|
 
 |
|
ORIGINAL ARTICLE |
|
|
|
| Year : 2013 | Volume
: 19
| Issue : 2 | Page : 136-143 |
| |
Etiology and genetic factors in clefts of lip and/or palate reported at children's hospital, Lahore, Pakistan
Muhammad Yaqoob1, Farrukh Mahmood2, Ghazala Hanif3, Saima Mansoor Bugvi1, Muhammad Afzal Sheikh4
1 Department of Medical Genetics, The Children's Hospital and The Institute of Child Health, Lahore, Pakistan
2 Department of Paediatric Plastic Surgery, The Children's Hospital and The Institute of Child Health, Lahore, Pakistan
3 Department of Histopathology, The Children's Hospital and The Institute of Child Health, Lahore, Pakistan
4 Department of Pediatric Surgery, The Children's Hospital and The Institute of Child Health, Lahore, Pakistan
| Date of Web Publication | 5-Aug-2013 |
Correspondence Address:
Muhammad Yaqoob
Department of Medical Genetics, The Children's Hospital and the Institute of Child Health, Lahore
Pakistan
 Source of Support: None, Conflict of Interest: None  | 8 |
DOI: 10.4103/0971-6866.116103

 Abstract Abstract | | |
The etiology of cleft lip (CL) and/or cleft palate (CP) has been extensively studied in industrialized countries and is suggested to be heterogeneous with increasing evidence that both genetic and environmental factors are operating. To evaluate this assertion in a developing country like Pakistan, a case finding cross-sectional study was completed from 1 st July 2010 to 31 st May 2011 for 100 cases of CL and/or CP referred to the Genetic Clinic of the Children's Hospital, Lahore, Pakistan. A clinical examination followed by necessary diagnostic work-up was completed for each case. The cause of CL and/or CP was clear in 18% of the children ( n = 18). Environmental causes were found in 6 children (four mothers developed hyperthermia during the 2 nd month of gestation, one mother was diabetic, and one mother was a known case of epilepsy and took sodium valproate throughout her pregnancy). Six children were suffering from known genetic malformation syndromes (each with Jarcho-Levin syndrome, Oral-Facial-Digital syndrome type XI, Oral-Duplication syndrome, Kabuki syndrome, Fronto-nasal dysplasia and Nager syndrome). Novel chromosomal aberrations were identified in 2 children. In 82% of the children ( n = 82) the cause of oro-facial clefts remained unknown. Impact of gender and consanguinity on the development of CL and/or CP was also studied. Prevalence of CP was significantly more among female children as compared to that in males ( P < 0.05). Associated anomalies were present in 18% of the cases, anomalies of the craniofacial region being the most common. These findings were compared with regional and international studies.
Keywords: Associated malformations, cleft lip, cleft palate, consanguinity, etiology
How to cite this article:
Yaqoob M, Mahmood F, Hanif G, Bugvi SM, Sheikh MA. Etiology and genetic factors in clefts of lip and/or palate reported at children's hospital, Lahore, Pakistan. Indian J Hum Genet 2013;19:136-43 |
How to cite this URL:
Yaqoob M, Mahmood F, Hanif G, Bugvi SM, Sheikh MA. Etiology and genetic factors in clefts of lip and/or palate reported at children's hospital, Lahore, Pakistan. Indian J Hum Genet [serial online] 2013 [cited 2016 May 24];19:136-43. Available from: http://www.ijhg.com/text.asp?2013/19/2/136/116103 |
 Introduction Introduction | |  |
Oro-facial clefts (OFCs) constitute a group of structural malformations around the oral cavity and can extend on to the face resulting in oral and facial deformities. Within this group the main categories are cleft lip (CL) and cleft palate (CP), occurring together, in isolation, or as part of a spectrum of physical malformations labeled as syndromes, associations, sequences or disruptions. Epidemiological surveys have shown that CL and/or CP (CL/P) are among the most frequently observed birth defects in children. [1]
The etiology of CL/P has been extensively studied in industrialized countries and is heterogeneous with increasing evidence that these anomalies are multifactorial in nature. Although genetic and environmental triggers are important for syndromic CL/P, the aetiology of the more common non-syndromic (isolated) forms remains poorly understood. [2],[3] CP is more common among females while Cleft lip and palate combined (CLP) is more common in males. [4],[5] A recent population based cohort study from Denmark has shown that the concordance rates and heritability estimates for monozygotic twins with CL/P have strong genetic component. [6] Other case finding studies reveal that chromosomal aberrations and single gene mutations are frequently associated with the development of CL/P; single gene mutation being more prevalent than the chromosomal abnormalities. [5]
The environmental factors causing CL/P are diversified. The population based studies have shown that folic acid deficiency in pregnancy has strong association with the development of OFCs in fetus. [7] Teratogenic effect of several drugs such as hydantoin, sodium valproate, trimethadion, tranquilizers, and alcohol is well-known. Children born to mothers suffering from diabetes mellitus or phenylketonuria are at higher risk of developing CL/P. It has also been reported that the development of fever more than 40°C, during the 1 st 8 weeks of gestation has high-risk of causing facial clefts in the developing fetus. [8] Early amniotic rupture can severely disrupt the intrauterine development of the fetus leading to different fetal anomalies including CL or CP or both. [9]
Associated malformations in cases with CL/P are also common. A recent retrospective case finding study from Iran has shown that 13% of children with OFCs had other associated malformations. [4] However, higher frequency of these anomalies (21.8%) is reported in other studies. [5]
Aim of the present investigation was to explore underlying causes of CL/P in a group of children affected with OFCs. Impact of gender and consanguinity on the development of OFCs was also studied. The findings were compared with other regional and international studies.
 Materials and Methods Materials and Methods | |  |
Place of study
The Children's Hospital and the Institute of Child Health, Lahore, is located in the southern part of Lahore city, the capital of the Punjab Province of Pakistan. The Punjab Province is the largest province of this country having population of more than 80 millions. The Children's Hospital is a tertiary health-care center in public sector of Punjab province and is catering patients not only from Punjab but also from other parts of the country.
Study population
From 1 st July 2010 to 31 st May 2011, 100 patients having CL/P were referred for genetic evaluation to the Genetic clinic in the Out-patient Department of the Children's Hospital. Basic demographic information was recorded for each child. Antenatal events such as development of fever, intake of drugs, or any maternal illness that could affect the developing fetus were also recorded.
Methods
After taking oral consent of the parents accompanying the patient, a detail history followed by clinical examination was performed.
Age of the child was ascertained in months and years as told by the parents. A marriage was said to be consanguineous if the parents had at least one ancestor in common. The upper limit of consanguinity was 2½ cousins. A pedigree of the nuclear family was drawn.
Development of each child was assessed in terms of achievement of milestones. If a child was found to be developmentally delayed or had any dysmorphic feature other than CL/P, relevant investigations were requested such as, X-ray skeletal survey, CT scan brain, 3D CT cranium and face, ultrasound abdomen, echocardiogram and chromosomal analysis. All clinical and demographic information was recorded on a structured data form.
Environmental causes were defined as those intrauterine insults that have been clearly shown association with the development of OFCs in the fetus, like intake of anticonvulsant drugs by the mother during 1 st 2 months of gestation, overt diabetes mellitus in the mother. Hyperthermia was taken when there was definite history of developing persistent high grade fever by the mother for at least 3 days during the 1 st 2 months of pregnancy. Syndromes were diagnosed on the basis of constellation of clinical features and relevant investigations. [8]
Children with CL/P were classified into three groups according to anatomical site, i.e., children with CL, children with CP and children having CLP.
Structural and developmental anomalies other than CL/P present in a child were labeled as associated anomalies. These anomalies were subdivided according to anatomical site [Figure 1].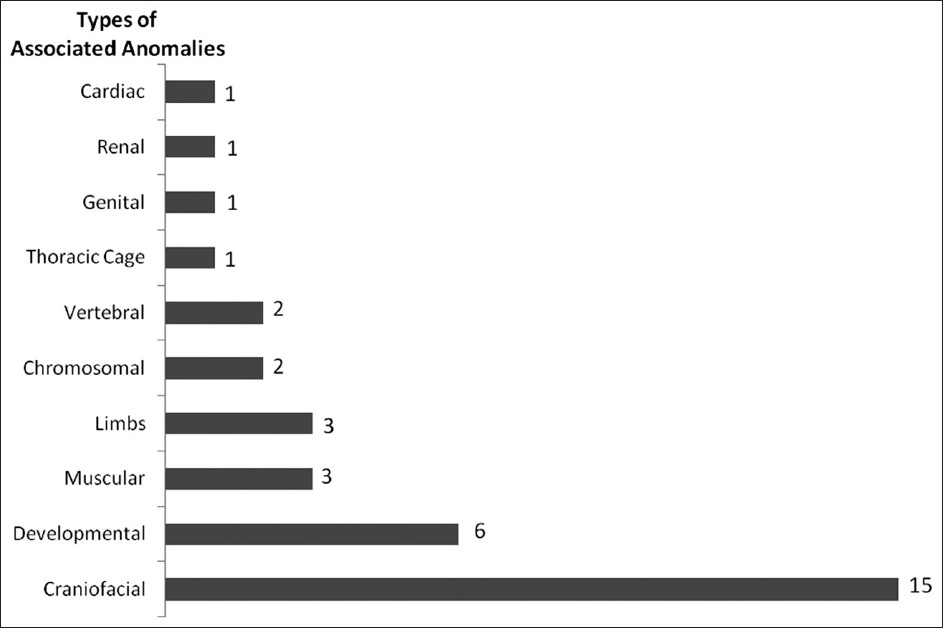 | Figure 1: Associated anomalies in 18 cases with known cause of oro-facial clefts
Click here to view |
Statistical analysis
Frequencies, proportions and means were calculated and tests of significance used were Chi-square and Fisher's exact tests, as appropriate. OFCs were treated categorically in the analysis against independent variables, i.e., gender and consanguinity.
 Results Results | |  |
Among 100 cases with CL/P, 49 were males, and 51 females. Mean age at presentation was 3 years, varying from 3 months to 11 years. Distribution of different categories of OFCs against gender and consanguinity is shown in [Table 1].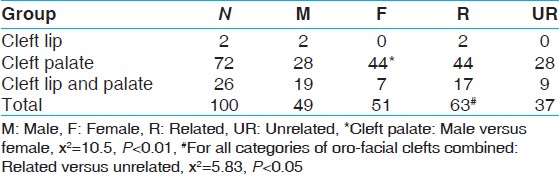 | Table 1: Frequency table showing different categories of oro-facial clefts against gender and consanguinity of the parents
Click here to view |
[Table 1] also shows 72 children having CP. CL alone was present in 2 children. CLP was present in 26 children, out of which 4 children had bilateral CL (3 males and 1 female). Of the 24 cases of unilateral CL (22 had CLP and 2 with isolated CL) 14 had left sided CL (58%).
[Table 1] also presents CP being significantly more common among females as compared to males, while CLP was more common among males but did not reach significant level. However, the effect of gender on the development of OFCs disappeared while all three categories of clefts were combined.
Parents of 63 children were consanguineously married (63%).
Most probable cause of OFCs was known in 18% of the cases (n = 18). In 6 cases the OFCs were due to teratogenic effect of diabetes mellitus, sodium valproate, and hyperthermia in mothers during the pregnancy. In 12 children the cause was genetic. In 82% of the cases (n = 82) the cause of OFCs remained untraceable, [Table 2].
Case reports
Jarcho-Levin syndrome
A 4-year-old male child of related parents showed tilting of trunk towards left side while standing. Trunk was asymmetrical, bulging of upper part of the sternum, right lower ribs prominent, and marked scoliosis. He had flat face, flat occiput, mild synophrys, low set ears, small mouth, CP (operated), short neck, and right undescended testis. Chest X-ray showed marked scoliosis with ribs 1-6 on left side and 1-9 on right side being hypoplastic. There was partial fusion of ribs 8-9 and 11-12 on right side. Renal ultrasound revealed both kidneys enlarged with diffused parenchymal echogenecity of grade I and II with prominent pyramids.
Oral-facial-digital syndrome type XI (Gabrielli type)
A 18-month-old female child presented with CP (operated), short neck and head tilt to right side. She had wide anterior fontanel, dysplastic ears, and prominent antihelix of left pinna, depressed nasal bridge, postaxial polydactyly left foot, and pre-axial polydactyly left hand. X-ray cervical spine showed hypoplastic right cervical vertebrae and X-ray facial bones revealed hypoplasia of right half of mandible.
Oral-duplication syndrome
A 2½-year-old male child presented with CP (operated), and an additional alveolar ridge behind the original one with two central incisors.
Kabuki syndrome
A 2-year-old male child presented with mild hypotonia, CP (operated), prominent ears, bilateral ptosis, developmental delay, and retardation of speech. CT scan brain, ultrasound abdomen, nerve conduction studies, electromyography, chromosomal analysis all were normal.
Frontonasal dysplasia
A 2½-year-old male child presented with CLP (operated), frontal bossing, wide anterior fontanels, hypertelorism, wide nasal tip, wide mouth, short stubby hands, bilateral inguinal hernia, and hypospadias. 3D CT of face and cranium showed wide metopic suture.
Nager syndrome More Details
A 15-month-old male child of related parents presented with CLP (operated), and absent both thumbs. Chromosomal analysis, ultrasound abdomen and CT scan brain were normal.
Chromosomal aberration 46, XY, t (2;17) (q 21;p 12)
An 8-year-old male child first presented to health facility soon after birth as he was having oblique facial cleft on left side of the face and a small lateral cleft extending from right angle of the month. Follow-up record showed normal development except speech. 3D CT of facial region revealed hypoplasia of left maxilla, wide gap between left maxilla, and premaxilla, wide gap between left maxilla, and left nasal bone extending through naso-maxillary suture in to the floor of orbital fossa. He had also CL (left side), CP and deflected nasal septum.
Chromosomal aberration 46, XY, t (12;14) (q13;p11)
An 18-month-old male child of related parents presented with CP (operated) and developmental delay, mild spasticity of upper extremities and severe spasticity of lower extremities with scissoring, normal deep reflexes. Echocardiography showed ventricular septal defect (VSD). CT scan brain was normal.
Associated anomalies
In total 35 additional anomalies were detected in 18 cases with known etiology, an average of 2 anomalies per case. The largest category was that of the craniofacial region (43%) followed by cognitive impairment (17%) and least for cardiac, renal, and genital anomalies (each 3%), [Figure 1].
 Discussion Discussion | |  |
Thorough the clinical evaluations followed by relevant diagnostic investigations have discovered several causes of CL/P in the present study. Presence of 18% of genetic or environmental causes has also been reported in other studies from Europe and Middle East. [5],[10] This establishment of etiology of these OFCs is important in determining the prognosis, nature and extent of service needed to support affected children. To the author's knowledge, the present investigation is first from Pakistan based upon the study population from poor to middle class groups. In 82% of the cases the cause of CL/P remained unknown and this finding is consistent with other studies. [5],[10]
There is a large variation in the distribution of different types of OFCs. The present survey presents isolated CL 2%, isolated CP 72%, and CLP 26%. However, a study from south India has shown these figures as 33%, 2%, and 65% respectively. [11] A retrospective study from Jordan has shown different figures as isolated CL 30%, isolated CP 22%, and CLP 48%. [10] In the present study, bilateral CL was lower as compared to 21% from south Indian and 30% from an Iranian study. [4],[11] The frequency of left sided CL in this survey is also lower as compared to that of south Indian study, 64%, and 66% from Iran.
OFCs were equally distributed among males and females in the present investigation. However, studies from Jordan, south India and Iran have reported higher proportion of OFCs among male patients, i.e., 55%, 58% and 65% respectively. [4],[10],[11] In the present study, CLP was more common in males and CP more common among females. This finding is consistent with other studies from Europe, Middle-East, India and USA. [5],[10],[11],[12]
The above discrepancy of sex, side, and type specific distribution of OFCs in different studies may be due to difference in sample size, ethnicity, geographical location, and socio-economic status of the population, case selection, and case finding methods.
Consanguinity is a biological factor much related with the culture of any society. The fundamental disadvantage of consanguinity is the emergence of rare recessive homozygous disorders, which otherwise may not appear in an out bred population. [13] The frequency of consanguineous marriages in the present study (63%) is significantly more as compared to general population of Punjab (46%). [14] A recent study from south India has also shown similar results. [11]
The etiological classification of OFCs, i.e., environmental, genetic or untraceable as described in the present study has also been used by other researchers. [15] This grouping is useful and simple when planning interventions for the prevention of OFCs.
A substantial proportion of children in the present study had recognized patterns of malformation. [8] More than 300 syndromes are known to have CL/P as an associated anomaly (Online Mendelian Inheritance in Man: http: www.ncbi.nlm.nih.gov/omim ). Probably due to high prevalence of inbreeding in Pakistani communities [14] some rare autosomal recessive syndromes, like Jarcho-Levin syndrome, Nager syndrome and Oral-Facial-Digital syndrome XI appeared in the present study population.
Exogenous substances such as drugs, cigarette smoking, maternal diabetes, alcohol consumption during the pregnancy, and the development of hyperthermia during early pregnancy substantially increase risk of cleft formation in developing embryo. [8],[16] Teratogenic effect of anticonvulsants, maternal diabetes, and hyperthermia was seen in 4 cases of OFCs in the present investigation. Studies on animal models have revealed that anticonvulsants reduce the facial prominences growth, especially of lateral nasal process, leading to inappropriate apposition of lateral nasal and maxillary processes resulting in CL. [17]
In four dysmorphic children with CL/P in the present study the cause of dysmorphism remained unknown. All routine conventional investigations including the chromosomal analysis were normal in these children. Genomic imbalances, deletions or translocations, particularly at submicroscopic level in subtelomeric regions, are believed to be a major cause of birth defects in many dysmorphic children. Detection of deletions and translocations at DNA level depend upon the usage of gene micro-array technology. We suggest molecular cytogenetic studies using chromosomal microarray analysis (CMA) for those four cases with dysmorphic features of probable genetic origin. [18]
The mechanism responsible for non-syndromic CL/P is not well-understood however, probably multifactorial in nature involving both genetic and environmental factors. The familial pattern and risk of recurrence in subsequent pregnancies of such cases signifies genetic component. Studies on monozygotic twins have emphasized the linkage between the genetic and environmental influences. One such study is from Denmark showing recurrence risk for both types of clefts (CL and CP) greater in dizygotic twins than in non-twin siblings with heritability estimates above 90% for both CL/P and CP. [6] The concordance rate of OFCs in monozygotic twins has never been 100% meaning there by that genetic components are not the sole operating elements for oral clefts. This observation has led to the assumption that the etiology of OFCs is by enlarge multifactorial.
In recent years, a number of significant breakthroughs have occurred with respect to the molecular genetics of OFCs. The rapid advances in molecular biology involving use of gene targeting technology, direct sequence analysis, and traditional developmental techniques have identified numerous candidate genes and gene pathways critical for craniofacial development. These advances have discovered mutations in the interferon regulatory factor-6 (IRF6) gene as the cause of van der Woude syndrome (VWS) and the poliovirus receptor related-1 (PVRL1) gene as being responsible for an autosomal recessive ectodermal dysplasia syndrome associated with CL/P. [19],[20],[21] PVRL1 encodes a cell adhesion molecule called nectin-1, which in the mouse embryo is highly expressed in the medial edge epithelium of the developing palate. VWS is one of the best models for non-syndromic CL/P. It is an autosomal dominant disorder characterized by the presence of pits on the lower lip in addition to CL/P. Another autosomal dominant condition comprising ectrodactyly, ectodemal dysplasia, and orofacial cleft syndrome is due to the mutations in the p63 gene. In mouse embryo, p63 is expressed in limb bud apical ectoderm and maxillary and mandibular processes. [20] A case control study in Northeastern European population provides evidence implicating FGF1 in the occurrence of CL/P, and support TIMP2 and WNT9B as novel candidate genes. It is likely that variation in FOXE1, TIMP2, FGFp1 and Wnt signaling pathway genes confers susceptibility to non-syndromic CL/P. [22] Evidence is accumulating that several other candidate genes showing strong linkage to the development of CL/P act as modifiers. [20]
Population of the present study belonged to poor to middle class social strata living in semi-urban and rural areas where mothers suffer from multiple nutrition deficiencies. The role of vitamins deficiency in pregnant mothers as a cause of fetal malformations is well-documented. [23] Folate deficiency in pregnant mothers has been linked to an increased incidence of neural tube defects. And in supplementation of folate to women during periconception period has shown to reduce the incidence of OFCs substantially as compared to that in the non-supplemented controls. [24] In fact, folic acid deficiency may be responsible for the different malformations in developing embryo through a common mechanism and probably this effect is modified depending upon the genetic background of the developing embryo. Further investigations are required to study in depth how nutritional factors would modify the expression of genotype leading to breakdown in the normal mechanisms involved during early embryonic development of the face. Unlike genetic factors, nutritional causes seem to be more important as those can be easily corrected and may therefore be used as useful tool in public-health for the prevention of OFCs.
Associated anomalies with OFCs were present in 18% of the patients in the present investigation. A similar figure (18%) has been reported from a study from Jordan. [10] However, a study from Iran has shown a lower frequency of associated anomalies with OFC cases, i.e., 13%. [4] Anomalies of the craniofacial region were most frequent followed by cognitive impairment. A study from Iran has also reported anomalies of head and face region being most frequent. [4] The clinical research shows that head, neck and face regions and cardiovascular system are involved in more than 60% of the recognized malformations in man. [8] Microbiological research has shown that neural crest cells are essential for the formation of structures in craniofacial region and apposition of medial nasal, lateral nasal, and maxillary processes. In cases with CL/P these cells are deficient in superoxide dismutase and catalase enzymes that are responsible for scavenging free radicals that damage these cells. More over the high vulnerability of neural crest cells to environmental teratogens such as radiation, chemicals, heat, and viruses make craniofacial region and brain the most vulnerable tissue for damage. Not the least, the craniofacial regions with all its organs for special senses involve a large group of genes with inductive influence for each other. A mutation in a single gene can affect function of several other neighboring genes. [17],[25]
OFCs pose a special social problem for the sufferers and economic burden for the health- care system. [24] Children with OFCs have high morbidity and mortality. Although, there has been much progress in the management of such cases and their access to health-care system; however, access to health-care system varies between and within countries and hence some clefts remain unrepaired even into adulthood. Even among repaired clefts there is residual deformity affecting facial outlook and speech of these children. Children with OFCs require a multidisciplinary medical approach including, surgery, dental, orthodontic, speech, hearing, psychosocial support, and rehabilitation. This means an important effort in terms of social organization as well as economical costs for the health-care system as management of these anomalies have lifelong implications for affected individuals. Last but not the least, the prevention at mass scale involves motivation for maternal health and nutrition supplements in periconception period with special reference to folic acid. Improving our knowledge of the role of nutrition, genes, and their interactions in the pathogenesis of OFCs may stimulate the development of nutritional interventions for OFCs prevention in future. In case the OFC is associated with a recognized pattern of malformation with known pattern of inheritance genetic risk assessment with the use of family history and DNA based genetic testing to clarify the genetic status of the family in order to assess the possibility of prenatal diagnosis. Selective abortion is highly successful in controlling the birth of syndromic babies with OFCs in subsequent pregnancies through genetic counseling. [26]
 Acknowledgment Acknowledgment | |  |
Authors are thankful to Professor Shakila Zaman, Department of Preventive Pediatrics, the Children's Hospital, Lahore, Pakistan, and Professor Karl-Henrik Gustavson, Department of Clinical Genetics, Uppsala University Children's Hospital, Uppsala, Sweden, for their helpful comments on the manuscript. This research was financially supported by Smile Train through Lahore CL and CP Society, Pakistan.
 References References | |  |
| 1. | Mossey P, Little J. Addressing the challenges of cleft lip and palate research in India. Indian J Plast Surg 2009;42:S9-S18. 
|
| 2. | Krapels IP, Vermeij-Keers C, Müller M, de Klein A, Steegers-Theunissen RP. Nutrition and genes in the development of orofacial clefting. Nutr Rev 2006;64:280-8. 
|
| 3. | Wong FK, Hagg U. An update on the aetiology of orofacial clefts. Hong Kong Med J 2004;10:331-6. 
[PUBMED] |
| 4. | Yazdee AK, Saedi B, Sazegar AA, Mehdipour P. Epidemiological aspects of cleft lip and palate in Iran. Acta Med Iran 2011;49:54-8. 
[PUBMED] |
| 5. | Lilius GP. Clefts with associated anomalies and syndromes in Finland. Scand J Plast Reconstr Surg Hand Surg 1992;26:185-96. 
[PUBMED] |
| 6. | Grosen D, Bille C, Petersen I, Skytthe A, Hjelmborg Jv, Pedersen JK, et al. Risk of oral clefts in twins. Epidemiology 2011;22:313-9. 
[PUBMED] |
| 7. | Bianchi F, Calzolari E, Ciulli L, Cordier S, Gualandi F, Pierini A, et al. Environment and genetics in the etiology of cleft lip and cleft palate with reference to the role of folic acid. Epidemiol Prev 2000;24:21-7. 
[PUBMED] |
| 8. | Jones KL. Smith's Recognizable Patterns of Human Malformation. 6 th ed. Philadelphia: WB Saunders Company; 2006. p. 264-5 and 664-5. 
|
| 9. | Blackmon LR. In: Sanders RC, Blackmon LR, Hogge WA, Spevak P, Wulsberg EA, editors. Structural Fetal Abnormalities. 2 nd ed. London: Mosby an Imprint of Elesevier Science; 2002. p. 255-66. 
|
| 10. | Al Omari F, Al-Omari IK. Cleft lip and palate in Jordan: Birth prevalence rate. Cleft Palate Craniofac J 2004;41:609-12. 
[PUBMED] |
| 11. | Reddy SG, Reddy RR, Bronkhorst EM, Prasad R, Ettema AM, Sailer HF, et al. Incidence of cleft Lip and palate in the state of Andhra Pradesh, South India. Indian J Plast Surg 2010;43:184-9. 
[PUBMED]  |
| 12. | Grant SF, Wang K, Zhang H, Glaberson W, Annaiah K, Kim CE, et al. A genome-wide association study identifies a locus for non-syndromic cleft lip with or without cleft palate on 8q24. J Pediatr 2009;155:909-13. 
[PUBMED] |
| 13. | Hedrick PW. Genetics of Populations. 2 nd ed., Ch. 5 (Inbreeding). London: Jones and Bartlett Publishers; 2000. p. 179-224. 
|
| 14. | Yaqoob M, Gustavson KH, Jalil F, Karlberg J, Iselius L. Early child health in Lahore, Pakistan: II. Inbreeding. Acta Paediatr Suppl 1993;82:17-26. 
[PUBMED] |
| 15. | Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: Understanding genetic and environmental influences. Nat Rev Genet 2011;12:167-78. 
[PUBMED] |
| 16. | Schutte BC, Murray JC. The many faces and factors of orofacial clefts. Hum Mol Genet 1999;8:1853-9. 
[PUBMED] |
| 17. | Bentz ML. Bilateral cleft lip deformity. In: Bentz ML. editor. Pediatric Plastic Surgery. Stamford, Connecticut: Appleton and Lange; 1998. p. 63-7. 
|
| 18. | Lu XY, Phung MT, Shaw CA, Pham K, Neil SE, Patel A, et al. Genomic imbalances in neonates with birth defects: High detection rates by using chromosomal microarray analysis. Pediatrics 2008;122:1310-8. 
|
| 19. | Ghassibe M, Bayet B, Revencu N, Desmyter L, Verellen-Dumoulin C, Gillerot Y, et al. Orofacial clefting: Update on the role of genetics. B-ENT 2006;2:20-4. 
[PUBMED] |
| 20. | Cobourne MT. The complex genetics of cleft lip and palate. Eur J Orthod 2004;26:7-16. 
[PUBMED] |
| 21. | Stanier P, Moore GE. Genetics of cleft lip and palate: Syndromic genes contribute to the incidence of non-syndromic clefts. Hum Mol Genet 2004;13:R73-81. 
[PUBMED] |
| 22. | Nikopensius T, Kempa I, Ambrozaitytë L, Jagomägi T, Saag M, Matulevièienë A, et al . Variation in FGF1, FOXE1, and TIMP2 genes is associated with non-syndromic cleft lip with or without cleft palate. Birth Defects Res A Clin Mol Teratol 2011;91:218-25. 
|
| 23. | Czeizel AE. The primary prevention of birth defects: Multivitamins or folic acid. Int J Med Sci 2004;1:50-61. 
[PUBMED] |
| 24. | World Health Organization. Community Genetics Services. Report of a WHO Consultation on community genetics in low- and middle-income countries Geneva, Switzerland: 13-14 September 2010. 
|
| 25. | Sadler TW. Head and neck. In: Sadler TW editor. Langman's Medical Embryology. 11 th ed. Philadelphia: Lippincott Williams and Wilkins Publishers; 2010. p. 265. 
|
| 26. | Mossey PA, Shaw WC, Munger RG, Murray JC, Murthy J, Little J. Global oral health inequalities: Challenges in the prevention and management of orofacial clefts and potential solutions. Adv Dent Res 2011;23:247-58. 
[PUBMED] |
[Figure 1]
[Table 1], [Table 2]
| This article has been cited by | | 1 |
Telbivudine Prevents Vertical Transmission of Hepatitis B Virus From Women With High Viral Loads: A Prospective Long-Term Study |
|
| Quanxin Wu,Hongfei Huang,Xiaowen Sun,Meiming Pan,Yun He,Shun Tan,Yi Zeng,Li Li,Guohong Deng,Zehui Yan,Dengming He,Junnan Li,Yuming Wang | | Clinical Gastroenterology and Hepatology. 2014; | | [Pubmed] | [DOI] | |
|
 |
|






