral Pathol 1961;14:474-92. 
[PUBMED] |
| 12. | Listgarten MA, Buser D, Steinemann SG, Donath K, Lang NP, Weber HP. Light and transmission electron microscopy of the intact interfaces between non-submerged titanium-coated epoxy resin implants and bone or gingiva. J Dent Res 1992;71:364-71. 
|
| 13. | Chavrier CA, Couble ML. Ultrastructural immunohistochemical study of interstitial collagenous components of the healthy human keratinized mucosa surrounding implants. Int J Oral Maxillofac Implants 1999;14:108-12. 
[PUBMED] |
| 14. | Rompen E, Domken O, Degidi M, Pontes AE, Piattelli A. The effect of material characteristics, of surface topography and of implant components and connections on soft tissue integration: A literature review. Clin Oral Implants Res 2006;17 Suppl 2:55-67. 
[PUBMED] |
| 15. | Adell R, Lekholm U, Rockler B, Branemark PI, Lindhe J, Eriksson B, et al. Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int J Oral Maxillofac Surg 1986;15:39-52. 
|
| 16. | Bengazi F, Wennstrom JL, Lekholm U. Recession of the soft tissue margin at oral implants. A 2-year longitudinal prospective study. Clin Oral Implants Res 1996;7:303-10. 
|
| 17. | Cardaropoli G, Lekholm U, Wennstrom JL. Tissue alterations at implant-supported single-tooth replacements: A 1-year prospective clinical study. Clin Oral Implants Res 2006;17:165-71. 
|
| 18. | Cooper L, Felton DA, Kugelberg CF, Ellner S, Chaffee N, Molina AL, et al. A multicenter 12-month evaluation of single-tooth implants restored 3 weeks after 1-stage surgery. Int J Oral Maxillofac Implants 2001;16:182-92. 
[PUBMED] |
| 19. | Ekfeldt A, Eriksson A, Johansson LA. Peri-implant mucosal level in patients treated with implant-supported fixed prostheses: A 1-year follow-up study. Int J Prosthodont 2003;16:529-32. 
[PUBMED] |
| 20. | Sclar AG. Strategies for management of single-tooth extraction sites in aesthetic implant therapy. J Oral Maxillofac Surg 2004;62:90-105. 
[PUBMED] |
| 21. | Belser UC, Schmid B, Higginbottom F, Buser D. Outcome analysis of implant restorations located in the anterior maxilla: A review of the recent literature. Int J Oral Maxillofac Implants 2004;19:30-42. 
[PUBMED] |
| 22. | Kokich VG. Maxillary lateral incisor implants: Planning with the aid of orthodontics. J Oral Maxillofac Surg 2004;62 (9 Suppl 2):48-56. 
|
| 23. | Buskin R, Castellon P, Hochstedler JL. Orthodontic extrusion and orthodontic extraction in preprosthetic treatment using implant therapy. Pract Periodontics Aesthet Dent 2000;12:213-9. 
[PUBMED] |
| 24. | Poggio CE, Salvato A. Bonded provisional restorations for esthetic soft tissue support in single-implant treatment. J Prosthet Dent 2002;87:688-91. 
[PUBMED] |
| 25. | Higginbottom F, Belser U, Jones JD, Keith SE. Prosthetic management of implants in the esthetic zone. Int J Oral Maxillofac Implants 2004;19 Suppl: 62-72. 
[PUBMED] |
| 26. | Small PN, Tarnow DP. Gingival recession around implants: A 1-year longitudinal prospective study. Int J Oral Maxillofac Implants 2000;15:527-32. 
[PUBMED] |
| 27. | Byrne D, Houston F, Cleary R, Claffey N. The fit of cast and premachined implant abutments. J Prosthet Dent 1998;80:184-92. 
[PUBMED] |
| 28. | Henriksson K, Jemt T. Evaluation of custom-made procera ceramic abutments for single-implant tooth replacement: A prospective 1-year follow-up study. Int J Prosthodont 2003;16:626-30. 
[PUBMED] |
| 29. | Andersson B, Taylor A, Lang BR, Scheller H, Schärer P, Sorensen JA, et al. Alumina ceramic implant abutments used for single-tooth replacement: A prospective 1- to 3-year multicenter study. Int J Prosthodont 2001;14:432-8. 
|
| 30. | Abrahamsson I, Berglundh T, Glantz PO, Lindhe J. The mucosal attachment at different abutments. An experimental study in dogs. J Clin Periodontol 1998;25:721-7. 
[PUBMED] |
| 31. | Rasperini G, Maglione M, Cocconcelli P, Simion M. In vivo early plaque formation on pure titanium and ceramic abutments: A comparative microbiological and SEM analysis. Clin Oral Implants Res 1998;9:357-64. 
[PUBMED] |
| 32. | Rimondini L, Cerroni L, Carrassi A, Torricelli P. Bacterial colonization of zirconia ceramic surfaces: An in vitro and in vivo study. Int J Oral Maxillofac Implants 2002;17:793-8. 
[PUBMED] |
| 33. | Cho HW, Dong JK, Jin TH, Oh SC, Lee HH, Lee JW. A study on the fracture strength of implant-supported restorations using milled ceramic abutments and all-ceramic crowns. Int J Prosthodont 2002;15:9-13. 
[PUBMED] |
| 34. | Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials 1999;20:1-25. 
[PUBMED] |
| 35. | Kucey BK, Fraser DC. The Procera abutment-The fifth generation abutment for dental implants. J Can Dent Assoc 2000;66:445-9. 
[PUBMED] |
| 36. | Yildirim M, Fischer H, Marx R, Edelhoff D. In vivo fracture resistance of implant-supported all-ceramic restorations. J Prosthet Dent 2003;90:325-31. 
[PUBMED] |
| 37. | Touati B, Guez G. Immediate implantation with provisionalization: From literature to clinical implications. Pract Proced Aesthet Dent 2002;14:699-707. 
[PUBMED] |
| 38. | Lewis S, Beumer J 3 rd , Hornburg W, Moy P. The "UCLA" abutment. Int J Oral Maxillofac Implants 1988;3:183-9. 
|
| 39. | Sinker SM. Acetals. In: Rubin I-I, editor. Handbook of plastic materials and technology. New York: Wiley; 1990. p. 11-24. 
|
| 40. | Hochwald DA. Surgical template impression during stage I surgery for fabrication of a provisional restoration to be placed at stage II surgery. J Prosthet Dent 1991;66:796-8. 
[PUBMED] |
| 41. | Gould TR, Westbury L, Brunette DM. Ultrastructural study of the attachment of human gingiva to titanium in vivo. J Prosthet Dent 1984;52:418-20. 
[PUBMED] |
| 42. | James R. A histopathological study of the nature of the epithelium surrounding implant posts. Part I. J Oral Implantol 1972;3:105-22. 
|
| 43. | James R. A histopathological study of the nature of the epithelium surrounding implant posts. II. Oral Implantol 1973:3:137-59. 
|
| 44. | Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent 1983;50:399-410. 
|
| 45. | Brånemark PI, Zarb GA, Albrektsson T, editors. Tissue integrated prostheses. osseointegration in clinical dentistry. Carol Stream, IL: Quintessence Publishing; 1985. 
|
| 46. | Beaty K. The role of screws in implant systems. Int J Oral Maxillofac Implants 1994;9(Spec Suppl):52-4. 
|
| 47. | Binon PP. Evaluation of machining accuracy and consistency of selected implants, standard abutments, and laboratory analogs. Int J Prosthodont 1995;8:162-78. 
[PUBMED] |
| 48. | Kallus T, Bessing C. Loose gold screws frequently occur in full-arch fixed prostheses supported by osseointegrated implants after 5 years. Int J Oral Maxillofac Implants 1994;9:169-78. 
[PUBMED] |
| 49. | Jansen VK, Conrads G, Richter EJ. Microbial leakage and marginal fit of the implant-abutment interface. Int J Oral Maxillofac Implants 1997;12:527-40. 
[PUBMED] |
| 50. | Jemt T, Pettersson P. A 3-year follow-up study on single implant treatment. J Dent 1993;21:203-8. 
[PUBMED] |
| 51. | Niznick GA. The Core-Vent implant system. Oral Health 1983;73:13-7. 
[PUBMED] |
| 52. | Niznick G. The implant abutment connection: The key to prosthetic success. Compendium 1991;12:932, 934-8. 
|
| 53. | Binon PP. The evolution and evaluation of two interference-fit implant interfaces. Postgraduate Dent 1996;3:3-13. 
|
| 54. | Norton MR. In vitro evaluation of the strength of the conical implant-to-abutment joint in two commercially available implant systems. J Prosthet Dent 2000;83:567-71. 
[PUBMED] |
| 55. | Mollersten L, Lockowandt P, Linden LA. Comparison of strength and failure mode of seven implant systems: An in vitro test. J Prosthet Dent 1997;78:582-91. 
|
| 56. | Sutter F, Weber HP, Sorenson J, Belser U. The new restorative concept of the ITI dental implant system: Design and engineering. Int J Perio Rest Dent 1993;13:409-31. 
|
| 57. | Arvidson K, Bystedt H, Ericsson I. Histometric and ultrastructural studies of tissues surrounding Astra dental implants in dogs. Int J Oral Maxillofac Implants 1990;5:127-34. 
[PUBMED] |
| 58. | Perriard J, Wiskott WA, Mellal A, Scherrer SS, Botsis J, Belser UC. Fatigue resistance of ITI implant-abutment connectors: A comparison of the standard cone with a novel internally keyed design. Clin Oral Implants Res 2002;13:542-9. 
[PUBMED] |
| 59. | Merz BR, Hunenbart S, Belser UC. Mechanics of the implant-abutment connection: An 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants 2000;15:519-26. 
[PUBMED] |
| 60. | Mehl A, Hickel R. Current state of development and perspectives of machine-based production methods for dental restorations. Int J Comput Dent 1999;2:9-35. 
[PUBMED] |
| 61. | Preston JD, Duret F. CAD/CAM in dentistry. Oral Health 1997;87:17-20, 23-4, 26-7. 
|
| 62. | Rekow ED. CAD/CAM in dentistry: A historical perspective and view of the future. J Can Dent Assoc 1992;58:283, 287-8. 
|
| 63. | Vigolo P, Majzoub Z, Cordioli G. Measurement of the dimensions and abutment rotational freedom of gold-machined 3i UCLA-type abutments in the as-received condition, after casting with a noble metal alloy and porcelain firing. J Prosthet Dent 2000;84:548-53. 
[PUBMED] |
| 64. | Wee AG, Aquilino SA, Schneider RL. Strategies to achieve fit in implant prosthodontics: A review of the literature. Int J Prosthodont 1999;12:167-78. 
[PUBMED] |
| 65. | Robson JA. The future of a dentist's lab support. ADA News 2004;35:4. 
|
| 66. | Osorio J. Use of the Atlantis Abutment in restorative practice speeds time to function and aesthetics. Dent Implantol Update 2000;11:57-62. 
[PUBMED] |
| 67. | Kerstein RB, Castellucci F, Osorio J. Ideal gingival form with computer-generated permanent healing abutments. Compend Contin Educ Dent 2000;21:793-7, 800-1. 
[PUBMED] |
| 68. | Kerstein RB, Osorio J. Utilizing computer-generated duplicate titanium custom abutments to facilitate intraoral and laboratory implant prosthesis fabrication. Pract Proced Aesthet Dent 2003;15:311-4. 
[PUBMED] |
| 69. | Ganz SD. Computer-milled patient-specific abutments: Incredible quality with unprecedented simplicity. Pract Proced Aesthet Dent 2003;15(Suppl 8):37-44. 
|
| 70. | Andersson M, Oden A. A new all-ceramic crown. A dense-sintered, high-purity alumina coping with porcelain. Acta Odontol Scand 1993;51:59-64. 
|
| 71. | Van Dooren E. Restoring implants with Procera technology and optimal tissue management. Pract Proced Aesthet Dent 2003;15:23. 
|
| 72. | Lovgren R, Andersson B, Bergovist S, Carlsson GE, Ekström PF, Odman P, et al. Clinical evaluation of ceramic veneered titanium restorations according to the Procera technique. Swed Dent J 1997;21:1-10. 
|
| 73. | Sulaiman F, Chai J, Jameson LM, Wozniak WT. A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont 1997;10:478-84. 
[PUBMED] |
| 74. | Lang LA, Sierraalta M, Hoffensperger M, Wang RF. Evaluation of the precision of fit between the Procera custom abutment and various implant systems. Int J Oral Maxillofac Implants 2003;18:652-8. 
[PUBMED] |
| 75. | Pautke C, Kolk A, Brokate M, Wehrstedt JC, Kneissl F, Miethke T, et al. Development of novel implant abutments using the shape memory alloy nitinol: Preliminary results. Int J Oral Maxillofac Implants 2009;24:477-83. 
[PUBMED] |
| 76. | Lewis S. An esthetic titanium abutment: Report of a technique. Int J Oral Maxillofac Implants 1991;6:195-201. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10], [Figure 11], [Figure 12], [Figure 13], [Figure 14], [Figure 15], [Figure 16], [Figure 17]
[Table 1], [Table 2]
|