|
 
 |
| CASE REPORT |
|
| Year : 2016 | Volume
: 4
| Issue : 2 | Page : 37-40 |
|
Rehabilitation of edentulous maxillary arch with implant-assisted fixed complete prosthesis using multi-unit straight and angulated abutments
Marut Pradipbhai Patel, S Anilkumar, Rajesh Chankramath, Sandhya Gopalakrishnan
Department of Prosthodontics, Government Dental College, Kottayam, Kerala, India
| Date of Web Publication | 14-Sep-2016 |
Correspondence Address:
Dr. Marut Pradipbhai Patel
Department of Prosthodontics, Government Dental College, Kottayam - 686 008, Kerala
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.190610

In comparison to an edentate mandible, rehabilitation of a completely edentulous maxilla using osseointegrated implants has always tested the ability of clinician and laboratory technician. Complex anatomy, as well as the biomechanical limitations of the maxillary bone, resists the placement of implant in its ideal location. This article illustrates a two-stage surgical and prosthetic management of edentulous maxilla opposing natural teeth using seven implants. This case report highlights the advantages of multi-unit straight and angulated abutments, torqued onto the implants, over which a cast titanium framework was made for fabrication of implant-assisted fixed complete dental prosthesis (FP-3 prostheses). Keywords: Edentulous maxilla, hybrid prostheses, multi-unit abutments
How to cite this article:
Patel MP, Anilkumar S, Chankramath R, Gopalakrishnan S. Rehabilitation of edentulous maxillary arch with implant-assisted fixed complete prosthesis using multi-unit straight and angulated abutments. Eur J Prosthodont 2016;4:37-40 |
How to cite this URL:
Patel MP, Anilkumar S, Chankramath R, Gopalakrishnan S. Rehabilitation of edentulous maxillary arch with implant-assisted fixed complete prosthesis using multi-unit straight and angulated abutments. Eur J Prosthodont [serial online] 2016 [cited 2018 Jun 29];4:37-40. Available from: http://www.eurjprosthodont.org/text.asp?2016/4/2/37/190610 |
| Introduction | |  |
The resorptive pattern in maxilla differs from that in the mandible. [1] Maxilla, in the anterior region, resorbs in upward and backward direction, while in the posterior region, it is upward and inward. An overall decrease in the quantity of bone compounded by the presence of nasal fossa in the anterior region and maxillary sinus in the posterior region has demanded more attention for treatment planning with osseointegrated implants in the completely edentulous maxilla. Ideal implant placement in maxilla is more difficult as compared to its mandibular counterpart. [2]
Cone beam computed tomography/cone beam volumetric tomography (CBCT) scan can help clinicians to analyze the labial cortical concavity in lateral incisor region, bone adjacent to nasal fossa and maxillary sinus, paranasal bony buttress in the canine region, and nasopalatine canal three-dimensionally. [3] Accurate measurement of distance, area, and volume could be easily obtained using specific CBCT images. [3],[4],[5] This case report describes an approach for rehabilitation of completely edentulous maxilla by placing seven implants planned using CBCT scan.
Evidence has shown that diverging or converging implant angulations could be managed by multi-unit abutments and abutment level impressions. [6],[7] In this case, multi-unit straight and angulated abutments were screw tightened after aligning them in best possible angulations. FP-3 fixed prosthesis was planned with framework cast in titanium and a wraparound [8] design of hybrid prosthesis.
| Case Report | |  |
A 55-year-old male reported to the Department of Prosthodontics, Government Dental College, Kottayam, Kerala, with a chief complaint of loose upper complete denture and excessive thickness of denture flange in the upper lip region. Patient desired for a fixed treatment option without an anterior flange.
Diagnostic and treatment planning phase
Intraoral clinical examination revealed ovoid edentulous maxillary arch opposed by a full complement of natural dentition. Bilateral labial cortical concavities were present in lateral incisor region. Diagnostic casts articulated using old denture showed edge-to-edge ridge relationship of the maxilla with respect to opposing arch and 15 mm of crown height space.
Based on the interpretations of chief complaint, intraoral examination, mounted diagnostic casts, and CBCT scan (ProMax3DMid ProFace, Planmeca Inc., IL, USA) [Figure 1], a treatment plan was developed to rehabilitate the edentulous maxilla with seven implants and an implant-assisted fixed complete prosthesis.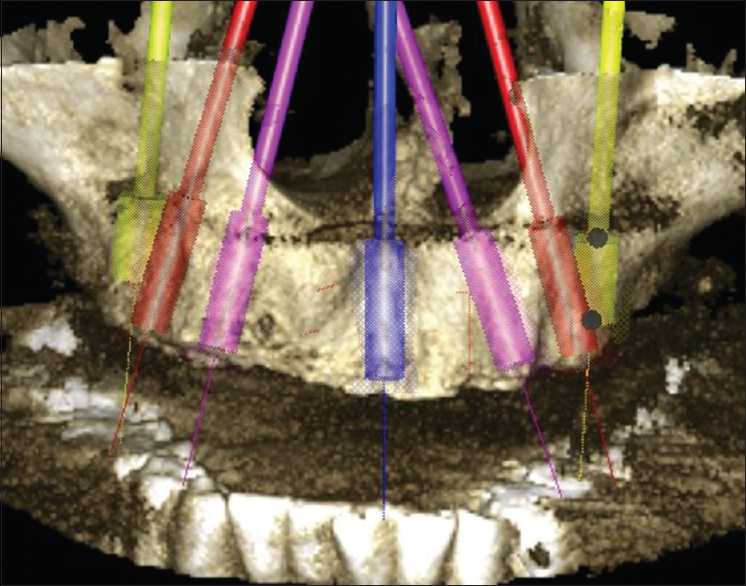 | Figure 1: Three dimensional view of seven virtual implants planned in edentulous maxilla using cone beam computed tomography (ProMax3DMid ProFace, Planmeca Inc., IL, USA)
Click here to view |
Surgical phase
A two-stage surgical protocol was followed. In the first stage, seven implants (Adin Dental Implant System Ltd, Afula, Israel) were placed, one each in canine, premolar, and first molar region, bilaterally, and single implant in central incisor region to counteract the cantilever forces from opposing natural dentition [Figure 2]. The second stage surgery was planned 6 months after the placement of implants. I-shaped incisions were given on each implant site with labial and palatal horizontal incision 0.5-1.0 mm inside the border of implant followed by a vertical incision in the middle of the implant [Figure 3]. Implants were exposed; cover screws were removed, and healing abutment placed without suturing the flap. Complete seating of healing abutments was reassured, radiographically.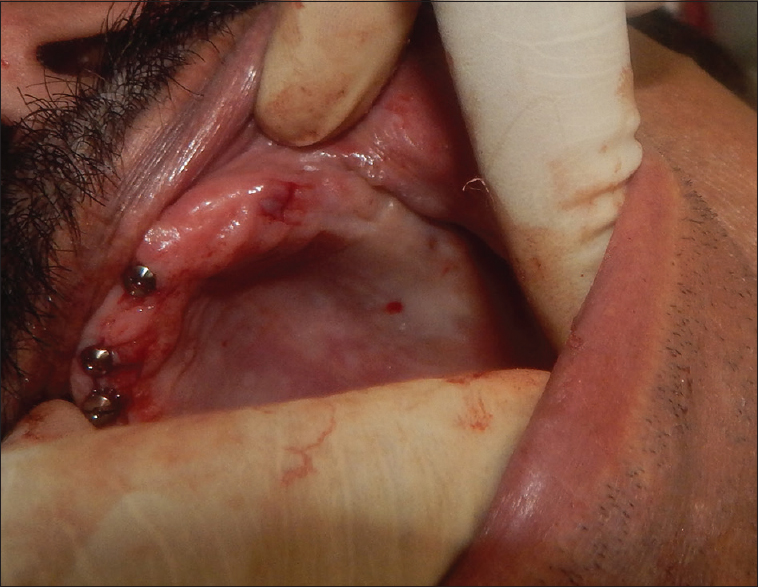 | Figure 3: I-shaped incision to expose the implant cover screw during second stage surgery
Click here to view |
Prosthetic phase
After 2 weeks of healing period, healing abutments were removed. Depending on the amount of correction required in the angulation of implant, three angulated and four straight multi-unit abutments (Transmucosal Abutments, Adin Dental Implant System Ltd, Afula, Israel) were selected. Appropriate direction for each multi-unit abutment was established using abutment holder and torqued to the implants intraorally according to the manufacturer's instruction [Figure 4]. Open tray impression copings (Adin Dental Implant System Ltd, Afula, Israel) specific to multi-unit abutments were placed and tightened with screws.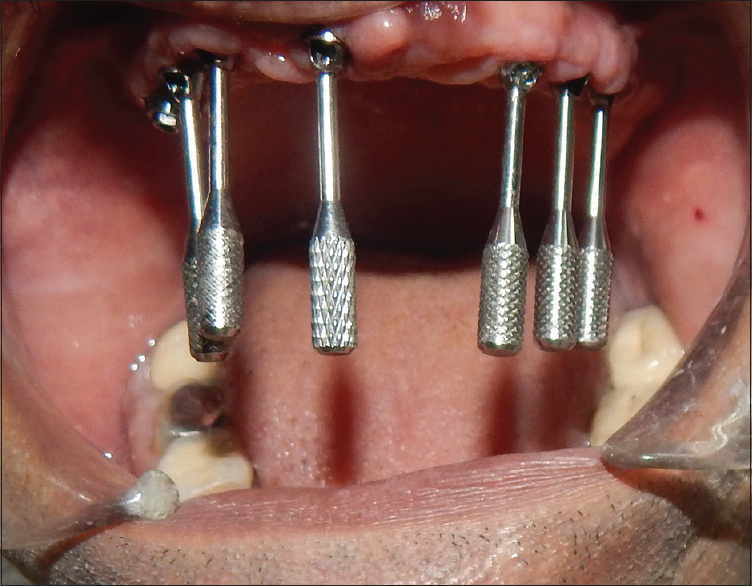 | Figure 4: Abutment holder attached to the multi-unit straight and angulated abutments
Click here to view |
Impression copings were splinted using worn-out dental burs. Burs were sectioned using the metal cutting disk, such that the length of bur was slightly longer than the distance between two impression copings. A hemostat was used to hold the dental bur on the impression copings and fixed with cyanoacrylate adhesive (Fevi Kwik, Pidilite, Mumbai, Maharashtra, India). A small amount of autopolymerizing resin (Pattern resin, GC Corp, Tokyo, Japan) was mixed, applied to the junction of bur and impression coping by brush-bead technique, and allowed to set for 17 min [Figure 5]. An open tray impression was made using medium viscosity addition silicone impression material (Hydrorise Regular Body, Zhermack SpA, Italy). Healing abutments were placed onto the multi-unit abutments. | Figure 5: Open tray impression copings splinted using worn-out dental burs and reinforced with autopolymerizing resin
Click here to view |
After making the master cast, a verification jig was made with pattern resin to confirm the accuracy of an impression. Simultaneously, temporary denture base (Autopolymerizing resin, DPI-RR, Cold Cure TM, DPI, India) was made and secured to two of seven implants using titanium cylinders (Adin Dental Implant System Ltd., Afula, Israel) [Figure 6]. Over the secured denture base, one more denture base was made with an occlusal rim to complete the jaw relation and try in procedures.
Wax-up was performed on the titanium cylinders and a cast titanium framework was fabricated [Figure 7]. The cast titanium framework was tried into the patient's mouth and checked for passivity using Sheffield's one-screw test and screw resistance test. [9] Maxillary denture teeth were waxed with titanium framework and injection molding technique (SR Ivocap High Impact, Ivoclar Vivadent, Schaan, Liechtenstein) was used to complete the processing. The prosthesis was finished, polished, and occlusion refined to achieve an equal intensity of contacts on both sides. An implant-assisted fixed complete prosthesis was screw tightened to the multi-unit abutments with insertion torque of 15 N/cm according to the manufacturer's recommendation. Screw channels were plugged with cotton and filled with autopolymerizing resin (DPI-RR, Cold Cure TM, DPI, India) [Figure 8]. | Figure 8: Implant-assisted fixed complete prosthesis screw tightened and openings sealed with autopolymerizing resin
Click here to view |
| Discussion | |  |
de Albuquerque Júnior et al. [10] have suggested that maxillary implant-assisted fixed/removable treatment should be considered in the patients dissatisfied with conventional dentures, those who desire for fixed dental prostheses or as a prevention to further bone loss. It is justifiable to give more time for proper treatment planning in restoring the edentulous maxilla to normal function, as well as re-establishing esthetics and psychological health of the patient. CBCT scan used in this case helped in placing more number of implants, avoiding encroachment onto important anatomic structures.
Uncovering the implants during the second stage surgery is conventionally done by a midcrestal incision. [11],[12] In this case, I-shaped incisions [13] were given to avoid using sutures, decrease the chair time. Small incision minimized the probability of trauma and inflammatory reaction, thus leading to an uneventful healing. [13]
The use of multi-unit abutments has been shown to influence the accuracy of implant impressions and thus the passive fit of the final superstructure. [14] Limited contact between impression copings and multi-unit abutment decreases the removal stress induced by implant angulations. [15] An effort has been made to describe the management of angulated implants using multi-unit abutments.
The proposition of splint technique of implant impression was based on the principle of connecting the impression copings to achieve an accurate impression. [16] Del'Acqua et al. attributed the accuracy of working cast to metal splinted impression coping technique. [17] This article describes the technique of splinting impression copings using worn-out dental burs. Merits of this technique include rigid splinting with metallic burs, minimal use of autopolymerizing resin to decrease the chance of distortion as a result of polymerization shrinkage, and ease of availability of worn-out dental burs in a clinical setup.
A stable denture base needs to be fabricated over the multi-unit abutments. In this case, titanium cylinders were used to secure the temporary denture base for making accurate jaw relation record and during try-in appointment.
| Conclusion | |  |
In maxillary edentulous arches with complex resorption pattern, it is difficult to place implants parallel to each other. This case describes the management of such implants with multi-unit abutments to restore the maxilla with an implant-assisted fixed complete prosthesis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years, 1972. J Prosthet Dent 2003;89:427-35.  [ PUBMED] |
| 2. | Misch CE. Dental Implant Prosthetics St. Louis: Elsevier Mosby; 2015. p. 615-9.  |
| 3. | Worthington P, Rubenstein J, Hatcher DC. The role of cone-beam computed tomography in the planning and placement of implants. J Am Dent Assoc 2010;141 Suppl 3:19S-24S.  [ PUBMED] |
| 4. | Palomo JM, Kau CH, Palomo LB, Hans MG. Three-dimensional cone beam computerized tomography in dentistry. Dent Today 2006;25:130, 132-5.  |
| 5. | John GP, Joy TE, Mathew J, Kumar VR. Applications of cone beam computed tomography for a prosthodontist. J Indian Prosthodont Soc 2016;16:3-7.  [ PUBMED]  |
| 6. | Carr AB. Comparison of impression techniques for a two-implant 15-degree divergent model. Int J Oral Maxillofac Implants 1992;7:468-75.  [ PUBMED] |
| 7. | Chang WG, Vahidi F, Bae KH, Lim BS. Accuracy of three implant impression techniques with different impression materials and stones. Int J Prosthodont 2012;25:44-7.  [ PUBMED] |
| 8. | Zarb G, Jansson T. Prosthodontic procedures. In: Branemark PI, Zarb G, Albrektsson T, editors. Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago: Quintessence; 1985. p. 250-1.  |
| 9. | Kan JY, Rungcharassaeng K, Bohsali K, Goodacre CJ, Lang BR. Clinical methods for evaluating implant framework fit. J Prosthet Dent 1999;81:7-13.  [ PUBMED] |
| 10. | De Albuquerque Júnior RF, Lund JP, Tang L, Larivée J, de Grandmont P, Gauthier G, et al. Within-subject comparison of maxillary long-bar implant-retained prostheses with and without palatal coverage: Patient-based outcomes. Clin Oral Implants Res 2000;11:555-65.  |
| 11. | Albrektsson T, Zarb G. The Branemark Osseointegrated Implant. Chicago: Quintessence; 1989. p. 117-26.  |
| 12. | Worthington P, Brånemark PI. Advanced Osseointegration Surgery: Applications in the Maxillofacial Region. Chicago: Quintessence; 1992. p. 211-32.  |
| 13. | Lee EK, Herr Y, Kwon YH, Shin SI, Lee DY, Chung JH. I-shaped incisions for papilla reconstruction in second stage implant surgery. J Periodontal Implant Sci 2010;40:139-43.  [ PUBMED] |
| 14. | Baig MR. Multi-unit implant impression accuracy: A review of the literature. Quintessence Int 2014;45:39-51.  [ PUBMED] |
| 15. | Sorrentino R, Gherlone EF, Calesini G, Zarone F. Effect of implant angulation, connection length, and impression material on the dimensional accuracy of implant impressions: An in vitro comparative study. Clin Implant Dent Relat Res 2010;12 Suppl 1:e63-76.  [ PUBMED] |
| 16. | Lee H, So JS, Hochstedler JL, Ercoli C. The accuracy of implant impressions: A systematic review. J Prosthet Dent 2008;100:285-91.  [ PUBMED] |
| 17. | Del'Acqua MA, Chávez AM, Amaral AL, Compagnoni MA, Mollo Fde A Jr. Comparison of impression techniques and materials for an implant-supported prosthesis. Int J Oral Maxillofac Implants 2010;25:771-6.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8]
|