|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 1
| Issue : 3 | Page : 56-60 |
|
Flexural properties of polyamide versus injection-molded polymethylmethacrylate denture base materials
Shivani Kohli1, Shekhar Bhatia2, Shivani Kohli1, Shekhar Bhatia2
1 Department of Prosthodontics, MAHSA University, Kuala lumpur, Malaysia
2 Department of Conservative Dentistry and Endodontics, MAHSA University, Kuala lumpur, Malaysia
| Date of Web Publication | 14-Oct-2013 |
Correspondence Address:
Shivani Kohli
19A-4-4, BangsarPermai, JalanTandok, Bangsar 59100, Kuala lumpur
Malaysia
Shivani Kohli
19A-4-4, BangsarPermai, JalanTandok, Bangsar 59100, Kuala lumpur
Malaysia
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.119792

Although polymethylmethacrylate is the most commonly used denture base resin, its limitation of compromised flexibility has promoted the use of nylon-based denture resins. Aims: The purpose of this study is to evaluate and compare flexural strength and flexural modulus of two commercially available nylon-based flexible denture base materials, Valplast and Lucitone FRS, and injection-molded SR Ivocap polymethylmethacrylate denture base resin. Materials and Methods: A total of 15 samples of each group (Group A, B, C [Valplast, Lucitone FRS, SR Ivocap]) were prepared. All the samples were subjected to three-point bending test on an Instron Universal Testing machine to test their flexural strength and flexural modulus. Results: The results were statistically analyzed using SPSS Version 12. The difference in flexural modulus and flexural strength of all the three groups was statistically significant, P < 0.05. Conclusion: The mean flexural modulus of Valplast was significantly lower than Lucitone FRS, indicating that Valplast is less rigid, more flexible than Lucitone FRS, and hence more useful in conditions where flexibility in denture base is desired. SR Ivocap displayed flexural strength comparable with Lucitone, but less than Valplast. Keywords: Flexural modulus, flexural strength, injection-molded, polyamide, polymethylmethacrylate
How to cite this article:
Kohli S, Bhatia S, Kohli S, Bhatia S. Flexural properties of polyamide versus injection-molded polymethylmethacrylate denture base materials. Eur J Prosthodont 2013;1:56-60 |
How to cite this URL:
Kohli S, Bhatia S, Kohli S, Bhatia S. Flexural properties of polyamide versus injection-molded polymethylmethacrylate denture base materials. Eur J Prosthodont [serial online] 2013 [cited 2018 Jul 12];1:56-60. Available from: http://www.eurjprosthodont.org/text.asp?2013/1/3/56/119792 |
| Introduction | |  |
Polyamide denture base material can be a useful alternative to polymethylmethacrylate (PMMA) [1],[2],[3] in special circumstances where higher flexibility, higher resistance to flexural fatigue, higher impact strength is required, and in cases where patient is allergic to monomer. The improved flexural properties of nylon denture base materials has promoted their usage in conditions like unyielding undercuts, pronounced tuberosities, tori and bulging alveolar ridges. [4],[5],[6] Thus nowadays, polyamide denture base materials are used because of higher flexibility compared to the commonly used poly methyl methacrylate. [7],[8],[9],[10],[11],[12]
Nylon polyamide were developed as a result of classic research of W.H. Carothers and associates of the Du Pont Chemical Co. of America in 1938 [5] and were used for construction of denture bases in 1950s. [6]
An increasing number of products are being marketed as a flexible denture base material. Valplast and Lucitone FRS are two commercially available monomer-free, nylon-based flexible denture base materials. [13] With the progress in technology and understanding of material, improvised nylon polyamides are finding novel applications in fabrication of removable partial dentures, small- to medium-sized complete dentures, occlusal splints, etc. [14],[15]
To date, very few studies have assessed the potential of these improvised flexible nylon materials for denture base construction. This study evaluates and compares clinically significant flexural properties of nylon-based flexible denture base material with injection-molded, high-impact polymethylmethacrylate-based denture polymers.
| Aims of the Study | |  |
The aim of this study is to evaluate and compare flexural modulus and flexural strength of two commercially available nylon-based flexible denture base materials, Valplast and Lucitone FRS, and injection-molded SR Ivocap polymethylmethacrylate denture base resin.
Objectives
- To evaluate flexural modulus and flexural strength of Valplast, Lucitone FRS, and SR Ivocap using a three-point bending test
- To compare flexural properties of Valplast, Lucitone FRS, and SR Ivocap polymethylmethacrylate.
| Materials and Methods | |  |
The materials and methodology used for this study have been described in [Table 1].
Materials
- VALPLAST (Cartridge system) Valplast, Valplast International Corp, USA
- LUCITONE FRS (Cartridge system) Dentsply Trubyte, U.S.A
- SR IVOCAP (Capsule) Ivoclar Vivadent India Pvt. Ltd.
Armamentarium and equipments
- Brass Metal Dies: 64 × 10 × 2.5 mm
- Valplast injection system
- SUCCESS Injection system assembly: (for Lucitone FRS and SR Ivocap samples)
- Universal testing machine (Instron Universal Testing Machine).
Methods
Preparation Of Samples: Eight brass metal dies with dimensions of 64 × 10 × 2.5 mm were fabricated, according to ISO specification 1567. [16],[17]
Preparation of Valplast samples (Group A) using injection molding technique
The flask used was specially designed for injection molding. A thin layer of petroleum jelly was applied over the brass dies which were then invested in the lower part of the dental flask using dental stone. Wax sprues were attached to the metal dies. The space maintainer for the cartridge was secured in place. The counterpart of the flask was positioned over the base part and dental stone was poured in counterpart. After the stone investment was set, the flask was placed in boiling water for 4 to 6 minutes for dewaxing. The flask was then opened and the brass dies and space maintainer were removed.
Valplast is supplied as a single component in a cartridge form. This cartridge was placed in the furnace, which was preheated to a temperature of 287.7°C (550°F) for 11 minutes. The stone moulds were exposed under heat lamps which were uniformly heated for 15 to 20 minutes to a temperature around 80°C. This was done to avoid any premature freezing of the molten nylon as it entered the mould cavity under pressure. The metal injector was placed in position, then together with the cartridge containing melted Valplast; they were placed on to the injection unit. The molten Valplast was then forced into flask using a plunger. The injection molding pressure was maintained at a pressure of 5 bars for 3 minutes and immediately after that, the assembly was removed and disengaged. The dental flask was bench-cooled for 20 minutes before deflasking. The blanks were removed from the moulds and the sprues were removed with a Valplast-specific disc. The surfaces of the specimens were polished as per manufacturer's instructions.
Preparation of Lucitone FRS (Group B) and SR Ivocap (Group C) resin samples using success injection molding technique
For Lucitone FRS samples (Group B)
Lucitone FRS is supplied as a single component in a cartridge form. Lucitone FRS cartridge was placed in the furnace, which was preheated to a temperature of 302° C (575.6° F). The stone moulds were exposed under heat lamps which were uniformly heated for 17 minutes to a temperature between 65 and 70° C. This was done to avoid any premature freezing of the molten nylon as it entered the mould cavity under pressure. The metal injector was placed in position and then the flask was assembled with brackets. Then together with the cartridge containing melted nylon, they were placed on to the SUCCESS injection unit. The injection molding pressure was maintained at a pressure of 5 bars for 1 minute and immediately after that, the assembly was removed and disengaged. The dental flask was bench-cooled for 5 minutes before deflasking. The blanks were removed from the moulds and the sprues were removed with a cut-off disc. The surfaces of the specimens were polished as per manufacturer's instructions.
For SR Ivocap samples (Group C)
The monomer and polymer content within the capsule of SR Ivocap was mixed as per manufacturer instructions and was carried to the flask assembly. The pressure apparatus was placed in position, flask halves were assembled with the help of brackets. The injection process was carried out in an injection unit at a pressure at 6 bars using injection molding system. The flask was kept on bench for 30 minutes followed by curing in the acrylizer. The polymerization time, once the water starts to boil, was exactly 35 minutes. In order to reduce the content of residual monomer below 1%, the material must be polymerized for 90 minutes in boiling water. The flasks were cooled slowly to room temperature and deflasking was done. The blanks were removed from the moulds and the sprues were removed with a cut-off disc. The surfaces of the specimens were polished as per manufacturer's instructions.
Testing of samples
A flexural three-point bending test was carried out in a water bath at 37 o C, on an Instron Universal Testing machine to test the flexural modulus and flexural strength. The dimensions of each specimen were entered into the program for computation. The distance between the two supporting wedges was 50 mm and the crosshead speed was set at 5 mm min -1 . Prior to flexural testing, all the specimens were stored in distilled water at room temperature for 50 hours. [17],[18],[19]
Individual specimens were removed from water bath and placed on supports of the flexural testing device. Valplast specimens were dipped in warm water for 2 to 3 minutes prior to testing, as per manufacturer's instructions. While placing the sample on the testing device, care was taken that the central loading plunger was touching the midline of the sample. The force in Newton was applied perpendicular to the center of specimen strips and the specimen was gradually loaded using universal testing machine at the crosshead speed of 5 mm min -1 . Load and corresponding deflections were recorded for each specimen. Load deflection curve was plotted for each specimen. The samples were loaded until they fractured for SR Ivocap (Group C) samples. Valplast (Group A) and Lucitone FRS (Group B) samples did not fracture, so the load was applied till maximum capacity of the three-point testing device (26 mm of deflection).
The flexural modulus (E) and flexural strength was determined by calibrating the machine and the values automatically computed from the equation:
Flexural modulus was determined by formula:

Where, y = deflection corresponding to load F at a point in a straight line portion of the load deflection curve,
L = length between jigs,
b = width and
d = thickness of specimen.
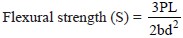
Where, P = load at fracture or maximum load recorded at load deflection curve (i.e., load at maximum deflection)
| Results | |  |
The results were statistically analyzed using SPSS Version 12. One-way ANOVA test of variance and post-hoc Scheffe multiple comparison and range test was applied. Level of significance was set at P < 0.05.
[Table 2] shows the mean flexural modulus, standard deviation, and coefficient of variation of Group A, Group B, and Group C, respectively. The comparison of flexural modulus of three groups was done using one-way ANOVA test of variance [Table 3]. The difference in flexural modulus of all the three groups was statistically significant, P < 0.05.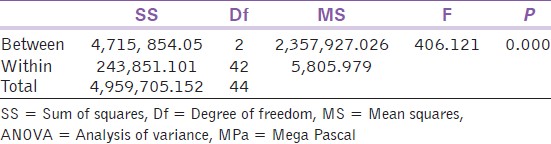 | Table 3: One-way ANOVA analysis-fl exural modulus (MPa) of denture base material
Click here to view |
The comparisons between three groups using post hoc Scheffe multiple comparison and range test revealed that the mean flexural modulus of nylon-based denture materials was higher than injection-molded polymethylmethacrylate. The difference was statistically significant, P < 0.05
The mean flexural modulus of Valplast (Group A) was lower than Lucitone FRS (Group B); hence, the difference was statistically significant, P < 0.05. This indicated that Valplast (Group A) is more flexible than Lucitone FRS (Group B).
[Table 4] shows the mean flexural strength, standard deviation, and coefficient of variation of Group A, Group B, and Group C, respectively. The comparison of flexural strength of three groups was done using one-way ANOVA test of variance [Table 5]. The difference in flexural strength of all the three groups was statistically significant, P < 0.05. The mean flexural strength of Valplast was highest followed by Lucitone FRS and SR Ivocap.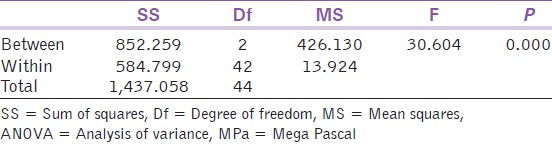 | Table 5: One-way ANOVA analysis-flexural strength (MPa) of denture base material
Click here to view |
| Discussion | |  |
Flexible resins were introduced in the market as an alternative to the use of conventional acrylic resins for the construction of complete and partial removable dentures. [20]
For nylon samples, load deflection curves show a sudden increase in the strain at a particular value of stress and the elongation increases rapidly. This cold drawing behavior is associated with the internal irregularity of nylon. Nylon is a crystalline polymer, whereas polymethylmethacrylate is amorphous. Thus in solid nylon, there is more or less ordered parallel packing of the long-chain molecules which is due to strong attractive forces between the chains. The consequence is a more perfect parallel orientation of the molecules in the direction of elongation, which result in considerable increase in mechanical properties like high flexural modulus, high resistance to shock, i.e., impact and resistance to abrasion. [21]
The load deflection curve of Valplast shows that the strain is directly proportional to flexural stress up to a particular point, beyond which the elongation increases considerably for the same value of stress. But unlike the behavior of Lucitone FRS after this rapid elongation, greater stress was required to produce further elongation. This strain-hardening phenomenon renders the material stronger, harder, and less ductile.
The load deflection curve of SR Ivocap shows that as flexural stress increases, strain increases steadily till the point where specimen fractures.
The mean flexural modulus of nylon-based denture material Lucitone FRS was (1547.9 ± 78.03 MPa). This was consistent with the values obtained by Yunus N et al.[8] (1714.4 ± 152.3 MPa).
The mean flexural modulus of nylon-based denture materials, Valplast, was (1211.09 ± 112.7 MPa). These values were higher than those given by Moore BK et al.[22] (785 ± 74.6) where a 6% maximum strain, low cycle fatigue test was performed in air at 23°C. Hence, the difference in values can be attributed to the different test conditions.
The mean flexural modulus of injection-molded SR Ivocap was (757.8 ± 13.4 MPa), which was in comparison to results obtained by Ucar. [1] The result of this study was in agreement with those of MacGregor et al., [6] Smith DC, [12] and Stafford et al.,[23] where nylon was found to be more flexible than polymethylmethacrylate denture base polymers.
Nylon polyamide is promoted as a denture base material on the basis of its good flexural strength, which allows it to engage certain degree of undercuts for retention. It is usually indicated in certain clinical situations where flexibility is desired like tori, tuberosities, protuberance, extremely bulging alveolar processes, especially in the maxillary anterior (labial) area posing problems of esthetics as well as retention and as an alternative in patients who have sensitivity or allergy to methyl methacrylate monomer. [24],[25],[26],[27],[28],[29]
The mean flexural modulus of Valplast was significantly lower than Lucitone FRS. This indicated that Valplast is less rigid and more flexible than Lucitone FRS, and hence more useful in conditions where flexibility in denture base is desired.
The mean flexural strength of Lucitone FRS was (73.78 ± 2.1 MPa), which is comparatively higher than the values obtained by Yunus N et al.[8] (55.3 ± 3 MPa). The flexural strength of nylon-based denture materials was calculated at maximum deformation, as the samples did not fracture and deflected beyond the capacity of transverse test jig. Matthews E and Smith DC, [5] Hargreaves AS [30] stated that though on straight comparison, the flexural strength of nylon materials is comparable to polymethylmethacrylate, the flexibility of nylon coupled with its strength enables it to resist fracture on constant stressing, i.e., under flexural fatigue.
The mean flexural strength of Lucitone FRS was significantly lower than Valplast. This is explained by the strain hardening phenomenon shown by Valplast. This indicates that Valplast is more resistant to deformation, fracture, or irreversible yield under flexural stress than Lucitone FRS. Though SR Ivocap has flexural strength comparable to Lucitone, its lower flexural modulus limits the amount of rigidity acquired by conventional compression-molded polymethylmethacrylate.
After relating all the data inferred, the results of this study indicate that the Valplast is more flexible than both Lucitone FRS and SR Ivocap. Its flexural strength is higher than Lucitone FRS and SR Ivocap.
However currently, the applications of Valplast flexible denture base material are limited to conditions like unyielding undercuts, tori, tuberosities, proven allergy to polymethylmethacrylate, and small- to medium-sized partial dentures. Hence, it has rising potential as a denture base material to be used in all conditions.
| Conclusion | |  |
Within the limitations of this study, the following conclusions were drawn that the mean flexural modulus of Valplast was significantly lower than Lucitone FRS, thereby indicating that Valplast is less rigid and more flexible than Lucitone FRS. SR Ivocap displayed flexural strength comparable with Lucitone, but less than Valplast.
To substantiate the results of this study, more extensive research with larger sample size, better simulation of oral conditions, and long-term clinical trials are advocated.
| References | |  |
| 1. | Ucar Y, Akova T, Aysan I. Mechanical Properties of Polyamide versus Different PMMA Denture Base Materials. J Prosthodont 2012;21:173-6. 
|
| 2. | Chiang BK. Polymers in the service of prosthetic dentistry. J Dent 1984;12:203-14. 
|
| 3. | Goguta L, Marsavina L, Bratu D, Topala F. Impact strength of acrylic heat curing denture base resin reinforced with E-glass fibers. Timisoara Medical Journal 2006;56:88-92. 
|
| 4. | Peyton FA. History of resins in dentistry. Dent Clin North Am 1975;19:211-22. 
|
| 5. | Mattews E, Smith DC. Nylon as a Denture Base Material. Br Dent J 1955;98:231-7. 
|
| 6. | MacGregor AR, Graham J, Stafford GD, Huggett R. Recent experiences with denture polymers. J Dent 1984;12:146-57. 
|
| 7. | Abuzar MA, Bellur S, Duong N, Kim BB, Lu P, Palfreyman N, et al. Evaluating surface roughness of a polyamide denture base material in comparison with poly (methyl methacrylate). J Oral Sci 2010;52:577-81. 
|
| 8. | Yunus N, Rashid A, Azmi L, Abu-hassan. Some flexural properties of a nylon denture base polymer. J Oral Rehabil 2005;32:65-71. 
|
| 9. | Goiato MC, Panzarini SR, Tomiko C, Luvizuto ER. Temporary flexible immediately removable partial denture: A case report. Dent Today 2008;27:114-6. 
|
| 10. | Meijer GJ, Wolgen PJ. Provisional flexible denture to assist in undisturbed healing of the reconstructed maxilla. J Prosthet Dent 2007;98:327-8. 
|
| 11. | Hamanaka I, Takahashi Y, Shimizu H. Mechanical properties of injection-molded thermoplastic denture base resins. Acta Odontol Scand 2011;69:75-9. 
|
| 12. | Smith DC. Recent developments and prospects in dental polymers. J Prosthet Dent 1962;12:1066-78. 
|
| 13. | Fabian T. Expert opinion of the clinic regarding Valplast prosthesis base plate. Prosthetics Clinic, Hungary: Semmelweis Medical University. 
|
| 14. | Memon MS, Yunus N, Razak AA. Some mechanical properties of a highly cross-linked, microwave-polymerized, injection- molded denture base polymer. Int J Prosthodont 2001;14:214-8. 
|
| 15. | Singh JP, Dhiman RK, Bedi RP, Girish SH. Flexible denture base material: A viable alternative to conventional acrylic denture base material. Contemp Clin Dent 2011;2:313-7. 
[PUBMED]  |
| 16. | International Standard Organization (ISO Specifications 1567): Specifications for denture base polymers. Geneva: Switzerland; 1999. 
|
| 17. | American dental Association (ADA): Specifications for denture base polymer number 12: 2002 (Reaffirmed 2008). 
|
| 18. | Pfeiffer P, Rolleke C, Sheriff L. Flexural strength and moduli of hypoallergic denture base material. J Prosthet Dent 2005;93:372-7. 
|
| 19. | Phoenix RD, Mansueto MA, Ackerman NA, Robert E. Jones evaluation of mechanical and thermal properties of commonly used denture base resins. J Prosthodont 2004;13:17-27. 
|
| 20. | Goiato MC, Santos DM, Haddad MF, Pesqueira AA. Effect of accelerated aging on the microhardness and color stability of flexible resins for dentures. Braz Oral Res 2010;24:114-9. 
|
| 21. | Hargreaves AS. Nylon as a Denture-Base Material. The Dent Prac Dent Rec1971;22:122-8. 
|
| 22. | Moore BK, Platt JA, Oshida Y, Clark H. Mechanical Properties of Four Flexible Denture Base Materials. IADR Abstract Form Washington, DC: 2000. 
|
| 23. | Stafford GD, Huggett R, MacGregor AR, Graham J. The use of nylon as a denture base material. J Dent 1986;14:18-22. 
|
| 24. | Taguchi Y, Shimamura I, Sakurai K. Effect of buccal part designs of polyamide resin partial removable dental prosthesis on retentive force. J Prosthodont Res 2011;55:44-7. 
|
| 25. | Takabayashi Y. Characteristics of denture thermoplastic resins for non-metal clasp dentures. Dent Mater J 2010;29:353-61. 
|
| 26. | Samet N, Tau S, Findler M, Susarla SM, Findler M. Flexible, removable partial denture for a patient with systemic sclerosis (scleroderma) and microstomia: A clinical report and a three-year follow-up. Gen Dent 2007;55:548-51. 
|
| 27. | Lowe LG. Flexible denture flanges for patients exhibiting undercut tuberosities and reduced width of the buccal vestibule: A clinical report. J Prosthet Dent 2004;92:128-31. 
|
| 28. | Zhao X, Cao J, Zhang Y. Clinical application of a kind of flexible gingival epithesis material. Hua Xi Kou Qiang Yi Xue Za Zhi 2003;21:324-6. 
|
| 29. | Anusavice KJ. Denture base resins: Technical considerations and processing techniques. Philips' Science of Dental Materials. 1 st ed, Vol. 1, Philadelphia, PA: W.B. Saunders; 2003. 
|
| 30. | Hargreaves AS. Nylon as a Denture-Base Material. The Dent Prac Dent Rec 1971;22:122-8. 
|
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
|