|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 2
| Issue : 2 | Page : 58-61 |
|
Original research radiological evaluation of marginal bone around dental implants: A pilot study
Anshul Chugh, Shikha Nandal
Department of Prosthodontics and Crown and Bridge and Implantlogy, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Dental Sciences, Rohtak, Haryana, India
| Date of Web Publication | 6-May-2014 |
Correspondence Address:
Anshul Chugh
Uh 7, Medical Campus, Rohtak 124 001, Haryana
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.131980

The use of dental implants has enabled the fabrication of highly functional and aesthetic restorations and improved the predictability of treatment. Standardized periapical radiographs at regular follow-up intervals are used to detect peri-fixtural radiolucency and/or progressive marginal bone loss or 'saucerization' around dental implants and thus to evaluate the success of implant. The aim of this study is to evaluate the early changes in the marginal bone level around dental implants through standard intraoral radiographs in the initial months of implant placement and to evaluate the relationship of various parameters i.e. gender, length and location of implants on amount of bone loss. Keywords: Image analysis, implant, intraoral periapical radiographs, marginal bone loss
How to cite this article:
Chugh A, Nandal S. Original research radiological evaluation of marginal bone around dental implants: A pilot study. Eur J Prosthodont 2014;2:58-61 |
| Introduction | |  |
Pursuit for perfection has always been a main aim of prosthodontist, and proper rehabilitation and restoration of ideal tooth form and function forms its base. The use of dental implants has enabled fabrication of highly functional and aesthetic restorations and has improved the predictability of a treatment. The primary function of a dental implant is to act as an abutment for a prosthetic device, similar to a natural tooth root or crown.
The discovery of osseointegration led to the utilization of tissue-integrated implants, and further biological and biomechanical research led to improvement in the function of titanium implants. [1 ] Natural teeth, prostheses, and implants are dependent on alveolar bone [1],[2 ] and osseointegration forms the basis of implant success. Numerous studies have been conducted to establish the criteria for success and failure of osseointegration and hence for the success and failure of dental implant. One of the first attempts to access osseointegrated dental implants came from the Swedish national board of health and welfare in 1975. [3]
Radiography is a non-invasive technique for determining the alveolar bone quantity and quality. Standardized periapical radiographs at regular follow-up intervals are used to detect peri-fixtural radiolucency and/or progressive marginal bone loss or "saucerization." [4]
The clearly visible threads of implants indicated that the central x-ray beam has been directed perpendicular to the object and film. [5] Alveolar crestal bone loss is one of the most important indices for evaluating implant health, and its loss after implantation is of great significance. If more than half of the bone around the implant is lost, then that implant is considered to have failed. [6 ]
According to the established criteria for the assessment of implant survival and success, marginal bone level change in first year should be less than 1.5 mm. [7 ] Smith and Zarb [8] suggested that one of the criteria for implant success was less than 0.2 mm of alveolar bone loss per year after the first year.
The crestal bone loss is dependent on various parameters like gender, length and width of implants, location of implants, bone density, patient's general health, and patient's habits. [9]
Hence, many authors have stated that the alveolar bone loss is around 1.2 mm during the first year and stabilizes to an average of 0.1 mm per year, [10] but the most active phase of bone loss during the first few months has not been studied extensively. [11]
The aim of this study was to evaluate the early changes in the marginal bone level around dental implants through standard intraoral radiographs in the initial 6 months of implant placement.
| Materials and Methods | |  |
Two subjects requiring replacement of missing teeth were selected from the patients referred to the Department of Prosthodontics, Government Dental College, Rohtak. Patients selected had a good oral hygiene, an adequate bone volume to accommodate an implant of appropriate dimension, and were co-operative and willing for the surgery and proper follow-up. After an explanation of proposed study criteria, including alternate treatment, potential risks, and benefits, the participants were asked to sign consent prior to the surgery. Also, a two-stage surgical procedure for implant placement was performed in both the patients.
An in vivo pilot study was undertaken to evaluate the crestal bone loss on the mesial and distal side of the implant by using standardized intra-oral periapical (IOPA) at the end of 6 months after placing the implants, but before prosthetically loading it. The radiographic evaluation was performed at 0 months (immediately after the implant placement) [Figure 1] and at 6 months after the implant placement [Figure 2]. A customized jig was fabricated for each patient in a modeling wax and having indentations of the teeth adjacent to implant site using the XCP- (extension cone paralleleing) Rinn apparatus[Figure 3], [Figure 4], [Figure 5]. The intraoral radiographs were obtained using a paralleling technique with the aid of XCP-Rinn apparatus and the customized jig to standardize the projection geometry. [12],[13] The radiographs were digitalized using a computerized scanner at 600 dpi, 256 gray scales.
The images were analyzed using the University of Texas Health Science Centre in San Antonio, TX (UTHSCSA, Image Tool (version 3.00 for Windows), after their calibration based on the known implant length [Figure 6]. The top surface of the implant was used as the reference line and the first bone-implant contact was used as the bone level. Perpendicular lines were dropped from the reference line and the bone level on mesial and distal sides of implant and the distance was measured to the nearest 0.01 mm with the UTHSCSA Image Tool [Figure 5]. Subtracting the bone level at 0 months from the bone level at 6 months gave the bone loss in millimeter on mesial and distal aspects of implant 6 months after the implant placement. | Figure 5: The customized jig having indentations of teeth adjacent to implant site
Click here to view |
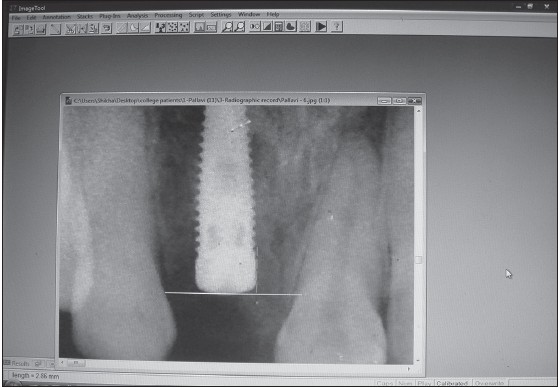 | Figure 6: Measurement of bone level from reference line (top surface of implant) to the bone level (fi rst bone-implant contact) using the UTHSCSA Image Tool (version 3.00 for Windows, University of Texas Health Science Centre in San Antonio, TX)
Click here to view |
| Results | |  |
The marginal bone measurements at 0 and 6 months are illustrated in [Table 1]. The mean marginal bone loss on mesial and distal aspect of implant is illustrated in [Table 2].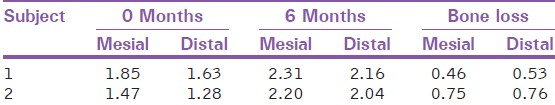 | Table 1: Measurements of marginal bone on mesial and distal aspects of implant
Click here to view |
| Discussion | |  |
Crestal bone loss around dental implants is considered to be one of the major problems and its preservation around implant is the key to long-term success of an implant restoration. [14] The amount of crestal bone lost during the first year of implant service affects the longevity of the implant. Various causes of greater crestal bone loss in the first year of implant function are surgical trauma, occlusal overload, peri-implantitis, presence of microgap, reformation of biologic width, and implant crest module design. [15] This study was undertaken to observe the amount of crestal bone loss, occurring at the end of 6 months after placing the implants, and before loading it prosthetically. [16] According to the established criteria for the assessment of implant survival and success, marginal bone level change in first year should be less than 1.5 mm. [5 ] Smith and Zarb [6 ] suggested that one of the criteria for implant success was less than 0.2 mm of alveolar bone loss per year after the first year.
In this study, the mean crestal bone loss of 0.605 mm on mesial and 0.645 mm on distal is within the success criteria of implant (mean crestal bone loss <1.5 mm in 1 year). [17] Since the study was of 6-month duration, longer follow-up and greater sample size is required for further assessment.
| Conclusion | |  |
A pilot study was undertaken to evaluate the crestal bone loss occurring 6 months after implant placement and before loading it. Two-stage implants were placed in 2 patients. After 6 months, the crestal bone loss on the mesial side and distal side of implant was evaluated by standardized periapical radiographs. The mean crestal bone loss was 0.605 mm on the mesial side of the implant and 0.645 mm on the distal side. More stress should be given on developing implant collar design to reduce the initial crestal bone loss. Although this is only a preliminary study, the results of this study are in concurrence with otherquoted studies. However, because of the limited number of implants placed in this pilot study, the results should be interpreted with caution and further extensive studies are needed to substantiate the data.
| References | |  |
| 1. | Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants in anterior partially edentulous patients. Int J Prosthodont 1993;6:180-8. 
|
| 2. | Bragger U, Hafeli U, Huber B, Hammerle CH, Lang NP. Evaluation of postsurgical crestal bone levels adjacent to non-submerged dental implants. Clin Oral Implants Res 1998;9:218-24. 
|
| 3. | Naert I, Koutsikakis G, Duyck J, Quirynen M, Jacobs R, van Steenberghe D. Biologic outcome of single-implant restorations as tooth replacements: A long-term follow-up study. Clin Implant Dent Relat Res 2000;2:209-18. 
|
| 4. | Penarrocha M, Palomar M, Sanchis JM, Guarinos J, Balaguer J. Radiologic study of marginal bone loss around 108 dental implants and its relationship to smoking, implant location, and morphology. Int J Oral Maxillofac Implants 2004;19:861-7. 
|
| 5. | Siepenkothen T. Clinical performance and radiographic evaluation of a novel single-piece implant in a private practice over a mean of seventeen months. J Prosthet Dent 2007;97:S69-78. 
|
| 6. | Heydenrijk K, Raghoebar GM, Meijer HJ, Stegenga B. Clinical and radiologic evaluation of2-stage IMZ implants placed in a single-stage procedure: 2-year results of a prospective comparative study. Int J Oral Maxillofac Implants 2003;18:424-32. 
|
| 7. | Bryant SR, Zarb GA. Crestal bone loss proximal to oral implants in older and younger adults. J Prosthet Dent 2003;89:589-97. 
|
| 8. | Kwon JY, Kim YS, Kim CW. Assessing changes of peri-implant bone using digital subtraction radiography. J Korean Acad Prosthodont 2001;39:273-80. 
|
| 9. | Schropp L, Kostopoulos L, Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: A prospective clinical study. Int J Oral Maxillofac Implants 2003;18:189-99. 
|
| 10. | Taylor RC, McGlumphy EA, Tatakis DN, Beck FM. Radiographic and clinical evaluation of single-tooth Biolok implant: A 5-year study. Int J Oral Maxillofac Implants 2004;19:849-54.11. 
|
| 11. | Schwartz-Arad D, Herzberg R, Levin L. Evaluation of long term implant success. J Periodontol 2005;76:1623-8. 
|
| 12. | Wakoh M, Harada T, Otonari T, Otonari-Yamamoto M, Ohkubo M, Kousuge Y, et al. Reliability of linear distance measurement for dental implant length with standardized periapical radiographs. Bull Tokyo Dent Coll 2006;47:105-15. 
|
| 13. | Rao W, Benzi R. Single mandibular first molar implants with flapless guided surgery and immediate function: Preliminary clinical and radiographic results of prospective study. J Prosthet Dent 2007;97:S3-14.14. 
|
| 14. | Chung DM, Oh TJ, Lee J, Misch CE, Wang HL. Factors affecting late implant bone loss: A retrospective analysis. Int J Oral Maxillofac Implants 2007;22:117-26.15. 
|
| 15. | Ketabi M, Pilliar R,Deporter D. Factors driving peri-implant crestal bone loss-literature review and discussion: Part 3. J Implant Adv Clin Dent Continuing Educ 2010;1:1-6. 
|
| 16. | Younis L, Taher A, Abu-Hassan MI, Tin O. Evaluation of bone healing following immediate and delayed dental implant placement. J Contemp Dent Pract 2009;10:35-42. 
|
| 17. | 17. Kan JY, Rungcharassaeng K, Liddelow G, Henry P, Goodacre CJ. Periimplant tissue response following immediate provisional restoration of scalloped implants in the esthetic zone: A one-year pilot prospective multicenter study. J Prosthet Dent 2007;97:S109-18. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6]
[Table 1], [Table 2]
|