|
 
 |
| CASE REPORT |
|
| Year : 2016 | Volume
: 4
| Issue : 3 | Page : 56-59 |
|
Prosthetic rehabilitation of a patient with orbital defect using silicone prosthesis
Ravindra S Pawar, Pravin E Raipure, Rahul S Kulkarni
Department of Prosthodontics, Nair Hospital Dental College, Mumbai, Maharashtra, India
| Date of Web Publication | 31-May-2017 |
Correspondence Address:
Rahul S Kulkarni
Department of Prosthodontics, Nair Hospital Dental College, Mumbai, Maharashtra
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.207364

Loss of eye, along with contents of the orbit may result from tumor ablative surgery, trauma, or burns, and may negatively affect social and psychological well.being of the patient. Conventional or implant retained orbital prostheses may be indicated, with or without plastic surgical intervention, to restore the appearance of the patient. Orbital prostheses fabricated from silicone, and retained by mechanical means such as spectacles, or adhesives, present an economically viable treatment option for patients who cannot afford implant.retained prostheses. This case report presents a simplified method of fabricating the silicone orbital prosthesis in a young patient with a history of orbital exenteration due to trauma. A. positive reaction was observed in patient's familiar and working surroundings postinsertion of the prosthesis, and the patient could socialize easily after wearing the prosthesis.
Keywords: Orbital exenteration, orbital prosthesis, silicone elastomers
How to cite this article:
Pawar RS, Raipure PE, Kulkarni RS. Prosthetic rehabilitation of a patient with orbital defect using silicone prosthesis. Eur J Prosthodont 2016;4:56-9 |
| Introduction | |  |
Loss of eye, along with contents of the orbit may result from tumor ablative surgery, trauma, or burns, and may negatively affect social and psychological wellbeing of the patient.[1] Conventional or implant retained orbital prostheses may be indicated, with or without plastic surgical intervention, to restore the appearance of the patient. Orbital prostheses fabricated from silicone, and retained by mechanical means such as spectacles, or adhesives, present an economically viable treatment option for patients who cannot afford implant-retained prostheses.[2] This case report presents a simplified method of fabricating the silicone orbital prosthesis in a young patient with a history of orbital exenteration due to trauma. The method described here was found to be cost-effective, easy to perform, and resulted in the restoration of facial esthetics and overall well-being of the patient.
| Case Report | |  |
A 37-year-old male patient presented for treatment with the chief complaint of facial disfigurement due to loss of an eye. History revealed exenteration of the left eye, following facial injury 3 months ago [Figure 1]. Complete healing was observed during clinical evaluation, and mechanical retention could be obtained from tissue undercut. Implant retained prosthesis was ruled out by the patient due to economic constraints, while he consented for silicone orbital prosthesis retained by mechanical undercuts and tissue adhesives.
Technique
- A modified impression tray was prepared using modeling wax (Prime Dental Products, Thane, India), to record an impression of the defect, peripheral tissues, and normal side. Patient was placed in supine position on a dental chair, and petroleum jelly was applied on eye brows and eye lashes for ease of removal of the impression
- A direct impression, was made with irreversible hydrocolloid material (Neocolloid, Bodia Polesine, Italy).[3] The impression material was poured gradually and gently until it covered entire surface, while gauze pieces were placed before its setting so as to provide strength and mechanical retention between alginate and plaster. Fast setting plaster (Caldent, Kalabhai Karson, Mumbai, India) was spread over entire surface to provide strength
- After setting of plaster, impression was removed gently and inspected for voids. Impression was poured in dental stone (Kalrock, Kalabhai Karson, Mumbai, India) to obtain facial moulage. The moulage was duplicated with Agar duplicating material in a metal flask, and a working cast was obtained for fabrication of the prosthesis [Figure 2]
- Wax pattern of orbital prosthesis was fabricated on working cast, and a prefabricated eye conformer (stock ocular prosthesis) was selected as per size and color of the contralateral eye. Wax pattern trial was done [Figure 3]. The position of eye shell was verified to be in accurate anteroposterior, mediolateral, and superioinferior planes in accordance with the contralateral eye [4]
- After wax trial and confirmation of appropriate contour, wax pattern was returned to working cast, and sealed before investing. Sticky wax, in the form of pyramids, was attached to ocular shell to maintain the position of ocular shell in the mold, and petroleum jelly was applied for easy separation of shell from the counter flask [Figure 4]. Flasking was done, and after setting of plaster, deflasking was done carefully so that the ocular shell-sticky wax pyramid could be retrieved without damage [Figure 5]
- The ocular shell-sticky wax assembly was duplicated in die stone with the help of putty index [Figure 6] and [Figure 7]. The duplicated die stone replica was then repositioned in counter flask where index was made by sticky wax pyramid assembly [Figure 8]
- Color matching was done with skin color adjacent to defect area. Silicone material (Factor II) was mixed as per the manufacturer instructions. Intrinsic stains were mixed to achieve shade matching. Packing of silicone was done, and the prosthesis was deflasked following polymerization, and finishing was done. Previously selected stock ocular conformer was fitted in the orbital prosthesis [Figure 9]. Patient's natural hair was used for upper and lower eyelid
- The prosthesis was delivered to the patient. Retention in the prosthesis was primarily obtained through mechanical undercuts of defect, and skin adhesives. A spectacle frame was selected and tried, which could be utilized to conceal the margins of prosthesis and enhance esthetics [Figure 10]
- Instructions were provided regarding prosthesis insertion, removal, maintenance, and hygiene. Follow-up was carried out, and patient satisfaction was noted during periodic recall visits.
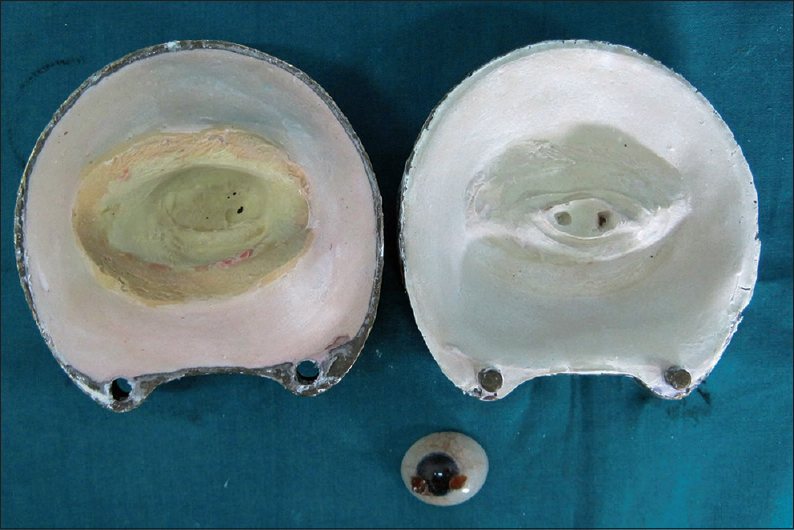 | Figure 5: Investing of wax pattern, wax elimination, and retrieval of conformer with sticky wax pyramids
Click here to view |
 | Figure 7: Formation of die stone replica of conformer-sticky wax assembly
Click here to view |
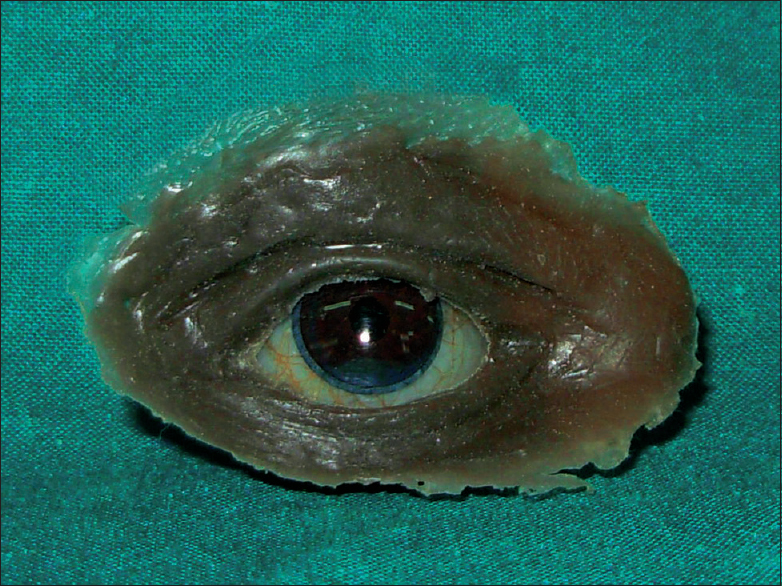 | Figure 9: Final prosthesis. The ocular conformer was inserted in prosthesis after deflasking procedure
Click here to view |
| Discussion and Conclusion | |  |
Retention of an orbital prosthesis depends on the presence of tissue undercuts, use of skin adhesives, and placement of implants. Implant placement was ruled out due to economic limitations, hence, retention would be primarily obtained by mechanical and adhesive means. Spectacles were used to conceal the margins of the prosthesis. Silicone elastomers are widely used to fabricate extraoral maxillofacial prostheses and are favoured due to their lifelike appearance and marginal adaptation. However, color instability is a serious disadvantage of silicones, and prosthesis may be remade every 2 years.[5] A positive reaction was observed in patient's familiar and working surroundings postinsertion of the prosthesis, and the patient could socialize easily after wearing the prosthesis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Dugad JA, Dholam KP, Chougule AT. Vacuum form sheet as a guide for fabrication of orbital prosthesis. J Prosthet Dent 2014;112:390-2.  [ PUBMED] |
| 2. | Veerareddy C, Nair KC, Reddy GR. Simplified technique for orbital prosthesis fabrication: A clinical report. J Prosthodont 2012;21:561-8.  [ PUBMED] |
| 3. | Hanasono MM, Lee JC, Yang JS, Skoracki RJ, Reece GP, Esmaeli B. An algorithmic approach to reconstructive surgery and prosthetic rehabilitation after orbital exenteration. Plast Reconstr Surg 2009;123:98-105.  [ PUBMED] |
| 4. | Padmanabhan TV, Mohamed K, Parameswari D, Nitin SK. Prosthetic rehabilitation of an orbital and facial defect: A clinical report. J Prosthodont 2012;21:200-4.  [ PUBMED] |
| 5. | Kulkarni RS, Nagda SJ. Colour stability of maxillofacial silicone elastomers: A review of the literature. Eur J Prosthodont Restor Dent 2014;22:108-15.  [ PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10]
|