|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 3
| Issue : 2 | Page : 36-41 |
|
Marginal accuracy of metal copings produced with different ring casting techniques: An in vitro study
Vishal Singh1, Sharad Gupta2, Akshay Bhargava2, Sridevi Kaul2
1 Department of Prosthodontics, Vananchal Dental College and Hospital, Garhwa, Jharkhand, India
2 Department of Prosthodontics, ITS Dental College, Ghaziabad, Uttar Pradesh, India
| Date of Web Publication | 29-May-2015 |
Correspondence Address:
Dr. Vishal Singh
Department of Prosthodontics, Vananchal Dental College and Hospital, Garhwa, Jharkhand
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.157824

Objective: Evaluation and comparison of marginal accuracy of three porcelain fused with metal alloy using ringless and closed ring casting techniques. Materials and Methods: A total of 60 metal copings was fabricated on a metal die. Specimens were divided into two groups (Group I ringless and II ring casting techniques) of 30 patterns each. Groups are further divided into three subgroups of 10 each representing porcelain fused to metal alloys castings namely Mealloy, Wiron-99, and Bellabond plus. The measurement of fit of the metal copings was recorded by stereo photomicroscope at four different surfaces. Results: No significant difference (P < 0.001) was found when the mean vertical marginal integrity at all the buccal, palatal, mesial and distal surfaces among three porcelain fused to metal alloys for both the groups. However on comparing in between group I and group II, it showed that there is significant difference (P > 0.001). The mean of the vertical integrity for the group I (Ringless) was less than group II (Closed Ring). Conclusions: Within the limitations of the study design, it can be concluded that there is a significant difference between ringless and closed ring casting but both are clinically acceptable. Keywords: Dental casting techniques, marginal accuracy, nickel chromium alloy
How to cite this article:
Singh V, Gupta S, Bhargava A, Kaul S. Marginal accuracy of metal copings produced with different ring casting techniques: An in vitro study. Eur J Prosthodont 2015;3:36-41 |
How to cite this URL:
Singh V, Gupta S, Bhargava A, Kaul S. Marginal accuracy of metal copings produced with different ring casting techniques: An in vitro study. Eur J Prosthodont [serial online] 2015 [cited 2018 Aug 27];3:36-41. Available from: http://www.eurjprosthodont.org/text.asp?2015/3/2/36/157824 |
| Introduction | |  |
A good marginal fit is important in dental restoration to fulfill biological, physical and cosmetic requirement. [1] Precise marginal fit is a crucial and critical factor for a successful dental cast restoration. Deficient margins can lead to intraoral degradation of cements that results loss of marginal seal and promotes retention of plaque. Marginal fit of the casting is one factor that can lead directly or indirectly to the development of secondary dental caries, the adverse pulpal reaction, and periodontal disease. [2],[3] Increase in the cost of gold in 1970's shifted the focus on the development of alternative alloy systems. [4] The search for low-cost alloys led to the introduction of noble and predominantly base metal alloys for fixed prosthodontics.
One of the common problems encountered with nonprecious alloys is the casting shrinkage due to the greater thermal contraction from higher solidification temperature. It is essential to achieve compensation for the shrinkage of the solidifying alloy by investment expansion. The use of casting ring (conventional casting technique) was challenged with the introduction of a ringless technique initially for phosphate-bonded investments for removable partial denture frameworks and recently, for conventional fixed restorations and even experimentally for implant-connected frameworks. The high strength of the phosphate bonded investment materials makes it possible to cast without the metal ring. [4]
Phosphate bonded investments were treated with the same techniques as that for gypsum-bonded investments. [5] The metal ring restricts the setting and thermal expansion of the investment, which is necessary to compensate for the shrinkage of the metal on solidification. To overcome this restriction, casting ring liner is used, and a paper cellulose liner was used. The need of a casting ring for phosphate bonded investment was not questioned till now as it was a standard and an established procedure. [4] According to recent studies, the high strength of these investment materials makes it possible to abandon the use of the casting rings. The ringless techniques are easier, less expensive and give clinically acceptable castings. The advantage of a ringless technique is not a restriction of thermal expansion that is associated with the presence of the metal ring. In the literature, there are very few studies to support the assumption that ringless casting technique can produce accurate castings for fixed partial dentures. Thus, this study was undertaken to compare the marginal integrity of metal copings fabricated from three commonly available porcelain fused to metal alloys using Ringless and Closed ring casting techniques.
| Materials and Methods | |  |
Porcelain fused to metal alloys used in this study were Mealloy (Ni - 62%, Cr - 25%, Mo - 9.5% and Si - 3.5%), Wiron-99 (Ni - 65.2%, Cr - 22.5%, Mo - 9.5% and Fe, Si, Mn in traces) and Bella Bond Plus (Ni - 65.2%, Cr - 22.5%, Mo - 9.5% and Fe, Si, Mn in traces) for the fabrication of metal coping. To conduct this study a total of 60 cast coping samples were prepared. The samples were divided into two groups Group I (Ringless casting technique) and Group II (Closed ring casting techniques) having thirty samples each. Based on the type of porcelain fused to metal alloys used (Mealloy, Wiron 99 and Bellabond) the samples of each Group were further categorized into three subgroups having 10 copings viz., subgroup Ia, Ib, Ic and IIa, IIb, IIc.
Preparation of metal die
The stainless steel master die [Figure 1] was machined to simulate the shape and dimension of maxillary first molar preparation. The stainless steel master die served as a control. The metal die consisted of two sections. Upper section simulated the tooth preparation used for the wax pattern preparation and seating of finished copings. The lower section of the master die was a rectangular columnar in shape containing reference lines for measurement of marginal integrity of the copings. The tooth preparation section was made with a vertical dimension of 5 mm from the cavosurface line angle to the occluso-axial line angle. The diameter of the die at the cavo-surface line angle was 10 mm. The shoulder width was 1.2 mm wide with rounded axial-occlusal angles. The convergence angle was 6° per axial wall, resulting in a diameter of 7.6 mm at the occlusal end of the die [Figure 2]. A "V" shaped orientation notch was placed on one surface of the tooth preparation section of the die in the region of finish line for exact positioning of the metal copings for measurements. Each lateral surface of rectangular column of die comprised of two engraved reference markings on the lower section, which were equidistantly placed parallel to long axis of column for the purpose of measurement of marginal accuracy of the copings on either side of the markings.
The above die was precisely positioned in an indigenously machined two-part stainless steel assembly [Figure 3] having a base portion containing the master die and a split top portion having a central opening hole for injecting molten inlay hard wax for the fabrication of wax patterns. A total of 60 wax patterns were fabricated for coping fabrication for the purpose of the study.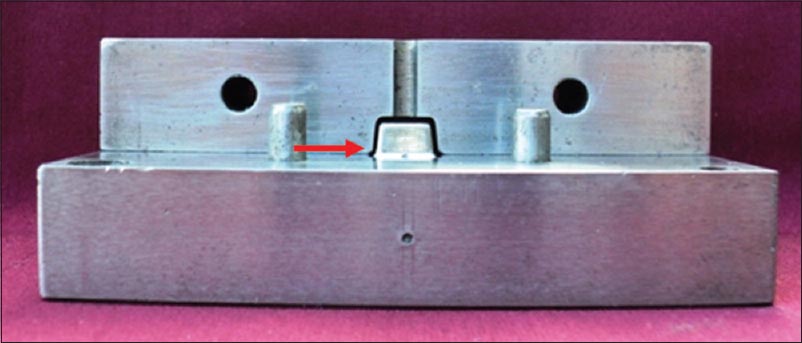 | Figure 3: Machined split assembly containing master die with 0.5 mm space for wax patterns of uniform size (arrow showing the space)
Click here to view |
Wax pattern preparation
Die lubricant (Isocera, Bego, United States) was applied to the Metal Die and machined split assembly so as to facilitate easy removal of the wax patterns before the master die placed in the machined assembly. The molten Inlay wax (Bego-Germany) was put in an electrically controlled wax bath (Bego) and kept at recommended temperature of 160°. The molten inlay wax was injected in the machined assembly. After injecting the molten wax, assembly was allowed to cool to room temperature. The top edge was carved flush with the open end of the machined assembly with a sharp lecron's carver. The split mold assembly was opened and the wax pattern carefully removed from the master die and invested immediately to avoid distortion. To ensure proper marginal adaptation, all margins of the patterns were readapted and redefined using sealing wax.
Spruing and surface treatment of completed wax patterns
Spruing
The wax pattern was separated from the master die by attaching a wax sprue of 3 mm diameter and 6 mm length at the center of the occlusal surface. The sprue attached to the wax pattern was carefully attached to the sprue former so as to allow 6 mm of thickness of investment between pattern and the silicone ring. A wax reservoir measuring 3 mm was positioned between pattern and sprue former. Debbublizer (Aurofilm, Bego Germany) was sprayed on the entire wax pattern to decrease the water repellent effect of wax and decrease the surface tension and to ensure complete coverage of the intricate portion of the patterns by investment material. This allowed for smoother castings with reduced casting nodules and better fit of the casting on the die. 5 wax patterns were invested in the silicone ring at a time [Figure 4].
Investment of the wax pattern
The Group I wax patterns were invested in a silicone ring of 3 cm diameter using Bellasun T phosphate-bonded investment material (Bego, Germany) according to manufacturer's recommendations. After 30 min of initial setting of the investment, the silicone ring was removed before placing in burnout furnace. The Group II wax patterns were invested in a metal ring of 2.5 cm diameter using the Bellasun T phosphate-bonded investment material (Bego, Germany) according to manufacturer's recommendations. A wet casting ring liner of 1 mm uniform thickness (cellulose paper) was placed encircling the inner aspect of the metal ring without any overlap and 3 mm short at both the free ends of metal ring. Powder and liquid were mixed according to manufacturer's instruction.
Mixing and investing
Liquid was put into a clean rubber bowl and then the powder was added. Mixing was done thoroughly with hand spatulation for approximately 10-15 s followed by vacuum mixing for 60 s. Mixed investment was poured in the casting ring with mild vibration, on the vibrator. Excessive vibration was avoided as it would lead to settling of the solids in the investment and allows free water accumulation adjacent to the wax pattern, resulting in surface roughness. Mold was kept 30 min for bench set.
Casting
A two stage programmed burnout process was followed in which the wax patterns were allowed to burnout. The temperature was brought at the 250°C control rate of temperature increase of 5°C/min and held for 30 min. The temperature was then be slowly increased to 950°C at a rate of 7°C/min and held for 1 h.
The casting was carried out in induction casting machine using three different porcelain fused to metal alloy selected for the study. All the castings were done in an induction casting machine (Ducatron series - 3, France) according to the manufacturer's recommendation. After this casting molds were allowed to cool down until warm to the touch.
Divesting
After 1 h of bench cooling the castings were divested, and residual surface investment removed by sandblasting with 50 μm aluminum oxide particles alumina particles in a sandblasting unit (Santer Labo - 16, Ugin, France). Residual surface investment was removed by using 250 μm airborne-alumina particles under 3 bar pressure at a distance of 40 mm from the nozzle tip (2 mm in diameter) in a sandblasting unit. Copings were separated from their respective sprue with carborundum discs. The cast specimens were steam cleaned for 5 s and ultrasonic cleaning were carried out for 10 min before air drying.
After washing, the intaglio surfaces of the castings were inspected for nodules. Castings having >1 internal nodule or with nodules at either site of measurement were rejected. Single nodule of 0.25 um diameter or less were removed with a round bur (0.5") castings with any nodules >0.25 um diameter were rejected. All castings were steam jet cleaned. A total of 60 copings were made [Figure 5].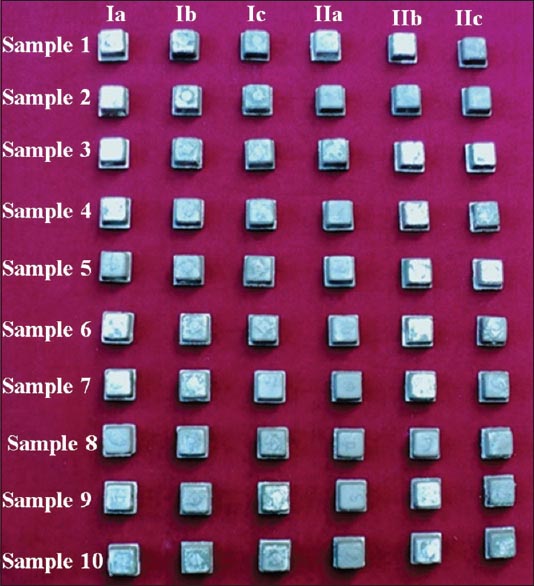 | Figure 5: Samples fabricated after two different casting techniques, that is, ringless and closed ring casting techniques using three different base metal alloys (Mealloy, Wiron 99 and Bellabond plus)
Click here to view |
Testing of sample for marginal integrity
Each coping was seated on the metal die and held by indigenously made holding device for the measurement from the perpendicular view. The holding device tightened up to the marked point in the holding device. The measurement was done with the help of Stereomicroscope (Labomed-Zoomar, Lawrence and Mayo Type - 022545, CA, United States) at magnification of ×80. The measurement was done either side of reference line which is 10 mm and engraved on rectangular columnar portion of die for a total of 4 area per surface. The images were captured and later transformed to the computer; Measurements were done with the help of the Microstructure Analyzer software (TCR World Inc. USA). From one lateral surface 4 readings were taken either side of the reference lines. The mean of each surface were calculated as the final reading for that surface.
| Results | |  |
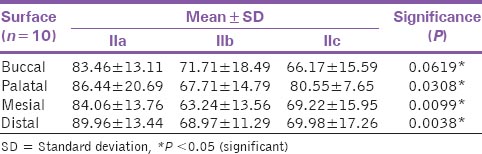
The mean and standard deviation for each group were calculated. One-way ANOVA was performed to identify statistically significant difference between among the different subgroups and groups. It was seen that there is no difference between the different subgroups of the same group as P > 0.001 [Table 1] and [Table 2], but there is highly significant difference between the different group of the same alloy as P < 0.001 [Table 3].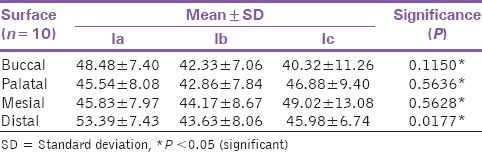 | Table 1: Comparison of vertical marginal integrity between subgroups Ia, Ib and Ic showing the mean SD and their significance values
Click here to view |
 | Table 2: Comparison of vertical marginal integrity between subgroups IIa, IIb and IIc showing the mean SD and their significance values
Click here to view |
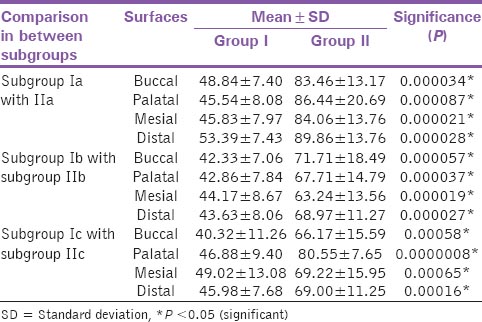 | Table 3: Comparison of vertical marginal integrity in between Group I and Group II showing the mean, SD and their significance values
Click here to view |
| Discussion | |  |
Marginal fit is one of the most important factors for the success of any restoration. [6] Precise fit of the restoration margin to the preparation margin is a necessary condition to prevent gingival inflammation and failure of restoration as it allows less plaque accumulation at marginal area. [7] The marginal accuracy of cast restorations is affected by both clinical as well as laboratory factors like the quality of preparation, undercuts, finish line location, final impression, the working cast, thickness of die spacer, the quality of the wax used for the lost wax technique, appropriate compensation for the casting shrinkage of the alloy used, sprue configuration and design, thickness of casting ring, thickness of ring liner, casting armamentarium used, type of cement and luting pressure applied, surface roughness and irregularities of cast restorations. Since the fit is dependent on so many factors. It is mandatory to follow sound production for fabrication of accurately fit castings. [8],[9]
Ringless casting technique is a commonly used procedure for both conventional fixed prosthodontics and implant prosthodontics, although the metal ring technique is clinically acceptable and it allows for the fabrication of accurate castings. [6] Metal ring restricts the setting and thermal expansion of the investment, which is necessary to compensate for the shrinkage of the metal on solidification. [2],[9],[10] The compensation for the shrinkage inherent in the dental casting procedure may be obtained by either one or both, that is, setting or hygroscopic expansion of the investment and the thermal expansion of the investment. [11]
The use of ringless casting technique has been made possible by the introduction of phosphate bonded investments, which are commonly used for modern day. They can withstand high temperature of castings alloys and do not require a metal ring for protection. [12],[13] The main advantage of these phosphate-bonded investment material is adequacy of investment expansion to compensate for casting shrinkage, ease of casting retrieval from the fired high strength investment, and the of this material ability to obtain complete, nonporous castings which minimizes the casting defects was used. [7] The expansion of the phosphate investment material can be increased by the various factors like increasing the number of layers of asbestos or fibrous ceramic lining the casting ring, increasing the special liquid-water ratio, decreasing the total liquid-water ratio, placing the investment in contact with water during setting and burning out the mold at higher temperature. [14]
In the present study, the marginal discrepancy of copings produced for the ring less casting technique (Group I: Ia-c) [Table 1] was compared. On comparing the marginal discrepancy within the Group I (Ringless casting technique) was observed that there was a statistically insignificant difference for the three different alloys used and a statistically insignificant difference in the values of mean marginal discrepancy was observed for Group I (Ringless casting technique) on the buccal palatal, mesial and distal surfaces. The marginal discrepancy of copings produced by closed ring casting technique (Group II: II-c) [Table 2] was compared. On comparing the marginal discrepancy within group II (ring casting technique) it was observed that there was a statistically insignificant difference for the three different type of alloys used in the study. Similarly a statistically insignificant difference was observed in the values of the mean marginal discrepancy for Group II (Closed ring casting technique) on the buccal, palatal, mesial and distal surfaces.
The results shows that all the three base metal alloys namely Mealloy, Wiron - 99 and Bellabond plus used for the castings of the copings have insignificant marginal discrepancy therefore it can be understood that all the base metal alloys are clinically acceptable for the castings and since the investment material and the casting technique employed is same with the only difference existing in the minor variation in the composition. It appears that the role of the base metal alloys in causing marginal discrepancy is of no consequences and this is mainly due to the fact that all the base metal alloys tested have more or less similar composition. These findings are in agreement with the results contributed by Lombardas et al. in a similar study where they concluded that there was no significant difference in marginal gaps between all the measured sites for a particular investment material and technique. [4]
On comparing the mean vertical marginal discrepancy of copings fabricated by Mealloy (Ia, IIa) at the buccal site between ringless and closed ring casting techniques [Table 3]. For subgroup Ia (Mealloy in Ringless group). It showed there was a statistically high significant difference. Similarly, a statistically high significant difference was also found on the palatal, mesial and distal surfaces.
Similarly on comparing the mean vertical marginal discrepancy of copings fabricated by Wiron- 99 (Ib, IIb) and Bellabond plus at the buccal site between ringless and closed ring casting techniques [Table 3] showed that there was a statistically highly significant difference (P < 0.001). Similarly, a statistically highly significant difference was also found on the palatal, mesial and distal surfaces.
The results indicate that, within the limitations of the study, the castings produced by the ringless casting technique fit better than the castings using the conventional metal ring technique. Studies have shown that casting ring shape, diameter and length affect the accuracy of castings produced because these may influence the expansion of the investment. [3] Although it produces clinically acceptable results, the metal ring restricts the setting and thermal expansion of the investment which is necessary to compensate for the shrinkage of the metal on solidification. To overcome this restriction on expansion, a soft liner is used. There is a lot of controversy regarding the method of use of the ring liner. Few advocates the use of wet liner whereas others advise a dry liner. [15],[16] Mitchell et al. stated that 120 μ represented the maximum clinically acceptable marginal gap. The results of both the groups in the above mentioned study fell into this range. [17] Use of a ring-less system will eliminate all these variables as discussed above and it will be easier to produce more accurate castings. The ring-less technique for investing and casting is based on the premise that the restrictive influence of the metal ring on setting and thermal expansion of mold would be avoided. [16],[18],[19],[20]
In the present study, the vertical marginal accuracy of castings fabricated with ring-less system (Group I) was found to be statistically significantly high (P < 0.001). This can be explained on the ground that in this technique, complete expansion of the mold during setting of the investment occurred uniformly in all directions without any restriction. [21],[22] The setting expansion was also not restricted as the plastic ring was opened up immediately on initial set of the investment Although the conventional casting technique has been the most popular and significantly common technique for both fixed partial denture prosthesis and implant supported prosthesis. [23],[24],[25],[26],[27] The results of this study show that ringless casting technique can be successfully adopted for fabrication of fixed partial denture copings. Further that the alloy types have no influence upon the casting and casting technique used. However further studies using ringless casting technique with a large sample size and different alloy should be carried out for studying the application of the technique to fabricate implant prosthesis.
| Conclusion | |  |
The results of this study substantiate the fact that both the ringless and closed ring cast techniques were clinically acceptable. Thus Ringless Casting Technique can be used for the fabrication of fixed prosthodontic restorations. A comparison of two groups in statistical analysis showed that the marginal accuracy of closed ring castings were inferior to that of the ringless casting techniques. However comparison of subgroups showed significant differences among the porcelain fused to metal alloys at all the surfaces, that is, buccal, palatal, mesial and distal surfaces.
| References | |  |
| 1. | Assif D, Antopolski B, Helft M, Kaffe I. Comparison of methods of clinical evaluation of the marginal fit of complete cast gold crowns. J Prosthet Dent 1985;54:20-4.  [ PUBMED] |
| 2. | Shillingburg HT, Hobo S, Fischer DW. Preparation design and margin distortion in porcelain fused to metal restorations. J Prosthet Dent 1973;29:276-84.  |
| 3. | Ushiwata O, Morae JV, Bottin MA, Silva EG. Marginal fit of nickel-chromium copings before and after internal adjustments with duplicated stone dies and disclosing agent. J Prosthet Dent 2000;83:634-43.  |
| 4. | Lombardas P, Carbunaru A, McAlarney ME, Toothaker RW. Dimensional accuracy of castings produced with ringless and metal ring investment systems. J Prosthet Dent 2000;84:27-31.  |
| 5. | Rudd K, Morrow R, Eissmann H. Dental laboratory procedures. In: Removable partial dentures: Investment, Burn out and Casting. Vol III. St. Louis: CV Mosby; 1981. p. 293-320.  |
| 6. | Sorensen JA. A rationale for comparison of plaque-retaining properties of crown systems. J Prosthet Dent 1989;62:264-9.  |
| 7. | Richter WA, Ueno H. Relationship of crown margin placement to gingival inflammation. J Prosthet Dent 1973;30:156-61.  [ PUBMED] |
| 8. | Shillingburg HT, Jacobi R, Brackett SE. Principles of Tooth Preparations. 3 rd ed. Carol Stream: Qintessence; 1991. p. 119.  |
| 9. | Shiratsuchi H, Komine F, Kakehashi Y, Matsumura H. Influence of finish line design on marginal adaptation of electroformed metal-ceramic crowns. J Prosthet Dent 2006;95:237-42.  |
| 10. | Hung SH, Hung KS, Eick JD, Chappell RP. Marginal fit of porcelain-fused-to-metal and two types of ceramic crown. J Prosthet Dent 1990;63:26-31.  |
| 11. | Anusavice KJ. Phillip's Science of Dental Materials. 11 th ed. St. Louis: Elsevier; 2003. p. 565.  |
| 12. | Annusavice KJ. Phillip's Science of Dental Materials. 11 th ed. St Louis: Elsevier. 2003. p. 309-19.  |
| 13. | O'brien WJ. Dental Materials and their Selection. 4 th ed. Quintessence Inc. IL, United States: 2002. p. 258-62.  |
| 14. | Rudd KD, Morrow RM, Eissmann HF. Dental Laboratory Procedures in Fixed Partial Denture Investing Procedures. Vol III. St. Louis: Mosby; 1981. p. 150-8.  |
| 15. | Earnshaw R. The effect of casting ring liners on the potential expansion of a gypsum-bonded investment. J Dent Res 1988;67:1366-70.  |
| 16. | Shah R, Singh JP, Kumar M, D′Souza DS. Dimensional accuracy of castings fabricated with ringless and metal ring investment systems for implant supported fixed dental prosthesis: An in-vitro comparative study. Med J Armed Forces India 2011;67:46-51.  |
| 17. | Mitchell CA, Pintado MR, Douglas WH. Nondestructive, in vitro quantification of crown margins. J Prosthet Dent 2001;85:575-84.  |
| 18. | Sinha MR, Thakur B, Gaikwad A, Chaudhari LD, Kulkarni A, Kulkarni H. Relating the marginal fit of the castings to the accuracy of the impressions made from laminated hydrocolloid impression technique: A comparative study. J Contemp Dent Pract 2012;13:167-72.  |
| 19. | Tannamala PK, Azhagarasan NS, Shankar KC. Evaluation of marginal gap of Ni-Cr copings made with conventional and accelerated casting techniques. Indian J Dent Res 2013;24:147-8.  [ PUBMED]  |
| 20. | Bhaskaran E, Azhagarasan NS, Miglani S, Ilango T, Krishna GP, Gajapathi B. Comparative evaluation of marginal and internal gap of Co-Cr copings fabricated from conventional wax pattern, 3D printed resin pattern and DMLS Tech: An in vitro study. J Indian Prosthodont Soc 2013;13:189-95.  |
| 21. | Singh GP, Datta K. Analysis of the marginal gap of complete crowns made by using wet and dry ceramic ring liners: An in vitro study. J Indian Prosthodont Soc 2005;5:152-4.   |
| 22. | Limkangwalmongkol P, Chiche GJ, Blatz MB. Precision of fit of two margin designs for metal-ceramic crowns. J Prosthodont 2007;16:233-7.  |
| 23. | Soriani NC, Leal MB, Paulino SM, Pagnano VO, Bezzon OL. Effect of the use of die spacer on the marginal fit of copings cast in NiCr, NiCrBe and commercially pure titanium. Braz Dent J 2007;18:225-30.  |
| 24. | Akova T, Ucar Y, Tukay A, Balkaya MC, Brantley WA. Comparison of the bond strength of laser-sintered and cast base metal dental alloys to porcelain. Dent Mater 2008;24:1400-4.  |
| 25. | Beuer F, Aggstaller H, Richter J, Edelhoff D, Gernet W. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int 2009;40:243-50.  |
| 26. | Quante K, Ludwig K, Kern M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent Mater 2008;24:1311-5.  |
| 27. | Abou Tara M, Eschbach S, Bohlsen F, Kern M. Clinical outcome of metal-ceramic crowns fabricated with laser-sintering technology. Int J Prosthodont 2011;24:46-8.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
[Table 1], [Table 2], [Table 3]
|