|
 
 |
|
ORIGINAL ARTICLE |
|
|
|
| Year : 2012 | Volume
: 18
| Issue : 1 | Page : 40-42 |
| |
An anthropometric and hematological comparison of sickle cell disease children from rural and urban areas
HS Nikhar1, SU Meshram2, GB Shinde3
1 Department of Microbiology, R.T.M. Nagpur University, L.I.T. Premises, Nagpur, India
2 Department of Microbiology and Rajiv Gandhi Biotechnology Centre, R.T.M. Nagpur University, L.I.T. Premises, Nagpur, India
3 Department of Biochemistry, R.T.M. Nagpur University, L.I.T. Premises, Nagpur, India
| Date of Web Publication | 26-May-2012 |
Correspondence Address:
H S Nikhar
PG Department of Microbiology, R.T.M. Nagpur University, L. I. T. Premises, MG. Marg, Nagpur - 440 033
India
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0971-6866.96643

 Abstract Abstract | | |
Background: Sickle cell disease (SCD) is a prevalent genetic disorder in India and the rural and urban areas experience distinctly different healthcare facilities. In view of this, a comparative study of SCD-SS pattern children of age 8-15 years from rural and urban areas of Wardha district of Central India was carried out using anthropometric and hematological parameters.
Materials and Methods: The data were collected using standard methods and the results showed a significant (P < 0.05) difference in the mean values for body weight, body mass index (BMI), hemoglobin, hematocrit, and white blood corpuscles (WBC). Statistical analysis of the data was done using SPSS 18.0 software. Individuals were screened by solubility test method. Sickle cell patterns (AS and SS) were determined by using electrophoresis technique.
Result : The SCD-SS children from rural were significantly underweight than those from the urban area of Wardha district. BMI is a good indicator of nutritional status and BMI values of SCD children have less than desired.
Conclusion : The study highlights an urgent need to conduct integrated investigations for SCD population of rural areas covering clinical, nutritional, and social aspects.
Keywords: Body mass index, hemoglobin, rural and urban area, sickle cell disease
How to cite this article:
Nikhar H S, Meshram S U, Shinde G B. An anthropometric and hematological comparison of sickle cell disease children from rural and urban areas. Indian J Hum Genet 2012;18:40-2 |
How to cite this URL:
Nikhar H S, Meshram S U, Shinde G B. An anthropometric and hematological comparison of sickle cell disease children from rural and urban areas. Indian J Hum Genet [serial online] 2012 [cited 2016 Jun 1];18:40-2. Available from: http://www.ijhg.com/text.asp?2012/18/1/40/96643 |
 Introduction Introduction | |  |
Sickle cell disease (SCD), a genetic disorder, is prevalent in many areas of India. [1] However, the reported prevalence estimates show an enormous variation (i.e., 0-40%). [2],[3],[4] So far, the initiatives of Indian Government have not shown great results of improving the quality of life of SCD sufferers. The disparity in nutritional intake in rural and urban areas may affect the physical development of SCD children. [5] In this report, we present the results of the comparative assessment of selected anthropometric and hematological parameters of SCD sufferers (SCD-SS) belonging to rural and urban areas of Wardha district of Central India.
 Materials and Methods Materials and Methods | |  |
Following purposive sampling method, 55 and 50 samples (SCD affected SS pattern) from rural and urban areas of Wardha districts were selected for this study. The SCD condition was confirmed by conducting solubility test method, [6] followed by SCD pattern (AS and SS) confirmation using cellulose acetate electrophoresis at pH 8.9. [7] Only SS pattern SCD children of age 8-15 years were selected for this study. The hematological parameters included hemoglobin, red blood corpuscles (RBC), white blood corpuscles (WBC), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) and the anthropometric measurements for height-weight [for body mass index (BMI) determination] were recorded by standard methods. Frame size was determined from height and measuring the breadth of elbow. Statistical analysis of the data was done using SPSS 18.0 software.
 Results and Discussion Results and Discussion | |  |
The results presented in [Table 1] indicate the hematological and anthropometric measurements of SCD (SS pattern) children from rural and urban areas of Wardha district, respectively. The SCD children (from rural and urban areas) exhibited statistically significant (P < 0.05) lower values for all the measurements. The comparative assessment of the hematological and anthropometric parameter values of SCD children belonging to rural and urban areas revealed remarkable difference. Specifically, hemoglobin, hematocrit, RBC, WBC, weight, and BMI parameters showed statistically significant (P < 0.05) difference in the mean values. However, there was no significant difference between SS-SCD children with respect to platelet count, MCV, MCH, MCHC, height mean values, and the frame size for children belonging to both the areas.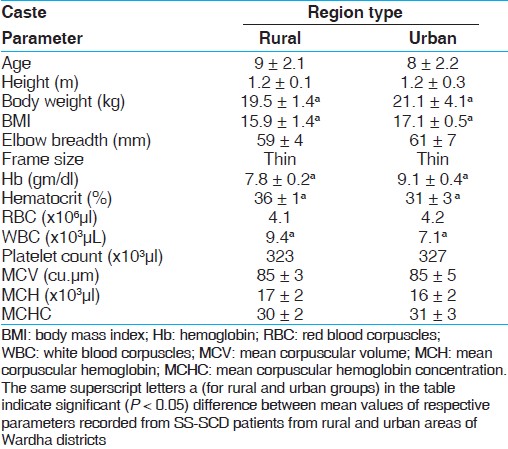 | Table 1: Comparative assessment of the hematological and anthropometric parameters of SS-SCD children belonging to rural and urban areas of Wardha district
Click here to view |
SCD is prevalent in India and often considered to be associated with specific communities. However, the demotechnique growth along with social change in this century is largely responsible for certain changes in the prevalence of SCD. This view can be corroborated with the large number of studies pertaining to prevalence of SCD in different regions as well as communities. [8] Although the SCD is considered to be a clinically benign condition, the past studies show that the pathophysiology is distinctly different than that is observed with the normal people. [9]
In addition to this, most of the studies carried out in India and elsewhere have reported comparison of SCD patients with normal population with respect to various anatomical, hematological, and anthropometric parameters of normal and SCD populations. A reasonable amount of literature [10] has now indicated that the SCD patients experience adverse effect upon the physical growth and development; however, more data are needed, especially from India to confirm this view.
In the backdrop of above information, this study made an attempt to compare the anthropometric and hematological parameters from SS-SCD patients from rural and urban backgrounds. Growth delay starts in early childhood but becomes more apparent during adolescence when the growth spurt of normal children separates them from the patients with SCD. [11] Apparently, the adequate nutritional supplement at young age thus is a prerequisite for relatively less difficult adolescence and higher age. [12] It is in this context, the comparative assessment of rural (compromised nutrition) and urban children with respect to nutrition is critical, which can provide a more clear picture to healthcare professional for delineating therapies (preventive and prophylactic) for SCD patients vis-à-vis various infectious diseases.
It is often considered that anemia plays a critical role in the pathophysiology of SCD. However, to rectify this problem, therapies such as transfusion and nutritional supplements [13] may act effective. In this study, very low Hb levels were associated with the SCD-SS children from rural as well as urban areas of Wardha district and indicated their mean hemoglobin levels to be 7.8 ± 0.2 and 9.1 ± 0.4 g/dl, respectively. From this result, it is evident that SCD-SS children from both the regions need additional nutritional supplements, such as vitamins [folic acid, vitamin B (12), and vitamin B (6)]. However, it is interesting to note that the comparative assessment between SCD-SS indicated that the children from rural area had significantly (P < 0.0.5) lower Hb than those from the urban areas. Similar results were observed with other parameters, such as weight, BMI, hematocrit, and WBC.
Though the physical growth of SCD children could be maintained at normal levels through repeated transfusions, however, this may not be a sustainable therapeutic measure, especially due to transfusion reactions.
The BMI is a good indicator of nutritional status, and the study results indicate that the children from rural as well as urban areas have less than desired, i.e., 18.5. [14] Hence, it would be more fruitful to carry out studies than can pin-point the specific causes for inadequate nutrition and the primary causes associated for under nutrition, which is reflected in low body weight as well as BMI. Although similar results have been reported elsewhere, [15] however, the identification of the cause is not mentioned in the published literature.
In conclusion, this study highlights the need for conducting a more comprehensive study by integrating the clinical, nutritional, and social aspects to determine the cause and effect on relationships between various factors associated with SCD. Besides, a dedicated monitoring programme for assessing hematological parameters of SCD-SS needs to be initiated for effective management. Education for patients with SCD should focus on specific food intake which can increase the nutritional value through various foods.
 Acknowledgement Acknowledgement | |  |
We authors are thankful to PG Department of Microbiology, R.T.M. Nagpur University, Nagpur, India.
 References References | |  |
| 1. | Balgir RS. Phenotypic diversity of sickle cell disorders with special emphasis on public health genetics in India. Curr Sci 2010;98:1096-102. 
|
| 2. | Kamble M, Chaturvedi P. Epidemiology of sickle cell disease in a rural hospital of central India. Indian Pediatrics 2000;37:391-6. 
|
| 3. | Deshmukh P, Garg BS, Garg N, Prajapati NC, Bharambe MS. Prevalence of sickle cell disorders in rural Wardha. Indian J Community Med 2006;31:26-7. 
 |
| 4. | Serjeant GR. The case for dedicated sickle cell centres. Indian J Hum Genet 2006;12:148-51. 
 |
| 5. | Heyman M. Growth retardation in sickle cell disease treated by nutritional support. Lancet 1985;325:903-6. 
|
| 6. | Huntsman RG, Barclay GP, Canning DM, Yawson GI. A rapid whole blood solubility test to differentiate the sickle-cell trait from sickle-cell anaemia. J Clin Pathol 1970;23:781-3. 
[PUBMED] [FULLTEXT] |
| 7. | Rocco RM. Joachim Kohn (1912-1987) and the origin of cellulose acetate electrophoresis. Clin Chem 2005;51:1896-901. 
[PUBMED] [FULLTEXT] |
| 8. | Kate SL, Lingojwar DP. Epidemiology of sickle cell disorder in the state of Maharashtra. Int J Hum Genet 2002;2:161-7. 
|
| 9. | Steinberg MH, Rodgers GP. Pathophysiology of sickle cell disease: Role of cellular and genetic modifiers. Semin Hematol 2001;38:299-306. 
[PUBMED] [FULLTEXT] |
| 10. | Mukherjee MB, Gangakhedkar RR. Physical growth of children with sickle cell disease. Indian J Hum Genet 2004;10:70-2. 
 |
| 11. | Platt OS, Rosenstock W, Espeland MA. Influence of sickle hemoglobinopathies on growth and development. N Engl J Med 1984;311:7-12. 
[PUBMED] [FULLTEXT] |
| 12. | Al-Saqladi AW, Cipolotti R, Fijnvandraat K, Brabin, BJ. Growth and nutritional status of children with homozygous sickle cell disease. Ann Trop Paediatr 2008;28:165-89. 
|
| 13. | Van der Dijs FP, Fokkema MR, Dijck-Brouwer DA, Niessink B, van der Wal TI, Schnog JJ, et al. Optimization of folic acid, vitamin B(12), and vitamin B(6) supplements in pediatric patients with sickle cell disease. Am J Hematol 2002;69:239-46. 
[PUBMED] [FULLTEXT] |
| 14. | WHO Child Growth Standards:Methods and development; Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age. Geneva: World Health Organization; 2006. p. 312. 
|
| 15. | Reed JD, Redding-Lallinger R, Orringer EP. Nutrition and sickle cell disease. Am J Hematol 1987;24:441-55. 
[PUBMED] |
[Table 1]
| This article has been cited by | | 1 |
Somatic Growth and Lung Function in Sickle Cell Disease |
|
| Tina Catanzaro,Anastassios C. Koumbourlis | | Paediatric Respiratory Reviews. 2014; 15(1): 28-32 | | [Pubmed] | [DOI] | | | 2 |
Explaining anthropometric variations in sickle cell disease requires a multidimensional approach |
|
| Mukherjee, M.B. and Ghosh, K. | | Indian Journal of Human Genetics. 2012; 18(1): 1-2 | | [Pubmed] | |
|
 |
|






