|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 3
| Issue : 1 | Page : 1-6 |
|
Human immunodeficiency virus-positive women: Pregnancy, delivery outcomes, and complications at the Korle-Bu Teaching Hospital in Accra, Ghana
Joseph D Seffah1, RA Kwame-Aryee1, Richard M.K Adanu1, Lorna A Renner2, Margaret Lartey3
1 Department of Obstetrics and Gynaecology, University of Medical School, Accra, Ghana
2 Department of Child Health, University of Medical School, Accra, Ghana
3 Department of Medicine and Therapeutics, University of Medical School, Accra, Ghana
| Date of Web Publication | 9-Nov-2015 |
Correspondence Address:
Joseph D Seffah
Department of Obstetrics and Gynaecology, University of Ghana Medical School, P. O. Box 4236, Accra
Ghana
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157.169178

Objective: To study the delivery outcomes and complications associated with human immunodeficiency virus (HIV) positive women. Patients and Methods: A clinical audit from January 2006 to December 2009 involving patients accessing antenatal and delivery services at the Korle-Bu Teaching Hospital and using the voluntary counseling and testing/prevention of mother-to-child transmission services. Results:. HIV-positive women on the highly active antiretroviral therapy and ART prophylaxis had a mean CD4 count of 681 cells/ul (range: 412–810). Those who were not on any prophylaxis had a mean count of 288 cells/ul (range: 34–601). The study and comparison populations had similar mean ages; 29.8 years and 28.4 years, respectively (P = 0.09). About half the HIV-positive women had vaginal delivery though none had an episiotomy, forceps, or vacuum delivery. The HIV-positive women had a caesarean section rate of 55% and the rate in the HIV-negative women was 21% (P < 0.001). About 50% of the caesarean deliveries were done as emergencies. The mean birth weight was lower in the HIV-positive women; 2.9 kg versus 3.1 kg, respectively (P = 0.08). The perinatal losses were significantly higher in the study population; 95 versus 70 (P = 0.04). The mean placenta weight was smaller in the study population; 510 g versus 550 g (P = 0.04). Conclusion: Among the HIV-positive parturient, the caesarean delivery rate was about 50% and the neonatal outcomes were significantly worse than in the HIV-negative women.
Keywords: Complications, delivery, human immunodeficiency virus positive, pregnancy
How to cite this article:
Seffah JD, Kwame-Aryee R A, Adanu RM, Renner LA, Lartey M. Human immunodeficiency virus-positive women: Pregnancy, delivery outcomes, and complications at the Korle-Bu Teaching Hospital in Accra, Ghana. J HIV Hum Reprod 2015;3:1-6 |
How to cite this URL:
Seffah JD, Kwame-Aryee R A, Adanu RM, Renner LA, Lartey M. Human immunodeficiency virus-positive women: Pregnancy, delivery outcomes, and complications at the Korle-Bu Teaching Hospital in Accra, Ghana. J HIV Hum Reprod [serial online] 2015 [cited 2018 Aug 6];3:1-6. Available from: http://www.j-hhr.org/text.asp?2015/3/1/1/169178 |
| Introduction | |  |
Globally about 420,000 children are infected with human immunodeficiency virus (HIV) annually and 90% of the infection occurs in the sub-Saharan Africa.[1] The children are infected during the antenatal and intrapartum periods or in the course of breastfeeding. Most exposure to the newborn occurs during labor and delivery when there is a micro transfusion of the virus during uterine contractions.[2] Maternal cervicovaginal secretions and blood at delivery could also be the media of transmission.[2]
The prevention of vertical transmission of the HIV from the mother to the fetus or newborn is a major objective in modern obstetric care and this is captured in the Millennium Development Goal No. 6 of the UN which seeks among other things to combat the transmission and reverse the trend of infections by 2015.[3]
The methods adopted to reduce vertical transmission include treatment of the mother with highly active antiretroviral therapy (HAART) or ART prophylaxis consisting of zidovudine and lamivudine during pregnancy and labor, and administering the drug to the neonate for the first 6 weeks after birth. The use of zidovudine to the mother and neonate reduces the transmission rate from 25% to 8%.[4]
Elective caesarean section reduces the rate of vertical transmission compared with emergency caesarean section or a vaginal delivery, and this is true whether or not the patient is on HAART or ART prophylaxis.[5]
At maternal plasma viral load of <1000 copies/ml, vertical transmission is near zero.[5],[6] This state can be achieved by the use of HAART. However, the benefit of the caesarean section to the woman on HAART or to women with low or undetectable maternal viral load is not well-documented in Ghana. In our setting where the women with prior caesarean section may be reluctant to deliver at the hospital because of fear of another caesarean section for a future delivery, the use of primary caesarean section for the prevention of vertical transmission of HIV should be carefully weighed.
In 2008, about 257,466 pregnant women in Ghana underwent voluntary counseling and testing (VCT) and 6021 of these women constituting 2.3% were HIV positive. About 83% of the HIV-positive women were given HAART or ARTs as prophylaxis after 28 weeks of pregnancy.[7],[8],[9]
The objective of this study was to find out the outcomes of delivery and complications associated with the HIV-positive women as compared with the HIV-negative women who delivered at the same time at the Korle-Bu Teaching Hospital in Accra, Ghana (KBTH).
| Patients and Methods | |  |
This was a clinical audit involving women who delivered between January 2006 and December 2009 at the KBTH.
The KBTH delivers about 12,000 women every year. Since May 2004, the KBTH has had a VCT/prevention of mother-to-child transmission (PMTCT) center that supervises the care of the HIV-positive pregnant women. The center works in close collaboration with the National AIDS/STI Control Program of Ghana. There are dedicated HIV counselors among the hospital staff: Doctors, nurses, pharmacists, and laboratory technicians. Testing for the HIV is done with two rapid ELISA tests, and a patient is declared reactive when both tests are positive. When only one rapid test shows a positive result, then the patient has to be sent to the Public Health Reference Laboratory at the KBTH for a confirmatory test. The CD4 counts are determined (as described by SACS caliber by BD) and the patients whose counts are below 350 cells/ul are administered the HAART, while those whose counts are above 350 cells/ul are administered with the prophylaxis. The protocol for the management of these patients has undergone frequent modifications with our increasing knowledge about the infection.
PMTCT practice at KBTH usually follows national guidelines. Since 2007 women can opt out of testing after counseling. Since 2007, women have been put on HAART consisting of three drugs if they met the criteria, but otherwise zidovudine and lamivudine were given to them from 28 weeks pregnancy till delivery with nevirapine being given in labor. Babies are given nevirapine at birth and zidovudine and lamivudine for 1–6 weeks depending on the duration of maternal prophylaxis. Before 2007 women were put on single-dose nevirapine when in labor and the same drug was given to the babies within 48 h of delivery. Counseling and laboratory testing for CD4 counts, provision of medications, and monitoring of pregnancy and labor are some of the areas that have improved considerably. Some of the patients have been on the HAART before they become pregnant, and these are allowed to continue with their medications consisting of zidovudine, lamivudine, and nevirapine.
A number of women, however, are given only nevirapine during labor when they have been diagnosed late in pregnancy. Their babies are given nevirapine syrup at birth. The women continue with their treatment at the Fevers unit of the KBTH where there are physicians and a dedicated staff while the babies are followed up by the pediatricians at the Department of Child Health, also at the KBTH.
In this study, the records of HIV-infected women who consecutively delivered at the KBTH during the period of study were included. For every HIV-positive woman who was selected, three HIV-negative women who delivered immediately after her were also selected for comparison. For each woman, either in the study or control group, the following data were obtained from the VCT/PMCT unit, labor wards and from their postnatal records: The age, parity, CD4 cell count, mode of delivery, sex and weight of baby, Apgar scores, placental weight, duration of stay at hospital, evidence of wound infection establishment of breastfeeding, Neonatal Intensive Care Unit (NICU) admissions, and maternal and perinatal mortality and morbidity.
Excluded from the study were women with incomplete delivery records. Permission to do the study was obtained from the administration of the Department of Obstetrics and Gynaecology.
As expected the sample size of 300 for the study population (HIV-positive) was based on the estimated HIV prevalence in the population of 4%, a confidence interval of 95%, a 5% acceptable margin of error, and the need for a sample size large enough to enable analysis. For each HIV-positive woman, three HIV-negative women were selected as control.
Ethical clearance for this study was obtained from the Ethical and Protocol Committee of the University of Ghana Medical School.
Statistical analysis
The data were entered into SPSS version 20 (IBM Chicago). Descriptive statistics were used for the two groups, case and control.
For the differences between the means of the two groups, the Student's t-test was used. For comparison of proportions, the Chi-square test was used, and a value of < 0.05 was taken as significant.
| Results | |  |
The clinical records of 300 HIV-positive women and 900 HIV-negative women were examined out of which 275 and 810, respectively, were selected for analysis.
The CD4 counts for the pregnant women who were on only prophylactic ART ranged between 462 and 810 cells/ul with a mean of 681 cells/ul while the CD4 count ranged between 34 and 601 cells/ul with a mean of 288 cells/ul for those on HAART during pregnancy. None of the pregnant women had the viral load test run for her.
The mean ages of the two groups were similar, but the mean parities differed slightly [Table 1].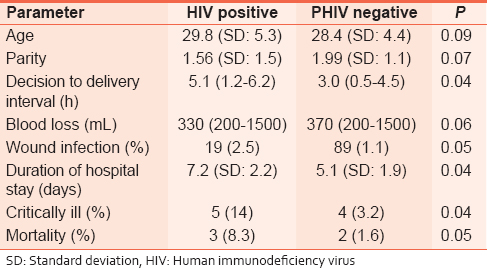 | Table 1: Comparison of demographic and delivery characteristics of HIV positive and HIV negative women
Click here to view |
This study showed caesarean section rate of 55% in the HIV-positive women who had care at the KBTH. The comparative figure for the HIV-negative women was 21%, and the difference was significant [Table 1] [Table 2] [Table 3].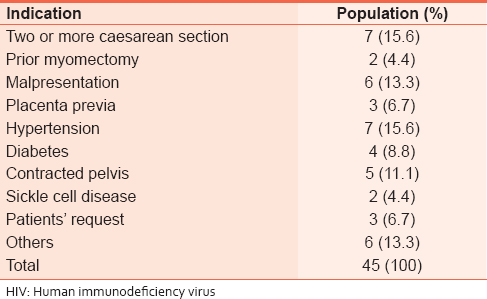 | Table 2: Indications for elective caesarean section in HIV--negative women
Click here to view |
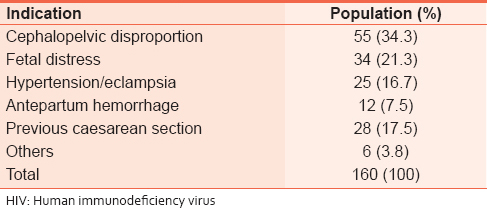 | Table 3: Indications for emergency caesarean section in HIV--negative women
Click here to view |
Out of the total of 275 HIV-positive women, 74 (27%) had elective caesarean delivery. 201 (73%) women went into labor resulting in 124 (45%) vaginal deliveries and 77 (28%) emergency caesarean sections.
Elective caesarean section was done for the HIV-positive women mostly because of choice by the women themselves. Other indications for elective CS were associated with the HIV status [Table 4]. The indications for emergency caesarean section in the 77 HIV-positive women were: HIV-positive women in labor, 37 (53%); cephalopelvic disproportion, 21 (27%); fetal distress, 12 (16%); and eclampsia, 7 (9%).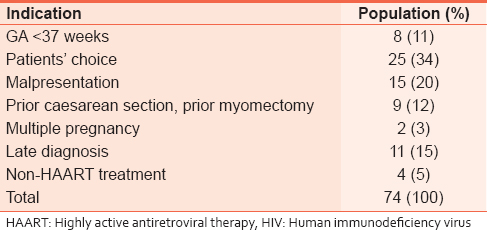 | Table 4: Indications for elective caesarean section for HIV--positive women
Click here to view |
Vaginal delivery was performed for 124 HIV-positive women [Table 5]. However, vacuum extraction, forceps delivery, induction of labor, and episiotomy were not performed for any of them.
In the HIV-negative women, the indications for the elective caesarean section were for obstetric reasons only and included: Prior caesarean section, prior myomectomy, and malpresentation. The emergency caesarean sections were done mostly for cephalopelvic disproportion and fetal distress.
The decision-to-delivery interval was significantly longer for the HIV-positive parturient. The mean blood loss at vaginal delivery was less in the HIV-positive women. Wound infection was more common in the HIV-positive women. There was a higher percentage of the critically ill, and the period of hospital stay was longer in the HIV-positive women.
The birth weight was lower in the HIV-positive and so was the mean placental weight [Table 6]. The Apgar scores at 5 min were lower, and the perinatal mortality was higher in neonates whose mothers were HIV-positive.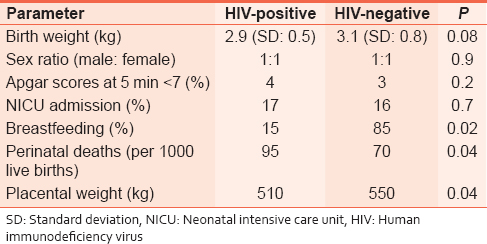 | Table 6: Comparison of neonatal characteristics of babies delivered by HIV--positive and HIV--negative mothers
Click here to view |
The indications for NICU admissions included simply babies delivered to HIV positive mothers, prematurity, respiratory distress syndrome, and sepsis. The percentage of babies who were breastfeeding at 2 weeks postdelivery was significantly lower in the HIV-positive population.
| Discussion | |  |
This clinical audit involved 275 HIV-positive and 810 HIV-negative women who were delivered at the Korle-Bu Teaching Hospital over a 4-year period from January 2006 to December 2009.
There was no significant difference between the mean ages of the HIV-positive and HIV-negative women. This might be attributed to the fact that the two groups were drawn from the same population at the KBTH. However, the parity of the two groups differed slightly.
ART was administered to HIV-positive pregnant women at KBTH as this was indicated. HAART is known to reduce the rate of progression of the disease in the advanced state.[10],[11] Pregnant women with CD4 count of <350 cells/ul were considered for the HAART at the KBTH. This approach has been recommended after the first trimester although it is known to be administered even in the first trimester at some centers.[10],[11]
The patients chose their preferred mode of delivery after counseling at the VCT/PMTCT center. Some women on the HAART chose to deliver vaginally even though their viral load had not been determined.
Some patients were admitted late in labor. Delay in deciding to come to the hospital and delay in securing a means of transportation have been some of the reasons given but it might be true that some of these women wanted to have vaginal delivery by all means. Future studies would be done to find out if the HIV-infected and uninfected women differ in these attitudes.
In the current study at KBTH, no woman opted for vaginal delivery because her viral load was lesser than 1000 copies/ml. The test was too expensive for the patients. It would have been desirable to have estimated the viral load for the women who had been on HAART to determine the viral load and then counsel them for a vaginal delivery. This approach would have reduced the caesarean section rate in this group. And better still, if all were to have the HAART, probably caesarean section will be done only for obstetric indications.[12],[13],[14]
The caesarean section rate was more than twice in the HIV-positive group compared with the control group. The rate for elective caesarean section was much higher, and the indications were different. While HIV-positive patients had surgery just because they were infected with the virus, the HIV-negative patients had a caesarean section for obstetric indications only.
The patients' choice was the main indication for elective caesarean section in the study population, but this was a rare indication for the comparison population. However, the main indications for elective caesarean section in the comparison population were: A history of two or more previous caesarean section, prior myomectomy, malpresentation, and hypertension.
In the HIV-positive women, no assisted vaginal delivery was performed with vacuum extraction or forceps delivery and no episiotomy was performed, and this was for the prevention of vertical transmission as has been well-documented.
The decision to deliver the HIV-positive women at a gestation of <37 weeks was because of the intercurrent medical conditions such as hypertension and intrauterine growth restriction and not as a result of the positive serology perse.
The decision-to-delivery interval was much longer in the HIV-positive women who required emergency caesarean section. This might have been due to the attitude of the operating room staff in the selection of HIV-negative over the HIV-positive patients when the theater space and resources were limited.
The wound infection rate was about twice in the HIV-infected women. This was despite the antibiotic cover given to all the women with HIV infection. This might be a reflection of the immune status of the women as evidenced by the CD4 cell count.
The mean blood loss in the HIV-positive women who delivered vaginally was lower, and this was likely to be due to the avoidance of instrumentation and episiotomy. However, since the caesarean section rate was about twice the rate in the HIV-positive women the total blood loss due to caesarean delivery in the study population was expected to be much higher.
Four HIV-negative patients needed the ICU services to survive, and there were two maternal mortalities due to eclampsia.
Five HIV-positive patients were so ill after their delivery that they had to be transferred to the Fevers Unit where three died. They did not have the ICU facilities since these were out of order at the time of the study.
The mean birth weight of the babies was lower for the HIV-positive women. Correspondingly, the mean placenta weight was smaller. Nutrition and oxygen delivery might have been lower in the HIV-positive women.
The perinatal losses were higher in the HIV-positive women. However, statistics from the pediatricians at the KBTH show that the babies do well and the HIV transmission rate has been about 4% in babies delivered by the mothers who had been on the ART and about 25–40% in babies whose mothers were HIV positive but were not on any ART.[15],[16]
Breastfeeding is universally encouraged in the postpartum mother in Ghana, and this was evident from the result in the HIV-negative mothers. The HIV-positive women were to breastfeed exclusively for the first 6 months after delivery, but the finding from the study suggested that only about 15% did so. The mothers were using formula feeds instead although they had been told about the risk of diarrhea in the children. They might have done this to prevent vertical transmission through breastfeeding.
It can be envisaged that if it becomes practicable to administer HAART to all pregnant women as early as possible, then vaginal delivery and breastfeeding could be encouraged more widely.
Limitations of the study
The study involved the use of case notes which were sometimes incompletely or poorly recorded. Some of the patients too had been lost to follow-up. Some biases were inherent in the sampling of case notes for study.
The protocol for the PMTCT has always undergone frequent revisions, and therefore, it was difficult to assign an outcome of management to a particular protocol.
| Conclusion and Recommendation | |  |
- Caesarean section rate is very high among the HIV-positive mothers seeking care at the KBTH
- Scaling up of the HAART in the hospital would increase the proportion of women who present for delivery with probably a low viral load even when this has not been confirmed by laboratory studies
- A vaginal delivery could be tried for the women who have had adequate treatment with the HAART
- Vaginal delivery would reduce the morbidity associated with caesarean delivery and also prevent a future catastrophe such as rupture of the uterus in the HIV-positive women with a scarred uterus
- Mothers on the HAART for a long period may be encouraged to breastfeed since the HIV transmission rate is very low
- A prospective study of the relationship between the duration of the HAART administration and the viral load in the pregnant Ghanaian women should be undertaken. This is to find out the minimum duration of therapy that would ensure safe vaginal delivery for the HIV-positive women
- Health education and improved antenatal coverage for all pregnant women and the scaling up of PMTCT in our heath institutions would prevent late presentation of the pregnant women, decrease the caesarean section rate and then decrease the high infection rate in the children.
| Acknowledgment | |  |
We are grateful to the counselors at the Department of Obstetrics and Gynaecology of the KBTH especially Ms. Joyce Dodoo and Sheila Boateng Gyasi, the Principal Nursing Officers in charge of the VCT-PMCT Unit. We are also grateful to all the other health personnel at the Departments of Obstetrics/Gynaecology, and Child Health and the Fevers Unit of the KBTH, who helped in managing these patients.
| References | |  |
| 1. | Guidozzi F, Black V. The obstetric face and challenge of HIV/AIDS. Clin Obstet Gynecol 2009;52:270-84.  |
| 2. | Bouchet M, Cohen HR, Gruslin A, Money D, Sreben M, Wong T. Mode of delivery for pregnant women infected by the human immunodeficiency virus. SOGC Clinical Practice Guidelines. No. 1. Vol. 101. Public Health, Agency of Canada; 2001. p. 1-3.  |
| 3. | |
| 4. | Connor EM, Sperling RS, Gelber R, Kiselev P, Scott G, O'Sullivan MJ, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med 1994;331:1173-80.  |
| 5. | European Mode of Delivery Collaboration. Elective caesarean-section versus vaginal delivery in prevention of vertical HIV-1 transmission: A randomised clinical trial. Lancet 1999;353:1035-9.  [ PUBMED] |
| 6. | European Collaborative Study. Mother-to-child transmission of HIV infection in the era of highly active antiretroviral therapy. Clin Infect Dis 2005;40:458-65.  [ PUBMED] |
| 7. | 2009 HIV Sentinel Survey Report. National AIDS/STI Control Programme Ghana Health Service, Ministry of Health, Accra, Ghana; 2009.  |
| 8. | 2008 Annual Report. National Aids/STI Control Programme, Ghana; 2008.  |
| 9. | |
| 10. | Suy A, Hernandez S, Thorne C, Lonca M, Lopez M, Coll O. Current guidelines on management of HIV-infected pregnant women: Impact on mode of delivery. Eur J Obstet Gynecol Reprod Biol 2008;139:127-32.  |
| 11. | Scheduled Caesarean Delivery and the prevention of vertical transmission of HIV infection. ACOG Committee on Obstetric practice. No. 234. May, 2000. p. 1-3.  |
| 12. | UNAIDS. Report on the Global AIDS Epidemic. Geneva: UNAIDS; 2004.  |
| 13. | WHO/UNAIDS/UNICEF. Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector. Geneva: WHO/UNAIDS/UNICEF; 2010.  |
| 14. | Badri M, Bekker LG, Orrell C, Pitt J, Cilliers F, Wood R. Initiating highly active antiretroviral therapy in sub-Saharan Africa: An assessment of the revised World Health Organization scaling-up guidelines. AIDS 2004;18:1159-68.  |
| 15. | Statistics from Dept of Child Health, Korle Bu Teaching Hospital, Accra; 2006-2009. [Unpublished data].  |
| 16. | Ampofo WK. Current status of HIV/AIDS treatment, care and support services in Ghana. Ghana Med J 2009;43:142-3.  |
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5], [Table 6]
|