|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 2
| Issue : 1 | Page : 2-7 |
|
Partner human immunodeficiency virus sero-discordance in Nnewi, Nigeria
Chukwuemeka O Ezeama1, George U Eleje1, Theresa Okonkwo2, Joseph I Ikechebelu1
1 Department of Obstetrics and Gynaecology, PMTCT Unit, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria
2 Department of HIV Care, PMTCT Unit, Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria
| Date of Web Publication | 1-Jul-2014 |
Correspondence Address:
Joseph I Ikechebelu
Department of Obstetrics and Gynaecology, Faculty of Medicine, Nnamdi Azikiwe University, Nnewi Campus, Nnewi
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157 .135741

Context: Disclosing one's human immunodeficiency virus (HIV) status helps in reducing the spread of the disease. Intimate partners are encouraged to reveal their status to each other. Such strategies aid in determining discordance and also target proven interventions to the correct demographic. Objective: The objective was to determine the rates of discordance among HIV positive pregnant women and their partners attending Nnamdi Azikiwe University Teaching Hospital, Nnewi. Materials and Methods: Partners of HIV positive pregnant women who had been notified of their spouses status were invited, counseled, and those who accepted, were tested for HIV using the national testing algorithm. Pre- and post-test counseling was offered to all tested partners. Results: A total of 10,070 new patients booked for antenatal care during the study period. Eight thousand nine hundred and seventy-nine (89.2%) of them were counseled, with 8317 (92.6%) of them accepted to do the HIV test. Seven hundred and ninety-seven women tested positive giving a sero-prevalence of 9.6%. Although 84.4% (673) of the positive mothers stated their intent to notify their partners, only 21% (141) of the partners presented for counseling and testing. On the whole, 98.6% (139) of the partners who presented accepted the test with 45.3% (63) of them testing positive, giving a sero-discordance rate of 54.7%. Conclusion: The discordance rate among tested partners is high in our center and suboptimal counseling, and testing rates were observed in the male partners. Interventions aimed at increasing partner involvement should be devised and adapted for our region. This will yield more data, give a truer picture of discordance rates as well as the aid in better management of scarce resources in program implementation. Keywords: Human immunodeficiency virus, Nnewi, partner, pregnant women, prevention of mother to child transmission, sero-discordance
How to cite this article:
Ezeama CO, Eleje GU, Okonkwo T, Ikechebelu JI. Partner human immunodeficiency virus sero-discordance in Nnewi, Nigeria. J HIV Hum Reprod 2014;2:2-7 |
How to cite this URL:
Ezeama CO, Eleje GU, Okonkwo T, Ikechebelu JI. Partner human immunodeficiency virus sero-discordance in Nnewi, Nigeria. J HIV Hum Reprod [serial online] 2014 [cited 2018 Feb 19];2:2-7. Available from: http://www.j-hhr.org/text.asp?2014/2/1/2/135741 |
| Introduction | |  |
Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) has continued to remain of worldwide interest with several interventions introduced to stem the viral spread. The prevention of mother to child transmission (PMTCT) has been demonstrated to be extremely effective. [1],[2]
For effective PMTCT, both the pregnant mother and her partner should ideally be aware of each other's status, and it appears that many women who are HIV-positive have partners whose HIV status is either negative or unknown. For negative mothers with positive husbands, there is an urgent need to commence health education and implement safer sexual practices, since infection during pregnancy is associated with higher transmission rates to the baby. [3] Furthermore, such practices also help to maintain the partner's negative status.
On the other hand, where there are positive mothers and negative fathers, specific interventions to reduce the fetal/neonatal spread should be immediately implemented, in conjunction with proven practices that help keep the partner negative. However, on many occasions, the status of the partner is unknown. Actively seeking out this information presents a unique opportunity for the couple to share the knowledge of their status and more importantly, for the male partner to use it as an entry point into the HIV prevention program if he eventually tests positive.
Disclosure of one's status is not a task easily undertaken. This is particularly true for the female partner. In an environment that is male dominated, serious and often severe repercussions may follow. [4],[5] However, where there is significant male involvement, this has been shown to positively influence maternal participation in PMTCT programs; thus, interventions targeting the male partner are welcome and urgently needed. [6]
The prevalence of HIV-positive pregnant women in relationships with HIV-negative men in Nnewi Nigeria has not been well-studied. Although some previous studies in Nigeria have examined sero-discordance and disclosure; [7],[8],[9] however, such studies examining these issues in pregnant women have mostly been done outside Nnewi, the study environment. Thus, the "face" of HIV transmission in marital settings in Nigeria expectedly may be different in the various regions of the country.
This study aims to assess the discordance in HIV status among pregnant positive antenatal patients and their partners in our hospital and deduce factors that may affect partner entry into our PMTCT program.
| Materials and methods | |  |
This study was conducted at the PMTCT unit of the Nnamdi Azikiwe University Teaching Hospital (NAUTH) Nnewi from January 2003 to December 2007. NAUTH Nnewi is a university teaching hospital that serves as the major referral center for other public and private health facilities in Anambra state. In addition, it is also one of the hospitals in the country that offers free care and support with respect to HIV prevention and treatment. The center provides free 24-h care for HIV-positive patients. The PMTCT unit is run in conjunction with the Department of Obstetrics and Gynecology, and all consultants are involved. There is, however, a coordinator who oversees all patients' management.
All pregnant women who attend antenatal care in our center are counseled on HIV and subsequently tested using the opt-out approach. The current partners of women who test positive for HIV are routinely asked to visit the hospital for confidential counseling and testing. Separate confidential counseling by hospital staff is offered to the woman and her partner. Confirmed partner HIV test results were used for analysis of partner HIV status and sero-discordance. Couples were considered married if they reported themselves as married according to legal or traditional criteria.
Study design and identification of cases
This study was a retrospective study carried out in NAUTH Nnewi. All patients who had been counseled and tested for HIV were identified from records within the PMTCT department and information regarding the number who accepted the test, the number positive, the number that intended to notify their partners, the number of partners that came for counseling and the number that accepted to test for HIV, and their results were all assessed.
Data analysis
Data were entered into a database using SPSS software version 13 (IBM Inc. Chicago USA). Results are presented as frequencies, percentages, and descriptive statistics.
| Results | |  |
During the study period, 10,070 new antenatal cases were registered of which 8979 (89.2%) of them underwent voluntary counseling and testing. Of these, 8317 women accepted to test for HIV giving an acceptance rate of 92.6% [Table 1]. A total of 797 tested positive giving an HIV sero-prevalence of 9.6% (797/8317).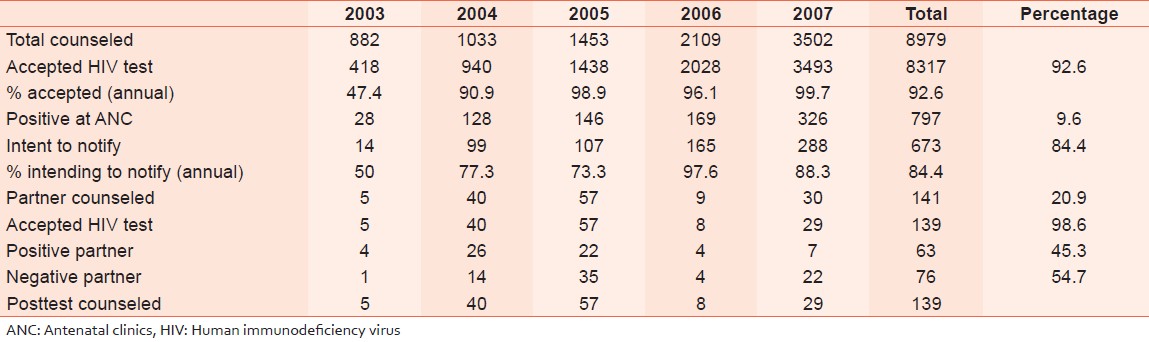 | Table 1: Annual counseling, testing and discordance rates at Nnamdi Azikiwe University Teaching
Hospital (2003-2007)
Click here to view |
A total of 673/8317 (84.4%) intended to notify their partners [Figure 1]; however, only 141/8317 (20.9%) of these partners presented for counseling [Figure 2]. And 139/141 (98.6%) of those counseled accepted to carry out the test [Figure 3]. Seventy-six of the 139 (54.7%) were discordant with their positive pregnant partners [Figure 4].
| Discussion | |  |
Despite many reports on HIV testing of pregnant women in Nigeria, there have been few reports of HIV test results of their partners. We found that among the partners that actually did the HIV testing, 54.7% of HIV-positive women were in sero-discordant relationships. In a previous study in Nigeria by Sagay et al., the city-by-city results showed that in Benin City (Southern Nigeria), 78.8% (104/132) of the partners were HIV negative (sero-discordant), Jos (Middle-Belt) had 48.4% (103/213) sero-discordance while Kano (Northern Nigeria) recorded a sero-discordance of only 7.7% (12/155). [7] However, they concluded that the "different dynamics of HIV transmission in marital settings" in the various regions of Nigeria, including socio-cultural and religious characteristics play a significant role in HIV transmission among couples studied. [7] The mean sero-discordance of 54.7% among HIV-positive mothers whose partners presented for testing seems quite high compared to data from other regions. [10],[11] This should be seen in the light of the actual number that presented for testing. A large majority of women who had indicated interest to disclose did not come with their partners. It, however, gives a baseline for strategy development and implementation.
Over 80% of seropositive women in this study agreed to disclose their HIV status, but only 20.9% of their partners actually presented and were counseled on the test to know their status. Almost all (98.6%) of those counseled accepted to test. Similar low partner involvement was reported by Byamugisha et al., [12] where only 12.5% of male partners presented for voluntary counseling and testing, with a large proportion (40%) of them presenting after the patient had delivered. Although, free HIV counseling and testing were available to any enthusiastic and consenting partner, four reasons may explain why small proportion of men agreed to be counseled for HIV testing in the first place: [13] The reasons are, the fear of discovering HIV seropositivity and subsequent stigmatization; the need to personally and actively request HIV testing (unlike pregnant women, who were offered HIV counseling and testing during antenatal care); the belief that couples cannot be HIV sero-discordant; and some partners already knew their status and subsequently saw no reason to further present at a hospital. Our finding was also similar to a study by Maman et al. in Tanzania where only 16% of partners informed of their wife's HIV status agreed to go for testing. [14] However, it is important to note that in relationships where disclosure has not occurred or the partner has not been tested present a major challenge to PMTCT as it makes the processes of counseling complex and may constitute an additional burden of HIV on the family unit. Interestingly, in our hospital, HIV positive pregnant women and their partners were counseled separately and before being offered joint counseling; both concordant and sero-discordant couples were strongly encouraged to discuss results to each other.
The sero-prevalence of HIV has increased steadily in pregnant women in Nnewi. The hospital prevalence data as seen in this study are based on routine counseling and testing of about 8979 pregnant women. It is our strong belief that they are dependable indicators of HIV prevalence for the general antenatal population. During the 5 years study period, antenatal clinic HIV sero-prevalence increased from 6.7% to 9.6%. Surprisingly, our findings are not consistent with national surveillance data. For example, the Federal Government has released the 2012 National HIV/AIDS and Reproductive Health Survey-Plus, which indicates that Nigeria now has HIV prevalence rate of 3.4% [15] compared with 5% in 2003 and 4.4% in 2007. [16] Thus, sero-prevalence rates for antenatal women are thought to reflect most closely the rates in the general population. However, our data show that prevalence in antenatal women was on the increase. One explanation, suggested by our study, is that young women may have partners several years older than themselves. Thus, prevalence in antenatal women may increase for several years before reflecting falling prevalence rates in the general population. Another reason may be the status of the study hospital as one of the national PMTCT sites, where management and treatment of HIV-positive patients is done free of charge. This thus attracts a larger number of positive patients resulting in the higher prevalence noted.
During the study period, 10,070 new antenatal cases were registered of which 8979 (89.2%) of them underwent voluntary counseling and testing. This shows a high counseling coverage. Integrating counseling and testing into programs aimed at reducing HIV spread is recommended by WHO. [9] However, the rates of counseling and testing, documented over the 5 years period show a consistent rising trend. As observed in this study, initial low rates of counseling could be attributed to poor knowledge and experience at the onset of the program in our center. Subsequently, with better capacity and experience among the counselors more coverage was expectedly recorded. Furthermore, the general awareness of HIV among the population increased, and this may have impacted positively on the counseling.
The testing rates parallel the counseling rates in that as more women were counseled, many more of them accepted to avail themselves of the test using our opt out approach to testing. More than 95% of those counseled eventually did get tested, and these rates are comparable with those noted in an Ugandian study [12] where up to 95% testing uptake was noted once counseling was optimized. These further buttresses the fact that routine counseling and testing, when incorporated into traditional antenatal care clinics, actually helps increase the identification of patients who will need further intervention in the index pregnancy.
A number of women may have declined to disclose their status to their husbands for fear of repercussions. There are several documented cases of severe abuse (physical, financial, and psychological), experienced by women consequent to their disclosure. [3],[4] The patriarchal nature of our society coupled with the harsh financial realities evident today in a very weak social services system potentiates the real fears with respect to such disclosure among women.
Once the partners presented to the hospital, however, all accepted counseling with 98.6% undergoing testing thus implying that rates of partner counseling and testing can be augmented if more effective methods of partner disclosure can be developed. These methods should be safer for the women and may need the presence of the healthcare provider at times to aid them in their intent to disclose.
This study is one of the few ones that had examined sero-discordance and disclosure in HIV-positive pregnant women to their partners in Nigeria. Notwithstanding, the limitations of this study must be recognized. This study is retrospective and relied on information obtained from the medical record, including self-reported information provided by the HIV-positive pregnant woman to the healthcare provider. As with all self-reported information, the potential exists for biases because of the sensitive nature of the topic. The demographic and behavioral risk profiles of HIV-positive antenatal women were not studied and there was lack of data about the use of HIV transmission prevention measures while trying to conceive. There were some missing data and unavailability of demographic data in the records may also have impacted strongly on the study findings. Finally, although we observed a high rate of sero-discordance in our clinic population, these findings may not be generalizable to other regions of Nigeria in line with previous published study. [7]
| Conclusion | |  |
This study revealed that HIV sero-discordant relationships were common in our antenatal clinic population and sero-prevalence appears to be rising in Nnewi, Nigeria. Approximately, one out of every two couples in our tested series had evidence of discordance. Although optimal intended disclosure rates were observed, suboptimal testing rates were observed in the partners. Further research is needed to evaluate the rising sero-prevalence and factors determining the sero-discordance including ground-breaking interventions in order to improve involvement of male partner. Programs that empower women to disclose their status effectively should be pursued, and integral to these programs should be social services available to such women in the event of abuse from their partners. Male partner involvement should be emphasized from the onset of pregnancy as this may encourage their attendance to the antenatal clinic and subsequent counseling and testing.
| References | |  |
| 1. | Nacius LA, Levison J, Minard CG, Fasser C, Davila JA. Serodiscordance and disclosure among HIV-positive pregnant women in the Southwestern United States. AIDS Patient Care STDS 2013;27:242-7. 
|
| 2. | Mnyani CN, McIntyre JA. Preventing mother-to-child transmission of HIV. BJOG 2009;116 Suppl 1:71-6. 
|
| 3. | Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: Implications for prevention of mother-to-child transmission programmes. Bull World Health Organ 2004;82:299-307. 
|
| 4. | Armistead L, Morse E, Forehan, R, Morse P, Clark L. African American women and self-disclosure of HIV-infection: Rates, predictors, and relationship to depressive symptomatology. AIDS Behav 1999;3:195-204. 
|
| 5. | Lester P, Partridge JC, Chesney MA, Cooke M. The consequences of a positive prenatal HIV antibody test for women. J Acquir Immune Defic Syndr Hum Retrovirol 1995;10:341-9. 
|
| 6. | Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr 2004;37:1620-6. 
|
| 7. | Sagay AS, Onakewhor J, Galadanci H, Emuveyan EE. HIV status of partners of HIV positive pregnant women in different regions of Nigeria: Matters arising. Afr J Med Med Sci 2006;35 Suppl: 125-9. 
|
| 8. | Olagbuji BN, Ezeanochie MC, Agholor KN, Olagbuji YW, Ande AB, Okonofua FE. Spousal disclosure of HIV serostatus among women attending antenatal care in urban Nigeria. J Obstet Gynaecol 2011;31:486-8. 
|
| 9. | Sagay AS, Musa J, Ekwempu CC, Imade GE, Babalola A, Daniyan G, et al. Partner disclosure of HIV status among HIV positive mothers in Northern Nigeria. Afr J Med Med Sci 2006;35 Suppl: 119-23. 
|
| 10. | Msuya SE, Mbizvo EM, Hussain A, Uriyo J, Sam NE, Stray-Pedersen B. Low male partner participation in antenatal HIV counselling and testing in northern Tanzania: Implications for preventive programs. AIDS Care 2008;20:700-9. 
|
| 11. | McKenna SL, Muyinda GK, Roth D, Mwali M, Ng'andu N, Myrick A, et al. Rapid HIV testing and counseling for voluntary testing centers in Africa. AIDS 1997;11 Suppl 1:S103-10. 
|
| 12. | Byamugisha R, Tylleskär T, Kagawa MN, Onyango S, Karamagi CA, Tumwine JK. Dramatic and sustained increase in HIV-testing rates among antenatal attendees in Eastern Uganda after a policy change from voluntary counselling and testing to routine counselling and testing for HIV: A retrospective analysis of hospital records, 2002-2009. BMC Health Serv Res 2010;10:290. 
|
| 13. | Brou H, Agbo H, Desgrees Du Loû A. Impact of HIV counseling and testing during antenal consultation for HIV- women in Abidjan (Côte d'Ivoire): A quantitative and qualitative study (Ditrame Plus 3 project, ANRS 1253). Sante 2005;15:81-91. 
|
| 14. | Maman S, Mbwambo J, Hogan M, Kilonzo G, Sweat M, Weiss E. HIV and Partner Violence: Implications for HIV Voluntary Counselling and Testing Programs in Dar es Salaam, Tanzania. Washington, (D. C.): Horizon, USAID, Population Council; 2001. p. 35. 
|
| 15. | Olokor F. Rivers has highest HIV/AIDS rate-FG. Available from: http://www.punchng.com/news/rivers. [Last accessed on 2014 Jun 09]. 
|
| 16. | UNAIDS/WHO. UNAIDS/WHO Policy Statement on HIV Testing. Geneva; 2004. Available from: http://www.unhcr.org/4b508b9c9.pdf. [Last accessed on 2014 Jun 09]. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1]
|