| |


 |
| Year : 2012 | Volume
: 6
| Issue : 3 | Page : 90-96 |
|
|
|
|
|
SURGICAL TECHNIQUE Miniopen coracohumeral ligament release and manipulation for idiopathic frozen shoulder
Abdelsalam Eid
Department of Orthopaedic Surgery, Faculty of Medicine, Zagazig University, Egypt
Correspondence Address:
Abdelsalam Eid
Department of Orthopaedic Surgery, Faculty of Medicine, Zagazig University, 5 Mahfouz Street, From Ahmed Ismail Street, Zagazig, 44511
Egypt
 Source of Support: None, Conflict of Interest: None  | 3 |
DOI: 10.4103/0973-6042.102561

|
|
|
|
| Date of Web Publication | 17-Oct-2012 |
 Abstract Abstract | | |
In the management of idiopathic frozen shoulder, manipulation under anaesthesia is known to have serious potential complications including fractures and intra-articular injuries. Arthroscopy is a safer treatment modality but requires special instruments, experience, and involves added cost. The aim of this work was to study the use of miniopen Coracohumeral ligament release and manipulation of the shoulder as a safe and simple method of treating idiopathic frozen shoulder that could be performed as a quick procedure under short duration anaesthesia obtaining a significant improvement of shoulder function while avoiding complications that are feared to occur with the use of manipulation under anaesthesia. Miniopen Coracohumeral ligament release is performed through a 3-cm incision. The Coracohumeral ligament is divided, and then the shoulder is manipulated without undue force. A case series including fifteen patients (19 shoulders) with idiopathic frozen shoulder operated by this technique is described. Miniopen Coracohumeral ligament release and manipulation is a quick procedure that may be performed under short duration anaesthesia obtaining a significant improvement of shoulder function meanwhile avoiding complications that are feared to occur with the use of manipulation under anaesthesia.
Keywords: coracohumeral ligament, frozen shoulder, mini-open, safe, simple
How to cite this article:
Eid A. Miniopen coracohumeral ligament release and manipulation for idiopathic frozen shoulder. Int J Shoulder Surg 2012;6:90-6 |
 Introduction Introduction | |  |
Primary frozen shoulder is a common condition. Earlier studies have suggested a prevalence of 2 to 5% in the general population and 11 to 36% in diabetics. [1],[2] However, a recent study demonstrated a prevalence of 0.5% in the general population and 4.3% in patients with diabetes mellitus. In patients with diabetes, the prevalence of frozen shoulder was found to be higher if the duration of diabetes was longer. [3] Although the condition is reported to be self limited, and the natural history usually ends in improvement, [1],[2] numerous lines of conservative and operative treatment have been proposed for it. This is because the disease, left untreated, runs a prolonged course over years. In addition, the ultimate resolution may not be complete. A prospective study with 5 to 10 years' follow-up found that only 39% of the patients had full recovery, while 54% had clinical limitation without functional disability, and 7% had functional limitation. [4] In another study, 50% of the patients had some degree of pain and stiffness at an average of seven years after onset of the disease. [5] Moreover, some patients are unwilling to endure the painful limitation of motion while they wait for resolution of the condition. [6]
Some authors described improvement of the shoulder range of motion using non-operative measures like local corticosteroid injections. [7] Others used a program of stretching exercises. [8] However, these authors also declared that a significant percentage of their patients had residual functional limitations, and some did not improve, and required further measures to manage the stiffness. [9]
Manipulation under anesthesia (MUA) is a well-established and accepted method of treatment of frozen shoulder that allows early restoration of mobility. [9],[10],[11] The disadvantage of MUA, however, is that it does not allow for controlled release of pathologic tissues. In addition, the toughness of the pathologic tissues may require the use of significant force until they yield. This combined with osteopenia present in most patients with frozen shoulder form old age, disuse, and/or diabetes poses a significant risk of causing a humeral fracture. Although fractures are frequently listed as potential complications of MUA, few papers actually report the actual occurrence of humeral [12],[13] and glenoid [14] fractures. Other complications that may occur include glenohumeral dislocation, rotator cuff tearing, and nerve injuries. [1,7],[8],[15] This has encouraged many orthopedic and shoulder surgeons to use arthroscopy to visualize and divide the incriminated pathologic tissues. However, the use of arthroscopy in the shoulder requires a certain level of skills above that usually present in the general orthopedic surgeon. Moreover, the use of arthroscopy in case of frozen shoulder is even more difficult and requires more skills and experience than the use of arthroscopy in the management of other shoulder pathologies. [16],[17],[18],[19] In addition, arthroscopic capsular release is a more costly procedure than MUA due to the costs of the arthroscope itself, besides the use of disposable cannulas and electrocautery knives, which imposes a financial burden, particularly in developing countries where health services are often paid for by the patient him/herself.
The aim of this work was to study the use of mini-open Coracohumeral ligament (CHL) release followed by manipulation of the shoulder as a simple method of treating idiopathic frozen shoulder. Our hypothesis was that mini-open CHL release followed by MUA could be performed as a quick procedure under short duration anesthesia obtaining a significant improvement of shoulder function meanwhile avoiding complications that are feared to occur with the use of MUA.
Surgical technique
All patients were given 2 g of third generation cephalosporin in a single dose prophylactically immediately before induction of anesthesia. Patients were positioned, prepped, and draped while still awake to save anesthesia time. Short intravenous anesthesia was given immediately before the incision [Figure 1].
The 3-cm incision comprised the uppermost extension of the deltopectoral approach between the coracoid inferiorly and the clavicle superiorly. The deltopectoral interval was developed. The conjoint tendon and the subscapularis were not met with as both lie beneath the coracoid, i.e., beneath the working area. The coracoid was palpated and followed to its lateral aspect where the CHL originates. The CHL was put under tension by having the assistant externally rotate the adducted shoulder. It was felt as a distinct band beneath the surgeon's finger. Internally rotating the shoulder relaxed the CHL which helped differentiate it from the neighboring coracoacromial ligament whose tension was fixed regardless of shoulder rotation. Sharp dissection of the coracoid origin of the CHL was done taking care to keep the blade on the lateral aspect of the coracoid just short of its tip to avoid the conjoint tendon and pectoralis minor, and not reaching its base to avoid the origin of the biceps long head from the supraglenoid tubercle. Meanwhile, the assistant applied steady external rotation force to the adducted shoulder. Further sharp release of the superior capsule was performed using the tip of scissors after inserting a dissector immediately beneath the capsule to protect the biceps tendon. As soon as the CHL was divided, the capsule yielded under the external rotation force and external rotation range of motion was obtained indicating release of superior and anterior capsule. After restoration of external rotation, the joint was manipulated into external rotation with abduction, releasing the inferior capsule, and then flexion with internal rotation, releasing the posterior capsule. Finally, the wound was closed in layers without drain.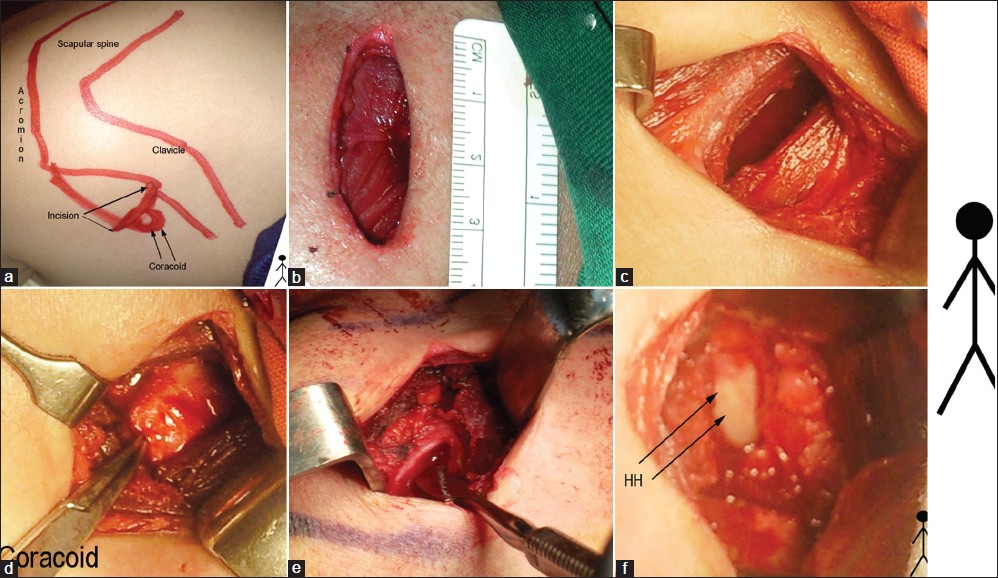 | Figure 1: Intraoperative photos of the surgical technique (This is the Right shoulder, head, and feet of the patient indicated by the stick figure to the right of the figure) (a) Outline of the bony landmarks and the incision. (b) The 3 cm incision. (c) The deltopectoral interval. (d) The coracoid. (e) Dissector under the CHL (f) Capsulotomy performed and the Humeral Head (HH) shown
Click here to view |
 Case Series Case Series | |  |
This prospective study was conducted between May 2005 and August 2009 in the department of Orthopaedic Surgery of our university hospital. As per the protocol followed in our hospital, cases of frozen shoulder are initially managed in the Rheumatology and Rehabilitation department. Their standard treatment protocol includes local corticosteroid injections and stretching exercises. Cases which do not respond to this protocol are then referred to the department of Orthopaedic Surgery for further management. During the study period, 15 patients (19 shoulders) with idiopathic frozen shoulder were operated by mini-open CHL release followed by MUA. An informed consent was obtained from every patient as well as approval of the institutional review board. The inclusion criteria were the presence of idiopathic global restriction of glenohumeral motion and a reasonable trial of conservative treatment and physiotherapy as previously stated. The exclusion criteria were the presence of history of significant trauma to the shoulder (post-traumatic frozen shoulder), the development of stiffness following an operation on the shoulder (postoperative frozen shoulder), the presence of concomitant shoulder pathology (e.g., rotator cuff tear), and the presence of significant pain and inflammation of the shoulder (Stage 1 frozen shoulder). The average age of the patients was 55.7 years (range: 47 to 63 years). There were nine female patients including three who had bilateral affection, and six male patients including one with bilateral affection. The right shoulder was involved in seven patients, the left in four patients, and both shoulders in four patients. In the four patients with bilateral affection, they developed involvement of the other shoulder at an average of 14.5 months (range: 12 to 18 months) following the initial procedure, respectively. All patients had tried conservative treatment in the form of NSAIDs, local injections, and stretching exercises for a period ranging from six to 15 months (Mean, 9.4 months). Five patients had had an unsuccessful attempt at MUA. Two patients had had unsuccessful arthroscopic releases. The diagnosis was made based on thorough clinical examination in all cases; however, plain radiographs and MRIs of the affected shoulders were obtained in every case to exclude any other concomitant shoulder pathology. All patients were operated on by mini-open CHL release followed by MUA of the shoulder.
In 16 cases, the procedure was performed under short intravenous anesthesia only. In three cases, a laryngeal mask was used to deliver inhalation anesthesia. However, in no case was intubation required. The mean duration of the procedure from skin incision to closure was 13.8 minutes (range, 10-18 minutes).
Postoperative care
Since the operation was done as a one-day procedure, the patient was discharged on the same day. Postoperative medication included an adequate non-steroidal analgesic and oral antibiotic for three days. The patient was given an exercise program to perform at home. Pendulum exercises were started on the day of the operation. However, passive range of motion exercises were started the next day with emphasis on external rotation and abduction. Postoperative pain was well controlled by analgesics and tolerated by all patients, and did not adversely affect the postoperative rehabilitation program.
Follow up
Follow up during the first month was performed weekly so that the surgeon could closely monitor and guide the physiotherapy program. Subsequently, patients came for follow up at 3, 6, and 12 months postoperatively, then yearly thereafter. The follow up ranged from 18 to 48 months (Mean, 34 months).
 Results Results | |  |
All patients gained a significant improvement in the range of shoulder motion following the operation. Most of the improvement in the ROM was seen in the first two weeks postoperatively. However, the ROM continued to improve over the next six months.
The patients were evaluated preoperatively using a modified Constant score [20] which did not measure shoulder strength. [9] This is because strength measurement in the Constant score required abduction to 90° which was impossible in all patients preoperatively. Postoperatively, however, the modified Constant score as well as the complete Constant score were both measured. The complete Constant score was then adjusted for age and sex. Pain was measured on a Visual Analog Scale (VAS) according to the method of Constant where (0) equals "intolerable pain," and (15) equals "no pain." [Table 1] Comparison between preoperative and the data obtained at the final follow up was done using the Wilcoxon signed ranks test. Analysis of the patients' data was done using "Microsoft Excel 2007" together with "XLSTAT Version 2012.2.01" (Copyright Addinsoft 1995-2012).
The significant items of the Constant score are detailed as follows:
Regarding pain (VAS), the mean score for pain from the affected shoulder improved from 6.8 (range, 5-10) to a mean of 14.7 (range, 10 to 15) at the final follow up. This was found to be statistically significant. (P) at a 95% confidence interval < 0.001.
Regarding the activities of daily living permitted by the shoulder in work and recreation, the mean score improved from 1.9 (range, 0-4) to a mean of 7.1 (range, 6-8) at the final follow up. (P) at a 95% confidence interval < 0.001.
As regards the level at which the patients were able to use their shoulder comfortably, at the final follow up, ten shoulders could be used above the head, eight shoulders could be used up to the top of the head, and one shoulder could be used up to the neck.
No patient reported any sleep disturbance related to the shoulder condition at the final follow up as opposed to preoperatively where all patients reported sleep disturbance related to the shoulder condition, either occasionally (8 cases), or every night (11 cases).
The improvement of the range of motion is detailed as follows:
The mean forward flexion improved from 61.3° (range, 40°- 100°) preoperatively to a mean of 150° (range, 110°-170°) at the final follow up. This was found to be statistically significant. (P) at a 95% confidence interval < 0.001.
Meanwhile, the mean abduction improved from 54.5° (range, 40°-100°) preoperatively to a mean of 152.6° (range, 120°-170°) at the final follow up. This was found to be statistically significant. (P) at a 95% confidence interval < 0.001.
The mean external rotation improved from 6.3° (range: -5° to 20°) preoperatively to a mean of 62.1° (range: 45° to 75°) at the final follow up. This was found to be statistically significant. (P) at a 95% confidence interval < 0.001.
The mean modified Constant score (Max. 75 points) improved from 19.8 (range, 13 to 35) preoperatively to 65.4 (range, 50 to 73) at the final follow up. This was found to be statistically significant. (P) at a 95% confidence interval < 0.001.
The mean complete Constant score at the final follow up was 73.3 (range: 54 to 85).
The mean Constant score adjusted for age and sex at the final follow up was 92.4% (range: 74% to 101.4%).
As regards patient satisfaction, 10 patients (14 shoulders) were very satisfied, and four patients were satisfied with the procedure. One patient was undecided.
Complications
There was no neurovascular injury or injury to any important tendons or other structures. However, there was some residual loss of internal rotation in four cases, but it was well tolerated by the patients.
 Discussion Discussion | |  |
Numerous authors have implicated the CHL as the primary restraint against external rotation in adhesive capsulitis. It has been related to restriction of external rotation, and its division has been listed by many authors as an essential step in the capsular release. [21],[22],[23] Open release of frozen shoulder is not a new concept. In fact, it has been reported by many authors as a treatment option in case of resistant cases that do not improve following MUA or arthroscopic release. [6],[8],[11],[22],[23] Others have used open release in cases with joints too contracted to allow arthroscopic maneuvers. [24] However, it has been usually described as a formal open release utilizing the deltopectoral approach and dividing the subscapularis, sometimes even Z-lengthening the subscapularis. The CHL and fibrous tissue in the rotator interval is excised and the middle glenohumeral ligament, inferior glenohumeral ligament may also be formally divided. [6],[8],[11],[22],[23],[25],[26]
Arthroscopy is believed to have become the most popular method of treating refractory adhesive capsulitis. [27] Some authors combined MUA with arthroscopic release either before arthroscopy as a means of facilitating access to the joint, as introduction of the arthroscope into the stiff shoulder with its decreased joint volume and capsular contracture is often quite difficult even for experienced arthroscopists, or after it to improve the range of motion. [16],[17],[18],[19],[28],[29],[30] In addition, arthroscopy imposes economic burdens, especially in a developing country with limited resources of the health system.
This has led us to postulate that mini-open division of the CHL would significantly weaken the capsule's resistance to stretch. The following manipulation could then be done without excessive force, so as to avoid the bony and articular injuries reported to occur with MUA. In this series, division of the CHL by sharp dissection was done as the capsule was placed under tension by external rotation of the shoulder. The tear propagated proximally and distally with minimal additional force, fully restoring external rotation. Afterwards, the capsule was weak enough so that restoration of flexion, abduction, and internal rotation occurred with minimal force. All the patients in this series gained a significant improvement in the range of shoulder motion that allowed the patients to engage immediately in the postoperative rehabilitation program.
The results obtained in this series are comparable with those reported in the literature by other authors utilizing different techniques [Table 2]. However, none of our patients suffered any serious complications on account of the intervention. This is an indication of the safety of the procedure. The mean duration of operative time was 13.8 minutes and all operations were performed under short duration anesthesia, making it an appealing procedure for anesthetists who are often concerned about the general condition and comorbidities often found in this patient population. This supports our hypothesis that mini-open CHL release followed by MUA could be performed as a quick procedure under short duration anesthesia obtaining a significant improvement of shoulder function, meanwhile avoiding complications that are feared to occur with the use of MUA.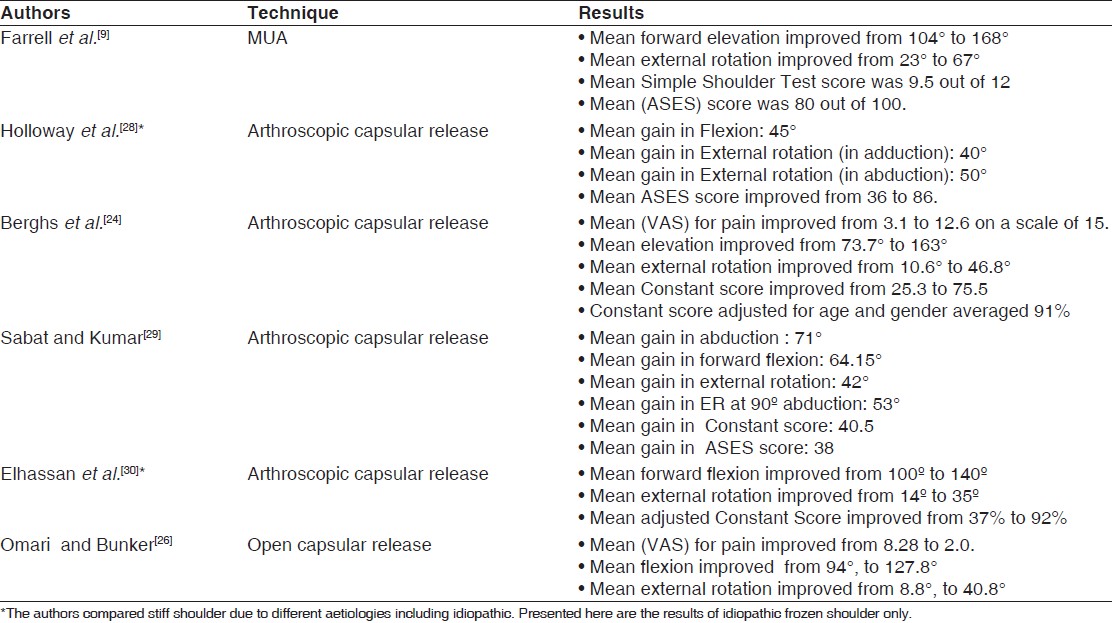 | Table 2: Examples of results of MUA, arthroscopic capsular release, and formal open release reported in the literature
Click here to view |
The ability of all the patients to engage immediately in the postoperative rehabilitation program is an indication that the minimal procedure was well tolerated by the patients and did not cause intolerable pain or soft tissue damage such as might be feared after formal open release. No special instruments or skills were required. This is an indication of the simplicity of the procedure, making it appealing for the general orthopedic surgeon in distant remote areas, less developed countries with no access to arthroscopic instruments or special training and experience, or easily accessible nearby specialized centers.
An important limitation of this study is the limited number of patients. Also, we have no data of our own regarding effectiveness of the mini-open release in comparison with MUA or arthroscopy due to the absence of a control group. However, for cases not improving after conservative treatment or MUA and non-feasibility of arthroscopy, it can be an alternative. These shortcomings, however, could be considered in further investigations regarding this technique.
 Conclusion Conclusion | |  |
Mini-open Coracohumeral ligament release and manipulation is a quick procedure that may be performed under short duration anesthesia obtaining a significant improvement of shoulder function, meanwhile avoiding complications that are feared to occur with the use of MUA.
 References References | |  |
| 1. | Tasto JP, Elias DW. Adhesive capsulitis. Sports Med Arthrosc 2007;15:216-21. 
[PUBMED] |
| 2. | Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ 2005;331:1453- 6. 
[PUBMED] |
| 3. | Thomas SJ, McDougall C, Brown ID, Jaberoo MC, Stearns A, Ashraf R, et al. Prevalence of symptoms and signs of shoulder problems in people with diabetes mellitus. J Shoulder Elbow Surg 2007;16:748-51. 
[PUBMED] |
| 4. | Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol 1975;4:193-6. 
[PUBMED] |
| 5. | Shaffer B, Tibone JE, Kerlan RK. Frozen shoulder. A long term follow up. J Bone Joint Surg Am 1992;74:738-46. 
[PUBMED] |
| 6. | Warner JJP. Frozen shoulder: Diagnosis and management. J Am Acad Orthop Surg 1997;5:130-40. 
|
| 7. | Griggs SM, Ahn A, Green A. Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. J Bone Joint Surg Am 2000;82:1398-407. 
[PUBMED] |
| 8. | Jacobs LG, Smith MG, Khan SA, Smith K, Joshi M. Manipulation or intra-articular steroids in the management of adhesive capsulitis of the shoulder. A prospective randomized trial. J Shoulder Elbow Surg 2009;18:348-53. 
[PUBMED] |
| 9. | Farrell CM, Sperling JW, Cofield RH. Manipulation for frozen shoulder: Long-term results. J Shoulder Elbow Surg 2005;14:480- 4. 
[PUBMED] |
| 10. | Hughes PJ, Evans RO, Goldberg JA. Frozen shoulder. In: Walsh WR, editor. Orthopedic Biology and Medicine: Repair and Regeneration of Ligaments, Tendons, and Joint Capsule. Totowa, NJ: Humana Press Inc.; 2005. p. 159-72. 
|
| 11. | Wang J-P, Huang T-F, Hung S-C, Ma H-L, Wu J-G, Chen T-S. Comparison of idiopathic, post-trauma and post-surgery frozen shoulder after manipulation under anaesthesia. Int Orthop 2007;31:333-7. 
|
| 12. | Quigley TB. Treatment of checkrein shoulder by use of manipulation and cortisone. J Am Med Assoc 1956;161:850-4. 
[PUBMED] |
| 13. | Hamdan TA, Al-Essa KA. Manipulation under anaesthesia for the treatment of frozen shoulder. Int Orthop 2003;27:107-9. 
[PUBMED] |
| 14. | Magnussen RA, Taylor DC. Glenoid fracture during manipulation under anaesthesia for adhesive capsulitis: a case report. J Shoulder Elbow Surg 2011;20:e23-6. 
[PUBMED] |
| 15. | Loew M, Heichel TO, Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg 2005;14:16-21. 
[PUBMED] |
| 16. | Cuomo F, Holloway GB. Diagnosis and management of the stiff shoulder. In: Iannotti JP, Williams GR Jr, editors. Disorders of the Shoulder, Diagnosis and Management. Philadelphia: Lippincott, Wiliams, and Wilkins; 2007. p. 541-59. 
|
| 17. | Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med 2008;1:180-9. 
[PUBMED] |
| 18. | Hannafin JA, Chiaia TA. Adhesive capsulitis. A treatment approach. Clin Orthop Relat Res 2000;372:95-109. 
[PUBMED] |
| 19. | Massoud SN, Pearse EO, Levy O, Copeland SA. Operative management of the frozen shoulder in patients with diabetes. J Shoulder Elbow Surg 2002;11:609-13. 
[PUBMED] |
| 20. | Constant CR, Gerber C, Emery RJH, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg 2008;17:355-61. 
|
| 21. | DePalma AE. Loss of scapulohumeral motion (frozen shoulder). Ann Surg 1952;135:193-204. 
|
| 22. | Neer CS, Satterlee CC, Dalsey RM, Flatow EL. The anatomy and potential effects of contracture of the coracohumeral ligament. Clin Orthop 1992;280:182-5. 
|
| 23. | Ozaki J, Nakagawa Y, Sakurai G, Tamai S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am 1989;71:1511-5. 
[PUBMED] |
| 24. | Berghs BM, Sole-Molins X, Bunker TD. Arthroscopic release of adhesive capsulitis. J Shoulder Elbow Surg 2004;13:180-5. 
|
| 25. | Hsu JE, Anakwenze OA, Warrenderb WJ, Abboud JA. Current review of adhesive capsulitis. J Shoulder Elbow Surg 2011;20:502-14. 
|
| 26. | Omari A, Bunker TD. Open surgical release for frozen shoulder: Surgical findings and results of the release. J Shoulder Elbow Surg 2001;10:353-7. 
[PUBMED] |
| 27. | Neviaser AS, Hannafin JA. Adhesive capsulitis: A review of current treatment. Am J Sports Med 2010;38:2346-56. 
[PUBMED] |
| 28. | Holloway GB, Schenk T, Williams GR, Ramsey ML, Iannotti JP. Arthroscopic capsular release for the treatment of refractory postoperative or post-fracture shoulder stiffness. J Bone Joint Surg Am 2001;83:1682-7. 
[PUBMED] |
| 29. | Sabat D, Kumar V. Early arthroscopic release in stiff shoulder. Int J Shoulder Surg 2008;2:36-40. 
[PUBMED]  |
| 30. | Elhassan B, Ozbaydar M, Massimini D, Higgins L, Warner JJ. Arthroscopic capsular release for refractory shoulder stiffness: A critical analysis of effectiveness in specific etiologies.J Shoulder Elbow Surg 2010;19:580-7. 
[PUBMED] |
[Figure 1]
[Table 1], [Table 2]
|
