| |


 |
| Year : 2015 | Volume
: 9
| Issue : 4 | Page : 110-113 |
|
|
|
|
|
ORIGINAL ARTICLE In-hospital mortality risk for total shoulder arthroplasty: A comprehensive review of the medicare database from 2005 to 2011
Frank McCormick1, Benedict U Nwachukwu2, Emmanouil B. S. Kiriakopoulos1, William W Schairer2, Matthew T Provencher3, Jonathan Levy1
1 Holy Cross Orthopedic Institute, Holy Cross Hospital, Fort Lauderdale, FL, USA
2 Department of Orthopedic Surgery, Hospital for Special Surgery, New York, NY, USA
3 Department of Sports Medicine, Massachusetts General Hospital, Boston, MA, USA
Correspondence Address:
Frank McCormick
5597 North Dixie Highway, Fort Lauderdale, FL 33334
USA
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.167938
 |
|
|
|
| Date of Web Publication | 22-Oct-2015 |
 Abstract Abstract | | |
Introduction: The in-hospital mortality rate after total shoulder arthroplasty (TSA) is unknown. The purpose of this study is to quantify the in-patient mortality rates and associated demographic risk factors for patients undergoing a TSA from 2005 to 2011 using a comprehensive Medicare registry database.
Materials and Methods: We conducted a retrospective review of the Medicare database within the PearlDiver database. The PearlDiver database is a publicly available Health Insurance Portability and Accountability Act-compliant national database that captures 100% of the Medicare hospital data for TSA between 2005 and 2011. Using International Classification of Diseases, Ninth Revision codes for TSA we identified a dataset of patients undergoing TSA as well as a subset of those for whom there was a death discharge (i.e., in-patient death). Risk for this outcome was further quantified by age, gender and year. Linear regression was performed to identify risk factors for the primary outcome.
Results: A total of 101,323 patients underwent 125,813 TSAs between 2005 and 2011. There were 113 in-patient mortalities during this period. Thus the incidence of death was 0.09%. Increasing age was a significant risk factor for mortality (P = 0.03). Gender and year of procedure were not significant risk factors for mortality.
Conclusion: The incidence of in-patient mortality for Medicare patients undergoing TSA between 2005 and 2011 was <1 in 1000 surgeries. Increased age is a significant predictor of mortality.
Level 4: Retrospective analysis
Keywords: Complications, in-hospital mortality, Medicare, reverse total shoulder replacement, total shoulder replacement
How to cite this article:
McCormick F, Nwachukwu BU, Kiriakopoulos EB, Schairer WW, Provencher MT, Levy J. In-hospital mortality risk for total shoulder arthroplasty: A comprehensive review of the medicare database from 2005 to 2011. Int J Shoulder Surg 2015;9:110-3 |
How to cite this URL:
McCormick F, Nwachukwu BU, Kiriakopoulos EB, Schairer WW, Provencher MT, Levy J. In-hospital mortality risk for total shoulder arthroplasty: A comprehensive review of the medicare database from 2005 to 2011. Int J Shoulder Surg [serial online] 2015 [cited 2016 Sep 20];9:110-3. Available from: http://www.internationalshoulderjournal.org/text.asp?2015/9/4/110/167938 |
 Introduction Introduction | |  |
The risks and benefits associated with surgical intervention are an integral aspect of preoperative surgeon-patient counseling. In-hospital risk of morbidity and mortality is of particular importance to patients. For total hip arthroplasty (THA) and total knee arthroplasty (TKA) in-hospital risk of mortality has been reported to range from 0.13 to 0.46%. [1],[2],[3],[4] There is a paucity of evidence reporting on the mortality risk associated with total shoulder arthroplasty (TSA). [5] As such, surgeons counseling potential shoulder arthroplasty recipients often rely on anecdotal evidence due to a lack of published data. Given the prior published literature for arthroplasty in other joints and orthopedic procedures in general, the mortality risk is perceivably small, however a quantification of the rates specific to TSA enables the shoulder surgeon to provide truly informed surgical consent. Moreover, specific modifiable and nonmodifiable risk factors may affect mortality rates and aid in surgical decision-making, preoperative screening and postsurgical care and rehabilitation methods.
Mortality after orthopaedic procedures has traditionally been difficult to study, in large part due to a low overall incidence. Evidence for mortality after TSA has relied primarily on institutional data. [5],[6] As such the current evidence significantly lacks the generalizability for the end-point of interest. Recent advances in electronic health records and supercomputer technology have enabled for more accurate capture and review of United States national healthcare trends. As such there are now large datasets with sufficient power to understand and abstract risks and trends associated with various procedures. Databases with 100% capture of Medicare data provide an opportunity for accurate reporting of in-hospital mortality rates coupled with demographic and medical factors that are associated with mortality.
The purpose of this study is to quantify the in-patient mortality rates for patients undergoing a TSA as well as the associated demographics from 2005 to 2011 using a comprehensive Medicare registry database. Our hypothesis is that the in-hospital mortality rate after TSA is rare and that age is a significant risk factor for mortality.
 Materials and Methods Materials and Methods | |  |
We conducted a retrospective review of the Medicare data within the PearlDiver database. The PearlDiver database is a publicly available, Health Insurance Portability and Accountability Act-compliant national database. PearlDiver captures 100% of the Medicare hospital charge data for TSA between 2005 and 2011. The database currently includes over 2 billion individual patient records. Diagnosis and procedures are encrypted using Current Procedural Terminology (CPT) and International Classification of Diseases, Ninth Revision (ICD-9) with codes specific to orthopedic measures. The database was queried based on hospital in-patient ICD-9 procedural codes for TSA (ICD-9-P-81.80). Stratified sampling was conducted through PearlDiver by creating a group within the data set calling for individuals with a death discharge from in-patient service centers using the procedure code ICD-9-P-81.80 (TSA), and compared against those with other discharge diagnoses (home and rehab). Note that there was no separate ICD-9 code for reverse TSA (rTSA) prior to 2010 thus our patient sample includes a subset of patients receiving rTSA prior to 2010. Data were further analyzed for demographic parameters, assessing age, gender, and year the procedure was performed.
Using the database we determined the number of death discharges from in-patient service centers within the available data. We secondarily assessed the influence of demographics such as age, gender, year of procedure.
Descriptive analyses were performed. We constructed a Poisson regression model to look at the influence of age and year of procedure on mortality risk. We used Fisher's exact testing to analyze mortality risk based on gender. Pearson's correlation was used to assess the impact of medical comorbidity with mortality. Results were deemed statistically significant at P = 0.05. All statistics were performed using. Statistical analyses were performed using Stata V.13 (StataCorp LP, College Station, Texas, USA).
 Results Results | |  |
A total of 101,323 patients underwent 125,813 TSAs at an in-patient setting between 2005 and 2011. There were 113 in-patient mortalities following TSA during the study period. The in-patient risk of mortality was 0.09%, or <1 in 1000 surgeries. Thus, perioperative survival rate is >99.9%.
Annual mortality risk was looked at as a function mortality risk per procedure performed [Table 1]. The annual mortality risk ranged from 0.05% (2011) to 0.11% (2009). The year during which the procedure was performed was not a predictor of mortality (P = 0.14). We looked at mortality risk based on 5 years age group sub-analyses [Table 2]. The highest risk for in-hospital mortality was in patients older than 84 years old. Increased age was a significant risk for in-patient mortality (P = 0.03). In-patient mortality was more common in women [Table 3] however there was no significant mortality risk based on gender (P = 0.163).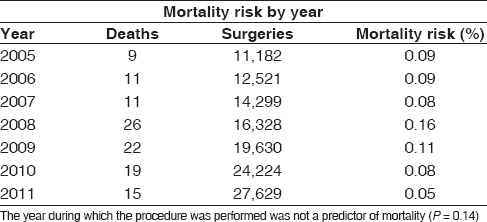 | Table 1: The risk rate and risk of mortality stratified by year of procedure performed from 2005 to 2011
Click here to view |
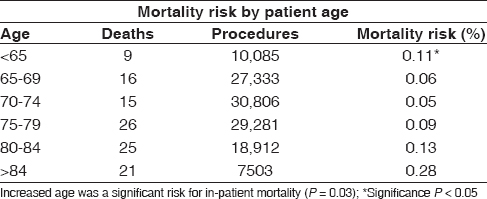 | Table 2: The mortality rate and risk of death as stratified by patient age at time of surgery
Click here to view |
 Discussion Discussion | |  |
The purpose of this study was to quantify in-hospital mortality rates for Medicare patients undergoing TSA between 2005 and 2011. We accept our null hypothesis : I0 n-hospital mortality after TSA is a rare event (0.09%-<1 in 1000 operations) and associated with increasing age. Death is the ultimate adverse outcome after any surgical procedure. Understanding surgical mortality risk is a vital component of medical-decision making, patient counseling and informed consent.
In-hospital mortality rate after TSA using a large national dataset has not been previously reported. One prior study using 30 years institutional data reported a 0.58% 90 days mortality rate after TSA. [5] In the study population, mortality risk was associated with the indication for TSA - neoplasm being the most significant risk for 90 days mortality. The authors found no deaths in patients undergoing elective TSA. Another study, similarly using long-term institutional data reported a 0.8% 90 days mortality risk associated with TSA. [7] Another prior study looked at 30 days mortality after TSA and the authors used a nationally representative data samples from the Veterans Administration National Surgical Quality Improvement Program for fiscal years 1999-2006. [8] The authors report a 0.4% mortality risk.
In this study, we report the in-hospital mortality rate after TSA to be 0.09%. Based on prior evidence there is no direct comparison. However, our reported in-hospital mortality rate is significantly lower than previously reported 30 days and 90 days mortality rates. The lower reported rate in the present study is likely due to a smaller follow-up period (i.e., in-patient admission). Our data suggests that from a mortality perspective TSA is a highly safe procedure and even safer than previously reported. Furthermore, in comparison to prior published in-hospital mortality data for TKA (0.21-0.51%) [9] and THA (0.29-0.33%), [10] TSA appears to be have lower mortality risk.
A major strength of our study compared to prior studies is the reporting of data from a national sample that is complete. In quantifying the risk of a rare-event, it is necessary to sample large and representative populations to garner an accurate estimate. Supercomputer technology has introduced the ability to review large databases accurately and cost-effectively. This study was able to gather a large cohort of patients undergoing TSA and to capture those with a discharge diagnosis of death, thereby capturing in-hospital, perioperative mortality risk. We were able to further breakdown this data between demographic variables of age, gender and year of surgery to appropriately stratify for the risk factors of mortality.
The influence of age on mortality risk after TSA has been previously investigated. Ricchetti et al. [6] found that there was no increased risk of mortality in TSAs performed in patients older than 80. However, the authors used a retrospective case control study design to assess 43 TSAs in patients older than 80 years. As such, the study was likely underpowered to detect mortality as a rare event. The TKA and THA evidence base suggests that age is an independent risk factor for postoperative complication and mortality. [11],[12],[13],[14],[15] Our findings support the previous nonshoulder total joints literature and identify advanced age as an important risk factor for mortality.
The significance of the in-patient mortality risk after TSA identified in this study should be evaluated in concert with the general risks associated with hospitalization and undergoing medical intervention of any kind. The micromort concept is a useful notion for conceptualizing the in-patient mortality risk presented in the present study. The micromort concept was first articulated by Stanford University Professor Ron Howard in 1968 and has been used when discussing risk trade-offs. [16] A micromort is a 1 in a million chance of death. This quantification of death allows comparison to other activities. The risk of mortality has thus been quantified to other medical and even leisurely activities based on the micromort concept. Based on our calculations, TSA surgery in a Medicare patient is <1000 micromorts. This makes this surgery nearly 5 times more dangerous than giving birth in the United States (170 micromorts) and 100 times more dangerous than undergoing general anesthesia alone (10 micromorts). A night in the hospital equates to 75 micromorts, thus, the mortality risk associated with hospitalization alone may be a contributing factor in the mortality risk for TSA.
There are certain limitations to the findings of the present study. Because our study utilizes CPT coding data, we are not able to differentiate between rTSA versus TSA. rTSA was not commonly performed prior to 2010. With a new CPT code now for rTSA, more work needs to be done in order to understand the demographics for this procedure, as well as the associated mortality risk. The database is subject to a lack of detailed patient-level data that is often absent in large patient databases. As such we cannot report on certain demographic and epidemiologic factors, such as height, weight, body mass index, activity level, race and socioeconomic status. Previous work on outcomes after total joint arthroplasty suggests that these demographics are important modifiers of outcome. [17],[18] In addition to the absence of certain patient demographics, we are unable to abstract causes of death from the database. Furthermore, as with any retrospective database investigation, the accuracy of coding within the system is critical to the validity of the findings. Moreover, we did not include the patients who underwent surgery at an outpatient center. This was a very limited number of patients that are assumed to be healthy enough where the risk is unlikely to be any higher than the patients who undergo the procedure as an impatient. We are unable to determine causes of death from this study. We also acknowledge that the scope of our mortality risk assessment is limited to in-hospital. As such, we do not capture perioperative and early mortality (i.e., 30-90 days mortality). This was not the intended goal of our study however. The utilization of "death discharges" allows us to capture with reasonable certainty all in-patient deaths after TSA. 30-90 days mortality estimates using the same dataset would introduce significant estimation errors and weaken the conclusions of this study. Finally, because the nature of our study was a database study, we were unable to conduct a multivariate analysis to control for increasing comorbidities with age. As such, we cannot conclude that age is an independent risk factor for mortality.
 Conclusion Conclusion | |  |
The incidence of in-patient mortality for Medicare patients undergoing TSA between 2005 and 2011 was <1 in 1000 surgeries. Increased age is a significant predictor of mortality.
 Acknowledgments Acknowledgments | |  |
The authors would like to thank Leonardo Villarroel, Clinical Research Coordinator, for his assistance in the preparation of this manuscript including data analysis and interpretation, revisions of manuscript and administrative and technical support.
 References References | |  |
| 1. | Bhattacharyya T, Iorio R, Healy WL. Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am 2002;84-A:562-72.  |
| 2. | Gill GS, Mills D, Joshi AB. Mortality following primary total knee arthroplasty. J Bone Joint Surg Am 2003;85-A:432-5.  |
| 3. | Memtsoudis SG, Della Valle AG, Besculides MC, Esposito M, Koulouvaris P, Salvati EA. Risk factors for perioperative mortality after lower extremity arthroplasty: A population-based study of 6,901,324 patient discharges. J Arthroplasty 2010;25:19-26.  |
| 4. | Memtsoudis SG, Pumberger M, Ma Y, Chiu YL, Fritsch G, Gerner P, et al. Epidemiology and risk factors for perioperative mortality after total hip and knee arthroplasty. J Orthop Res 2012;30:1811-21.  |
| 5. | White CB, Sperling JW, Cofield RH, Rowland CM. Ninety-day mortality after shoulder arthroplasty. J Arthroplasty 2003;18:886-8.  |
| 6. | Ricchetti ET, Abboud JA, Kuntz AF, Ramsey ML, Glaser DL, Williams GR Jr. Total shoulder arthroplasty in older patients: Increased perioperative morbidity? Clin Orthop Relat Res 2011;469:1042-9.  |
| 7. | Singh JA, Sperling JW, Cofield RH. Ninety day mortality and its predictors after primary shoulder arthroplasty: An analysis of 4,019 patients from 1976-2008. BMC Musculoskelet Disord 2011;12:231.  |
| 8. | Fehringer EV, Mikuls TR, Michaud KD, Henderson WG, O′Dell JR. Shoulder arthroplasties have fewer complications than hip or knee arthroplasties in US veterans. Clin Orthop Relat Res 2010;468:717-22.  |
| 9. | Memtsoudis SG, Della Valle AG, Besculides MC, Gaber L, Laskin R. Trends in demographics, comorbidity profiles, in-hospital complications and mortality associated with primary knee arthroplasty. J Arthroplasty 2009;24:518-27.  |
| 10. | Liu SS, Della Valle AG, Besculides MC, Gaber LK, Memtsoudis SG. Trends in mortality, complications, and demographics for primary hip arthroplasty in the United States. Int Orthop 2009;33:643-51.  |
| 11. | D′Apuzzo MR, Pao AW, Novicoff WM, Browne JA. Age as an independent risk factor for postoperative morbidity and mortality after total joint arthroplasty in patients 90 years of age or older. J Arthroplasty 2014;29:477-80.  |
| 12. | Fehring TK, Odum SM, Fehring K, Springer BD, Griffin WL, Dennos AC. Mortality following revision joint arthroplasty: Is age a factor? Orthopedics 2010;33:715.  |
| 13. | Memtsoudis SG, Sun X, Chiu YL, Nurok M, Stundner O, Pastores SM, et al. Utilization of critical care services among patients undergoing total hip and knee arthroplasty: Epidemiology and risk factors. Anesthesiology 2012;117:107-16.  |
| 14. | Singh JA, Lewallen DG. Ninety-day mortality in patients undergoing elective total hip or total knee arthroplasty. J Arthroplasty 2012;27:1417-22.  |
| 15. | Whittle J, Steinberg EP, Anderson GF, Herbert R, Hochberg MC. Mortality after elective total hip arthroplasty in elderly Americans. Age, gender, and indication for surgery predict survival. Clin Orthop Relat Res 1993:119-26.  |
| 16. | Howard RA. Microrisks for medical decision analysis. Int J Technol Assess Health Care 1989;5:357-70.  [ PUBMED] |
| 17. | Nwachukwu BU, Collins JE, Nelson EP, Concepcion M, Thornhill TS, Katz JN. Obesity & hypertension are determinants of poor hemodynamic control during total joint arthroplasty: A retrospective review. BMC Musculoskelet Disord 2013;14:20.  |
| 18. | Nwachukwu BU, Kenny AD, Losina E, Chibnik LB, Katz JN. Complications for racial and ethnic minority groups after total hip and knee replacement: A review of the literature. J Bone Joint Surg Am 2010;92:338-45.  |
[Table 1], [Table 2], [Table 3]
|
