|
 
 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 3
| Issue : 1 | Page : 20-22 |
|
Pancreatic tuberculous abscess mimicking as cystic neoplasm: A rare initial manifestation of AIDS-defining illness
Chanabasappa V Chavadi1, Swetha Kory2, Pallavi Rao1, Ajit Mahale3
1 Department of Radiodiagnosis, Kasturba Medical College, Manipal University, Manipal, Karnataka, India
2 Department of Pathology, Yenepoya Medical College, Mangalore, Karnataka, India
3 Department of Radiodiagnosis, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India
| Date of Web Publication | 9-Nov-2015 |
Correspondence Address:
Chanabasappa V Chavadi
Flat No C-1-13 (Third Floor), KMC, Staff Quarters, Light House Hill Road, Mangalore - 575 001, Karnataka
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157.169175

A pancreatic tuberculous abscess is extremely rare, considered to be an AIDS-defining illness in HIV-positive patients. It is even rare to present as an initial manifestation of AIDS. We present a case that presented with epigastric pain, fever, and reduced appetite. The cystic pancreatic lesion was identified and computed tomography-guided fine needle aspiration proved it to be a tuberculous abscess, confirmed by demonstration of acid fact bacilli in the pus aspirated. Although rare, it must be considered in the differentials in HIV-positive patients and can be confirmed by minimally invasive image-guided aspiration with microbiological or histopathological evaluation. Etiopathogenesis, presentation, and review of the literature is been summarized.
Keywords: Computed tomography, fine needle aspiration, pancreas, tuberculous abscess
How to cite this article:
Chavadi CV, Kory S, Rao P, Mahale A. Pancreatic tuberculous abscess mimicking as cystic neoplasm: A rare initial manifestation of AIDS-defining illness. J HIV Hum Reprod 2015;3:20-2 |
How to cite this URL:
Chavadi CV, Kory S, Rao P, Mahale A. Pancreatic tuberculous abscess mimicking as cystic neoplasm: A rare initial manifestation of AIDS-defining illness. J HIV Hum Reprod [serial online] 2015 [cited 2018 Aug 6];3:20-2. Available from: http://www.j-hhr.org/text.asp?2015/3/1/20/169175 |
| Introduction | |  |
Isolated pancreatic involvement by mycobacterium tuberculosis (TB) is extremely rare, implicated by the inherent protection offered by the pancreatic enzymes.[1],[2] Only 10 cases of pancreatic TB have been reported in the literature from India in last 5 years.[3] It is considered to be an AIDS-defining illness in HIV-positive patients, but there are very few case reports as the first manifestation. We present a case of cystic pancreatic lesion identified on imaging, wherein computed tomography (CT)-guided fine needle aspiration (FNA) followed by pus drainage was performed, and microscopy of pus demonstrated acid fact bacilli (AFB).
| Case Report | |  |
A 39-year-old man presented with epigastric pain, fever, reduced appetite since 2 months. The abdomen was soft without any palpable mass, auscultation of chest revealed normal breath sound. There was no cough, and chest radiograph was normal. Clinical examination of other systems was unremarkable. Laboratory findings included liver function tests, serum amylase was 80 U/L and lipase was 110 U/L, and random blood sugar was 110 mg/dl being in normal range. Ca19-9 was 3 U/ml, Tn-T - 0.01ng/ml fundus examination-normal. Blood culture revealed no growth. Hemoglobin - 9.5g/dl, total count - 6000 cells/µL, erythrocyte sedimentation rate (ESR) -98 mm/h, peripheral blood smear microcytic hypochromic anemia with few elliptocytes, and toxic granules. HIV-positive and C-reactive protein were 228 mg/L.
Ultrasonography (USG) of the abdomen was performed, which revealed a hypoechoic lesion with cystic components in the region of the pancreas. CT demonstrated a predominantly cystic lesion without internal enhancement in the pancreas [Figure 1]c, the splenic artery was noted within the lesion. Multiple peripancreatic and adjacent retroperitoneal lymph nodes with central nonenhancing component were identified [Figure 1]d. No mass effect, biliary dilatation or thrombosis of blood vessels. A pancreatic pseudocyst seemed unlikely in a clinical context and with the absence of previous pancreatitis. Imaging features prompted a possible diagnosis of pancreatic cystadenoma. CT guided aspiration was performed [Figure 2]a, which was uneventful; after aspiration of the lesion, near the complete reduction in size was achieved and became inconspicuous [Figure 2]b. About 60 ml of purulent, turbid fluid was aspirated. Microscopy of pus revealed numerous AFB with Ziehl-Neelsen Stain [Figure 2]c and [Figure 2]d. AFB culture with Lowenstein Jensen medium was also positive. The patient improved clinically on anti-tuberculosis (ATT) medications: Ethambutol, isoniazid, pyrazinamide, and rifampin for 3 months. A repeat USG after 3 months of ATT medication revealed no evidence of the pancreatic lesion.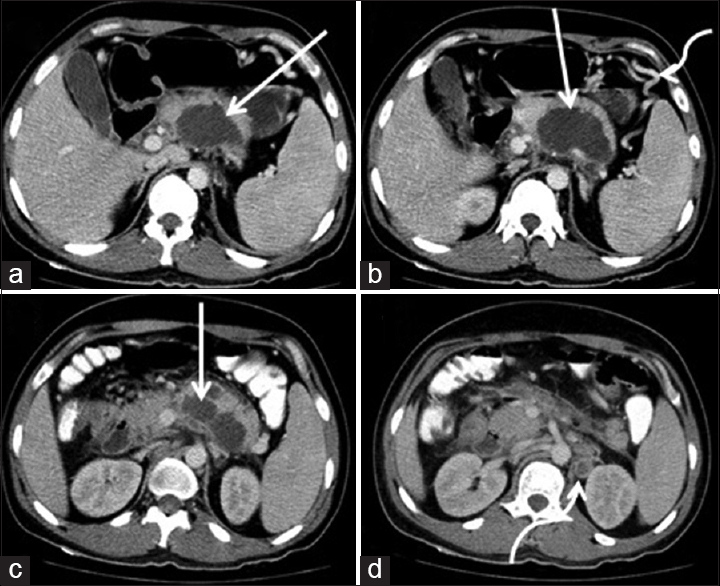 | Figure 1: Axial section computed tomography demonstrates nonenhancing cystic lesion in the pancreas with ill-defined margins (straight white arrow a, b, and c). Enlarged lymph nodes in the left para-aortic region with central necrotic component (curved white arrow in d). Collateral vessels (curved white arrow in b) secondary to narrowing of splenic vein
Click here to view |
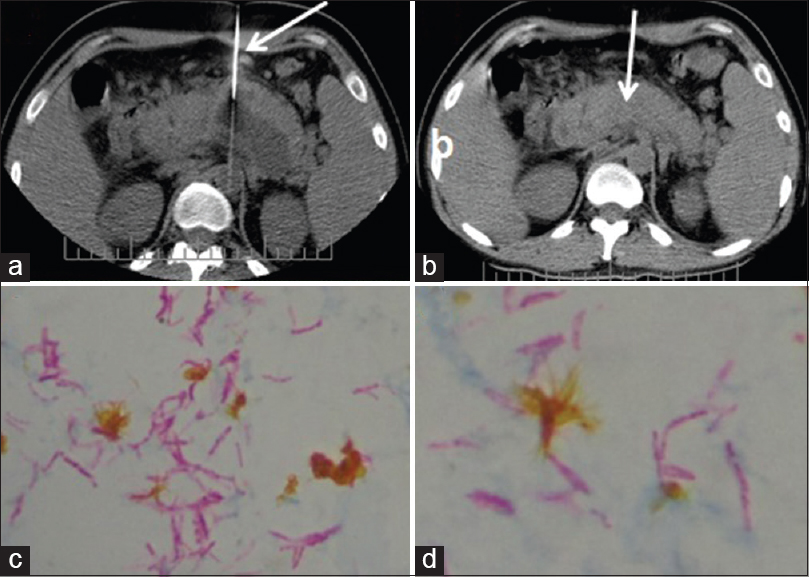 | Figure 2: Computed tomography FNA performed with spinal puncture needle (straight white arrow a). After computed tomography guided aspiration drainage, near complete resolution of the collection, was confirmed (straight arrow in b). Microscopy of pus aspirate in Ziehl-Neelsen Stain demonstrates numerous acid fact bacilli (c and d)
Click here to view |
| Discussion | |  |
In 1977, Bhansali reported on 300 cases of abdominal TB. There were no cases of pancreatic TB.[4] TB of Abdomen is seen affecting commonly the spleen, liver, ileocecal region, and peritoneum.[5] TB of the pancreas is considered a rare entity, usually occurring in the setting of HIV infection or immunosuppression. The etiopathogenesis of pancreatic TB proposed include - secondary to miliary disease, hematogenous dissemination, or direct spread from contiguous lymph nodes.[5] Regional lymph nodes with central necrosis and peripheral enhancement were noted, in this case, supporting this popular hypothesis.
In a review of the literature, we observed that pancreatic TB was frequently diagnosed by a surgical approach, either by laparotomy or laparoscopy, justified by the very fact that it closely resembles malignancy. Image guidance used for diagnosis included USG, endoscopic USG (EUS), and CT. In only three reports, it was the initial manifestation of AIDS.
Clinical characteristics of pancreatic TB remain unclear. Common presentation is abdominal pain, weight loss, anemia, night sweats, and elevated ESR with lymphopenia.[6],[7] Our patient had abdominal pain, anemia, night sweats, and elevated ESR, which was a clue for an infective process.
The differentials for cystic lesions of the pancreas are pseudocysts, cystic neoplasms, lymphoepithelial cyst, abscess, and metastasis. Pancreatic TB can be diagnosed with the help of EUS or CT-guided FNA, thereby obviating the necessity for surgery.[8] It can be effectively treated with ATT drugs. In a review of 51 case reports in the literature by Demir et al., seven were diagnosed by CT-guided FNA and 44 underwent diagnostic laparotomy.[9] Several case reports detail patients who have undergone pancreaticoduodenectomy to make the diagnosis. When the cystic lesion is erroneously diagnosed as pancreatic malignancy or pseudocyst, it often leads to unnecessary laparotomies.
| Conclusion | |  |
Pancreatic TB with an abscess is a rare clinical entity, yet to be considered in immunocompromised patients. Cystic pancreatic neoplasm being the main differential, imaging, and image-guided intervention helps in the diagnosis and along with appropriate anti-tubercular therapy obviates the need for surgery. Abdominal TB is an AIDS defining illness, and we hereby present a rare instance, where the pancreatic tubercular abscess is the initial manifestation of HIV/AIDS.
| References | |  |
| 1. | Nagar AM, Raut AA, Morani AC, Sanghvi DA, Desai CS, Thapar VB. Pancreatic tuberculosis: A clinical and imaging review of 32 cases. J Comput Assist Tomogr 2009;33:136-41.  |
| 2. | Khaniya S, Koirala R, Shakya VC, Adhikary S, Regmi R, Pandey SR, et al. Isolated pancreatic tuberculosis mimicking as carcinoma: A case report and review of the literature. Cases J 2010;3:18.  |
| 3. | Sonthalia N, Ray S, Pal P, Saha A, Talukdar A. Fine needle aspiration diagnosis of isolated pancreatic tuberculosis: A case report. World J Clin Cases 2013;1:181-6.  |
| 4. | Bhansali SK. Abdominal tuberculosis. Experiences with 300 cases. Am J Gastroenterol 1977;67:324-37.  [ PUBMED] |
| 5. | Liu Q, He Z, Bie P. Solitary pancreatic tuberculous abscess mimicking prancreatic cystadenocarcinoma: A case report. BMC Gastroenterol 2003;3:1.  |
| 6. | Xia F, Poon RT, Wang SG, Bie P, Huang XQ, Dong JH. Tuberculosis of pancreas and peripancreatic lymph nodes in immunocompetent patients: Experience from China. World J Gastroenterol 2003;9:1361-4.  |
| 7. | Lo SF, Ahchong AK, Tang CN, Yip AW. Pancreatic tuberculosis: Case reports and review of the literature. J R Coll Surg Edinb 1998;43:65-8.  |
| 8. | Asim S, Manjari L, Kenneth MS, Alexander CR, Christopher K, Khek-Yu H. Pancreatic tuberculous abscess diagnosed by endoscopic ultrasound-guided fine needle aspiration. J Pak Med Assoc 2010;60:499-501.  |
| 9. | Demir K, Kaymakoglu S, Besisik F, Durakoglu Z, Ozdil S, Kaplan Y, et al. Solitary pancreatic tuberculosis in immunocompetent patients mimicking pancreatic carcinoma. J Gastroenterol Hepatol 2001;16:1071-4.  |
[Figure 1], [Figure 2]
|