|
 
 |
| CASE REPORT |
|
| Year : 2013 | Volume
: 1
| Issue : 2 | Page : 42-45 |
|
Maxillofacial rehabilitation of nasal bridge and frontal bone defect resulting from squamous cell carcinoma
Anupam Purwar1, Rajeev Gulati2, Amit Singh1, Shally Khanna3
1 Department of Prosthodontics and Maxillofacial Prosthetics, Purvanchal Institute of Dental Sciences, AL-4, Sector-7, GIDA, Gorakhpur, Uttar Pradesh, India
2 Department of Orthodontics, Purvanchal Institute of Dental Sciences, AL-4, Sector-7, GIDA, Gorakhpur, Uttar Pradesh, India
3 Department of Oral Pathology, Purvanchal Institute of Dental Sciences, AL-4, Sector-7, GIDA, Gorakhpur, Uttar Pradesh, India
| Date of Web Publication | 17-Aug-2013 |
Correspondence Address:
Anupam Purwar
Department of Prosthodontics and Maxillofacial Prosthodontics, Purvanchal Institute of Dental Sciences, Gorakhpur - 273 209, Uttar Pradesh
India
 Source of Support: None, Conflict of Interest: None  | Check |
 
Facial defects result from tumor, congenital anomaly and external injury not only leads to serious impairment of function and aesthetics, but also makes the patient psychologically disabled. Prosthetic rehabilitation attempts to restore these facial disfigurements may improve aesthetic, level of function, quality of life. This clinical report describes to rehabilitate a patient who has undergone removal of nasal bridge and focal area of frontal bone due to infiltration of carcinoma with the aid of maxillofacial silicone prosthesis. In present case, nasal bridge and frontal bone prosthesis was made combined in single epithesis to achieve retention with the help glass spectacles and anatomical undercuts of surgically excised area. Keywords: Facial defects, frontal bone prosthesis, nasal bridge prosthesis
How to cite this article:
Purwar A, Gulati R, Singh A, Khanna S. Maxillofacial rehabilitation of nasal bridge and frontal bone defect resulting from squamous cell carcinoma. Eur J Prosthodont 2013;1:42-5 |
How to cite this URL:
Purwar A, Gulati R, Singh A, Khanna S. Maxillofacial rehabilitation of nasal bridge and frontal bone defect resulting from squamous cell carcinoma. Eur J Prosthodont [serial online] 2013 [cited 2018 Jul 12];1:42-5. Available from: http://www.eurjprosthodont.org/text.asp?2013/1/2/42/116590 |
| Introduction | |  |
Cancer of head and neck has the potential for producing obvious disfigurement and dysfunction, which may be only partially compensated by prostheses and rehabilitation. [1] Restoration of such facial defects resulting from ablation of facial neoplasms is a challenge for the head and neck surgeon, plastic surgeon, and prosthodontist. [2] Large defect that result from cancer treatment are rarely rehabilitated by surgical reconstruction alone and usually require a facial prosthesis to restore function and appearance. [3] The challenge of restoring such large facial defect has always perplexed the maxillofacial prosthodontist. [4] The advent of silicone rubber has brought us a material that most nearly meets the requirements of the ideal prosthetic material as outlined by Bulbulian. [5] This clinical report describes prosthetic rehabilitation of defects involving nasal bridge and focal area of frontal bone.
| Case Report | |  |
A 62-years-old male patient was referred to the department of maxillofacial prosthodontics, M.S. Ramaiah Dental College and Hospital, Bangalore. He was diagnosed with squamous cell carcinoma of nasal bridge and nasal septum, infiltrated into frontal bone. Patient had undergone removal of nasal bridge including partial nasal septum and focal area of frontal bone followed by radiation therapy with chemotherapy. In this case, reconstructive plastic surgery could be performed as advised by plastic surgeons from M.S. Ramaiah medical college and hospital, Bangalore, but due to unaffordable financial status of patient, surgery did not performed. When we explained the alternative of reconstructive plastic surgery that is maxillofacial silicone prosthesis and its uses in detail, he chose to proceed with the treatment in order to enhance the confidence and quality of life.
Procedure
- Place the patient in the physiological rest position preferably semi-supine position, determined by the operator to make an impression of affected area [Figure 1]
 | Figure 1: Pre-operative showing defect at nasal bridge and focal area of frontal bone
Click here to view |
- The subject was draped with hospital towel. Lubricated the patient's face by light application of petroleum jelly, and deep surgical sites were blocked with a sterile gauge piece to prevent flow of impression material
- Impression of affected area was made with the help of hand mixed irreversible hydrocolloid [Tulip alginate impression material (CAVEX), Holland] with appropriate water powder ratio [Figure 2]. The impression was poured into a Type IV gypsum product (Ultrarock, type IV dental stone; Kalabhai Karson Ltd., Vikhroli (W), Mumbai, India) to obtained undamaged definite cast for the laboratory phase of prosthesis fabrication
 | Figure 2: Impression of defected area with the help of irreversible hydrocolloid
Click here to view |
- Patient's preoperative photograph was used to carve the wax pattern of prosthesis. Wax pattern was tried and evaluated for its esthetics and marginal adaptation on overlying skin of nasal septum and frontal bone. The edges of wax prosthesis were kept feather edge to ensure marginal adaptation with patient's skin to create natural merged appearance as well as to avoid unnecessary trimming of definite silicone prosthesis
- A final evaluation of complete wax prosthesis was performed with glass spectacle, which was used as a primary retentive device to hold the prosthesis
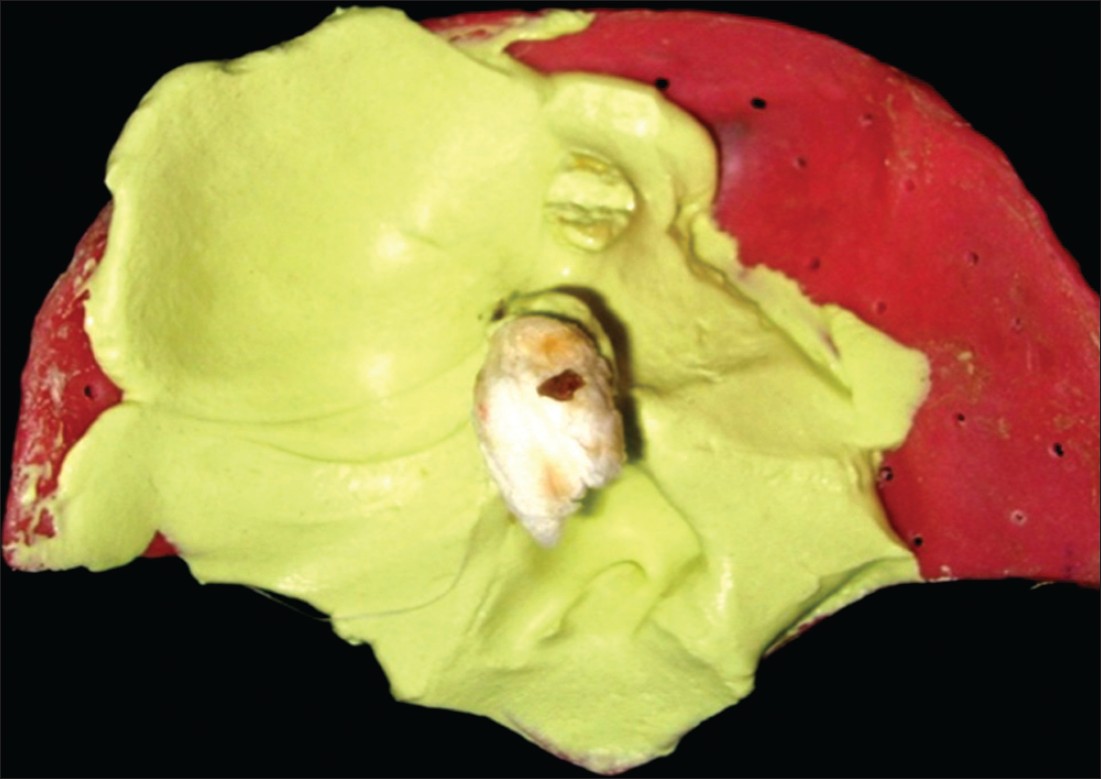
- After consent of patient, flasking of wax pattern was performed [Figure 3] followed by investment in air-free vacuum mixed type IV dental stone (Kalabhai Karson Ltd., Vikhroli (W), Mumbai, India) and de-waxing was carried out. Complete elimination of wax from mold is mandatory for anticipated curing of silicone
- To match the skin shade, base shade had selected, appropriate flocks [Technovent, PM Ltd., Newport, UK], master colors [Technovent, PM Ltd., Newport, UK] etc., were added to achieve the color of localized area of skin. After final shade was achieved, silicone [Maxillofacial Rubber (M511), Technovent, PM Ltd., Newport, UK] was packed in mold under bench press for overnight according to manufacturer's instructions
- After curing of silicone, deflasking, trimming and finishing was carried out
- Fitting of prosthesis was evaluated, and extrinsic coloration was performed to match skin tone of patient [Figure 4]. A thin layer of Vaseline was applied to the feather edges of prosthesis to make it blend with soft tissue. Glass spectacle borne retention was chosen to hold the prosthesis in position [Figure 5]
- Proper care instructions were given to patient, and he was kept under follow up to check the fitting of prosthesis during observation period.
| Discussion | |  |
Vast majority of malignant neoplasms of head and neck exist. Generally, the treatment of choice depends upon the location and extent of the lesion. In present case, due to deep infiltration of carcinoma, a combined approach of surgery followed by post-operative radiotherapy was performed. After surgical excision and radiation therapy, patient was referred to the department of Maxillofacial Prosthodontics for definite silicone prosthesis.
Various maxillofacial impression techniques described so far have been based upon the materials available and the dexterity of the operator, making fabrication of an extraoral facial prosthesis more art than science. [6] The conventional method of making maxillofacial impression involved the use of irreversible hydrocolloid material reinforced with Type II gypsum. [7] Alternatively, high-viscosity polyvinyl silicone impression material [8] was used with the help of a suitable carrier. In our case, we have used the conventional method with a suitable carrier. Impression was made with the help of irreversible hydrocolloid impression material. Use of suitable carrier controls the amount of material; include the heavy bulk of materials that cause tissue distortion. [9]
In this case, retention was achieved by glass spectacle and deep anatomical site of defected area. Today, numerous methods of retention for facial prostheses have been described in the literature; they include eyeglasses [10] extensions from the denture that engage tissue undercuts, [1] magnets, [11] adhesives, [11] and osseointegrated implants. [1],[12] Although osseointegrated implant may provide the most reliable prosthesis retention, additional surgeries, expenses, inadequate bone, and prior radiation to the area may contraindicate this type of treatment. [13],[14]
A subjective measurement of patient was evaluated to assess the improvement in quality of life (QOL). Chang et al. proposed a standard questionnaire to evaluate the patient's satisfaction with facial prosthesis. [15] However, QOL can be used to evaluate patient outcome in any treatment [1] and treated as a "subjective multidimensional concept." [16] In the described case, patient explained that retention and overall appearance was fair and satisfactory, wearing and cleaning of prosthesis was comfortable, and there was no problem regarding tissue discomfort. This inferred that patient had overall improvement in QOL during observation period.
| Conclusion | |  |
Treatment of patient with carcinoma requires a multidisciplinary approach of rehabilitation with the help of plastic surgeon and maxillofacial prosthodontist. In this case, maxillofacial rehabilitation of patient with the help of prosthesis viewed as an alternative to reconstructive surgery, but best result could be obtained by multidisciplinary approach of reconstructive surgery and maxillofacial prosthesis.
| References | |  |
| 1. | Beumer J, Curtis TA, Firtill DN. Maxillofacial rehabilitation: Prosthodontic and surgical consideration. St Louis: C V Mosby; 1979. p. 364-71. 
|
| 2. | Ota Y, Ebihara S, Ooyama W, Kishimoto S, Asai M, Saikawa M, et al. A large maxillofacial prosthesis for total mandibular defect: A case report. Jpn J Clin Oncol 1999;29:256-60. 
[PUBMED] |
| 3. | Brignoni R, Dominici JT. An intraoral-extraoral combination prosthesis using an intermediate framework and magnets: A clinical report. J Prosthet Dent 2001;85:7-11. 
[PUBMED] |
| 4. | Marunick MT, Harrison R, Beumer J 3 rd . Prosthodontic rehabilitation of midfacial defects. J Prosthet Dent 1985;54: 553-60. 
|
| 5. | Bulbulian AH. Maxillofacial prosthetics: Evolution and practical application in patient rehabilitation. J Prosthet Dent 1965;15:554-69. 
|
| 6. | Vibha S, Anandkrishna GN, Anupam P, Namratha N. Prefabricated stock trays for impression of auricular region. J Indian Prosthodont Soc 2010;10:118-22. 
|
| 7. | Andreas CJ, Haug SP. Facial prosthesis fabrication: Technical aspects. In: Taylor TD, editor. Clinical maxillofacial prosthetics. 1 st ed. Chicago: Quintessence Publishing; 2000. p. 233-44. 
|
| 8. | Alsiyabi AS, Minsley GE. Facial moulage fabrication using a two-stage poly (vinyl siloxane) impression. J Prosthodont 2006;15:195-7. 
[PUBMED] |
| 9. | Shifman A. Clinical applications of visible light-cured resin in maxillofacial prosthetics. Part II: Tray material. J Prosthet Dent 1990;64:695-9. 
[PUBMED] |
| 10. | Pflughoeft FA, Shearer HH. Fabrication of a plastic facial moulage. J Prosthet Dent 1971;25:567-71. 
[PUBMED] |
| 11. | Dumbrigue HB, Fyler A. Minimizing prosthesis movement in a midfacial defect: A clinical report. J Prosthet Dent 1997;78:341-5. 
[PUBMED] |
| 12. | Menneking H, Klein M, Hell B, Bier J. Prosthetic restoration of nasal defects: Indications for two different osseointegrated implant systems. J Facial Somato Prosthet 1998;4:29-33. 
|
| 13. | Arcuri MR, LaVelle WE, Fyler E, Jons R. Prosthetic complications of extraoral implants. J Prosthet Dent 1993;69:289-92. 
[PUBMED] |
| 14. | Roumanas E, Nishimura R, Beumer J III, Moy P, Weinlander M, Lorant J. Craniofacial defects and osseointegrated implants: Six-year follow-up report on the success rates of craniofacial implants at UCLA. Int J Oral Maxillofac Implants 1994;9:579-85. 
|
| 15. | Chang TL, Garrett N, Roumanas E, Beumer J III. Treatment satisfaction with facial prosthesis. J Prosthet Dent 2005;94:275-80. 
|
| 16. | Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: Development and validation of the general measure. J Clin Oncol 1993;11:570-9. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|