|
 
 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 3
| Issue : 3 | Page : 80-84 |
|
The use of oral appliances in two patients diagnosed with different stages of obstructive sleep apnea
Eda Ozdere1, Gulsum Sayin2, Yener Okutan1
1 Department of Prosthetic Dentistry, Selcuk University, Konya, Turkey
2 Department of Prosthetic Dentistry, Medipol University, Istanbul, Turkey
| Date of Web Publication | 29-Sep-2015 |
Correspondence Address:
Dr. Eda Ozdere
Department of Prosthetic Dentistry, Selcuk University, Faculty of Dentistry, Department of Prosthodontics, Konya
Turkey
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.166186

Obstructive sleep apnea (OSA) is a common, chronic disorder of sleep, and breathing that causes disability from pathologic sleepiness, respiratory, and cardiovascular complications. Oral appliance therapy is an alternative in the treatment of OSA, especially in mild and moderate cases. The aim of this report was to assess the effectiveness of custom-made mandibular advancement devices (MAD) and analyze the change in sleep quality and polysomnographic variables in patients diagnosed as having severe OSA and primary snoring. In the present report, two custom-made MADs were produced for two patients who were diagnosed as having severe sleep apnea and primary snoring, according to polysomnographic measurements. The apnea-hypopnea index (AHI) was changed after follow--up period, and complaints were reduced in both patients. MADs are generally indicated for patients with mild to moderate OSA but can be effectively used by severe OSA and primary snoring patients. Keywords: Mandibular advancement device, obstructive sleep apnea, oral appliances
How to cite this article:
Ozdere E, Sayin G, Okutan Y. The use of oral appliances in two patients diagnosed with different stages of obstructive sleep apnea. Eur J Prosthodont 2015;3:80-4 |
How to cite this URL:
Ozdere E, Sayin G, Okutan Y. The use of oral appliances in two patients diagnosed with different stages of obstructive sleep apnea. Eur J Prosthodont [serial online] 2015 [cited 2018 Aug 27];3:80-4. Available from: http://www.eurjprosthodont.org/text.asp?2015/3/3/80/166186 |
| Introduction | |  |
Obstructive sleep apnea (OSA) is a chronic sleep disorder caused by loss of muscle tone and a narrowing of the upper airway during sleep.[1] Snoring is one of the main symptoms of OSA. OSA patients generally complain about snoring, waking up frequently at night, and excessive daytime sleepiness.[2] Untreated sleep apnea can cause neurocognitive impairment, increase the risk of cardiovascular diseases, and motor vehicle accidents.[3]
An increasingly popular treatment method during the last decade is the use of oral appliances (OAs).[4] OAs hold the mandible in a forward and downward position, enlarged the pharyngeal airway space during the sleep.[5] The American Academy of Sleep Medicine reported the indications of OA therapy:[6],[7]
- Patients with mild to moderate OSA who prefer OAs to continuous positive airway pressure (CPAP)
- Patients with severe OSA who refuse CPAP
- Patients who do not respond to CPAP or fail in CPAP therapy, or
- Patients who are not appropriate candidates for CPAP.
Mandibular advancement appliances are the most popular devices used in the treatment of OSA.[8] The aims of the study were to assess the effectiveness of a custom-made mandibular advancement device (MAD) and analyze the change in sleep quality and polysomnographic variables in severe OSA and primary snoring diagnosed patients.
| Case Report | |  |
Two patients were referred to the Selcuk University Department of Prosthodontics with a history of snoring and daytime sleepiness for OA therapy.
The first patient was a 58-year-old man with an AHI score of 38.9, diagnosed as a severe OSA patient. The impressions of upper and lower dental arches were registered using an irreversible hydrocolloid impression material (Kromopan, Lascod, Italy). Intermaxillary relation with 5 mm vertical opening and 70–75% of maximum protrusion was recorded with C-silicone impression material (Zetaplus, Zhermack, Italy) for bite registration. Irreversible hydrocolloid dental impressions were poured with dental stone (Elite Stone, Zhermack, Italy), and plaster models were attached to an articulator (Stratos 100, Ivoclar, Liechteinstein). Custom-made, monoblock OA was produced from thermoplastic night guard (Essix ACE Plastic, Dentsply International, USA) and acrylic material (Paladent, Heraeus Kulzer, Germany) [Figure 1] and [Figure 2]. A ventilation hole was placed in the middle of the appliance to enlarge the airway volume. The adaptation of the appliance and premature contacts were controlled in the patient mouth. The appliance stretched the mandible to approximately 70–75% of the patient maximum protrusive range of movement, measured from the position of maximum intercuspation [Figure 3]. Another polysomnography was performed after 1-month, and the variables were recorded. The patient used his OA with CPAP for 1-month and underwent polysomnography with CPAP. The necessary CPAP titration pressure measured 12 cm H2O, and the AHI score was 3.1 in the polysomnography report. The complaints about daytime sleepiness and snoring were reduced, but the patient refused to use CPAP during the follow-up period because of side effects such as air leaks, abrasions on the ridge of the nose, and dry nose. The patient decided to continue his treatment only with OA therapy. The patient underwent polysomnography with the OA after 6-month follow-up period ended. AHI score was decreased from 38.9 to 28.8 without CPAP therapy after 6-month follow-up period [Table 1]. Apnea and hypopnea durations were also decreased after treatment [Table 2].
The second patient was a 50-year-old woman with an AHI score of 2, diagnosed as a primary snoring patient before the treatment. OA was performed with the same procedure [Figure 4],[Figure 5],[Figure 6] and lateral cephalometric radiograph was taken with and without appliances [Figure 7] and [Figure 8]. CPAP was not indicated for the primary snoring patient. Only an OA was used in the treatment of this patient for 1-month. The AHI score was 0.9 without CPAP due to second polysomnography results [Table 3]. Apnea durations were also decreased after treatment [Table 4]. The patient stated that her complaints were substantially lessened 1-month after the therapy.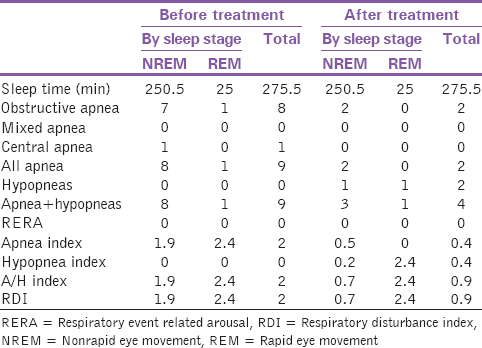 | Table 3: Number of respiratory events-sleep stage (primary snoring patient)
Click here to view |
| Discussion | |  |
OSAs can be classified according to the AHI values: Mild (0–15), moderate (15–30), severe (>30).[9] Based on this classifying the first case was severe and the second was mild OSA patient.
OAs have been reported as an alternative treatment method to surgery and CPAP therapy in patients with OSA. Several studies have investigated the efficiency and success rates of different treatment methods and various design of OAs. In a study, Clark et al. demonstrated that either MAD or CPAP therapy reduced the symptoms of OSA, and found CPAP therapy more effective than OAs, especially in severe patients.[4] In the present study, although after CPAP therapy severe OSA patients AHI index was 3.1, the patient refused to use this treatment after 1-month because of the side effects and difficulties. OA therapy was thus the only treatment option for this patient. For this patient, AHI index decreased from 38.9 to 28.8; shorter apnea and hypopnea durations were observed after treatment. Also, the number of obstructive apnea dropped from 81 to 11.
One month after the treatment, simple snoring patient's apnea index reduced from 2 to 0.9 and average apnea (nonrapid eye movement) duration reduced from 40.9 to 10 s. In addition, a significant reduction was observed at the number of obstructive apnea. Soft palatal lift (SPL) devices can also be preferred for snoring but because of excess gagging and qualm reflex, they are not considered tolerable by patients.[10] Hence, we prefer MAD for this case.
Several investigators have addressed the question of which vertical distance between the upper and lower incisors is acceptable in OA therapy. According to the literature, some authors accepted a 5–7 mm vertical opening as optimal for OAs in the treatment of OSA patients.[11],[12] However, there is no true agreement in this respect. In the present study, we made a 5 mm vertical opening between the incisors. An excessive vertical distance may increase the risk of temporomandibular disorders (TMDs) and other side effects. Various side effects were reported for all treatment modalities of OSA in the literature. There are many studies comparing the dental side effects of OA and CPAP therapy. Doff et al. reported an increased overjet and overbite in the OA group compared to the CPAP therapy group at 2-year follow-up.[3] A study by Ferguson et al. showed that patients in the OA group were more satisfied than those in the CPAP group and had fewer side effects.[13] OAs are simple and easy to use compared to other treatment methods of OSA but may lead to minor side effects such as temporomandibular joint disorders and changes in occlusion. These side effects can occur at any time during the therapy, so the patients treated with OAs must be under control during therapy. In a long-term study, Chen et al. evaluated the side effects of OA therapy and found changes in occlusion.[14] In an another long-term study, the occurrence of TMDs and pain were assessed, and it was documented that pain-related TMDs occurred at the beginning of the OA therapy but returned to normal values during a 2-year follow-up.[15] Our patients reported no side effects during the follow-up period.
Polysomnographic data indicate that our custom-made MAD was helpful in decreasing the AHI score in both severe OSA and simple snoring patients. The AHI score was reduced 26% in severe OSA patient at the end of 6-month follow-up period and 55% in simple snoring patient at the end of 1-month follow-up period. The patients were satisfied with the results after therapy.
| Conclusion | |  |
According to the results of this study, it is concluded that OAs can be an alternative treatment for primary snoring patients, but cannot be as effective as CPAP therapy, especially in patients diagnosed with severe OSA over a long period.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Cistulli PA, Gotsopoulos H, Marklund M, Lowe AA. Treatment of snoring and obstructive sleep apnea with mandibular repositioning appliances. Sleep Med Rev 2004;8:443-57.  |
| 2. | Gerbino G, Bianchi FA, Verzé L, Ramieri G. Soft tissue changes after maxillo-mandibular advancement in OSAS patients: A three-dimensional study. J Craniomaxillofac Surg 2014;42:66-72.  |
| 3. | Doff MH, Finnema KJ, Hoekema A, Wijkstra PJ, de Bont LG, Stegenga B. Long-term oral appliance therapy in obstructive sleep apnea syndrome: A controlled study on dental side effects. Clin Oral Investig 2013;17:475-82.  |
| 4. | Clark GT, Blumenfeld I, Yoffe N, Peled E, Lavie P. A crossover study comparing the efficacy of continuous positive airway pressure with anterior mandibular positioning devices on patients with obstructive sleep apnea. Chest 1996;109:1477-83.  |
| 5. | Seehra J, Sherriff M, Winchester L. Craniofacial characteristics of successful responders to mandibular advancement splint therapy: A pilot study. Br J Oral Maxillofac Surg 2014;52:314-6.  |
| 6. | Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances. American Sleep Disorders Association. Sleep 1995;18:511-3.  |
| 7. | Cistulli PA, Ferguson KA, Lowe AA. Oral appliances for sleep-disordered breathing. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 5 th ed., Ch. 109. Philadelphia: W.B. Saunders; 2011. p. 1266-77.  |
| 8. | Engleman HM, McDonald JP, Graham D, Lello GE, Kingshott RN, Coleman EL, et al. Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: Continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 2002;166:855-9.  |
| 9. | Fukuda T, Tsuiki S, Kobayashi M, Nakayama H, Inoue Y. Selection of response criteria affects the success rate of oral appliance treatment for obstructive sleep apnea. Sleep Med 2014;15:367-70.  |
| 10. | Fairbanks DN, Mickelson SA, Woodsn BT. Snoring and Obstructive Sleep Apnea. 3 rd ed.., Ch. 7. Philadelphia: Lippincott Williams and Wilkins; 2003. p. 79-91.  |
| 11. | Bondemark L, Lindman R. Craniomandibular status and function in patients with habitual snoring and obstructive sleep apnoea after nocturnal treatment with a mandibular advancement splint: A 2-year follow-up. Eur J Orthod 2000;22:53-60.  |
| 12. | Liu Y, Zeng X, Fu M, Huang X, Lowe AA. Effects of a mandibular repositioner on obstructive sleep apnea. Am J Orthod Dentofacial Orthop 2000;118:248-56.  |
| 13. | Ferguson KA, Ono T, Lowe AA, Keenan SP, Fleetham JA. A randomized crossover study of an oral appliance versus nasal-continuous positive airway pressure in the treatment of mild-moderate obstructive sleep apnea. Chest 1996;109:1269-75.  |
| 14. | Chen H, Lowe AA, de Almeida FR, Fleetham JA, Wang B. Three-dimensional computer-assisted study model analysis of long-term oral-appliance wear. Part 2. Side effects of oral appliances in obstructive sleep apnea patients. Am J Orthod Dentofacial Orthop 2008;134:408-17.  |
| 15. | Doff MH, Veldhuis SK, Hoekema A, Slater JJ, Wijkstra PJ, de Bont LG, et al. Long-term oral appliance therapy in obstructive sleep apnea syndrome: A controlled study on temporomandibular side effects. Clin Oral Investig 2012;16:689-97.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8]
[Table 1], [Table 2], [Table 3], [Table 4]
|