|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 3
| Issue : 2 | Page : 29-33 |
|
Risky sexual behavior and associated factors among married people receiving antiretroviral therapy in a tertiary hospital in Ondo State, Nigeria
Ayodeji M Adebayo1, Olayinka S Ilesanmi2, Faith O Alele2
1 Department of Communiy Medicine, College of Medicine, University of Ibadan, Ibadan, Nigeria
2 Department of Community Health, Federal Medical Centre, Owo, Ondo State, Nigeria
| Date of Web Publication | 14-Jul-2016 |
Correspondence Address:
Olayinka S Ilesanmi
Department of Community Health, Federal Medical Centre, Owo, Ondo
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157.186338

Background: Risky sexual behavior (RSB) increases the risk of human immunodeficiency virus (HIV) transmission. There are few documented studies on the pattern of RSB and associated factors among people living with HIV. This study aimed to determine the pattern and proportion of HIV-positive patients with RSB and and its associated factors at the Federal Medical Centre, Owo, Ondo State, Nigeria. Methods: A cross-sectional study of 314 sexually active persons receiving antiretroviral therapy treatment for at least 1 month was done using a semi-structured interviewer-administered questionnaire. Study-related data were obtained and analyzed using Statistical Package for the Social Science version 21.0. Bivariate analysis to find the association between age, sex, level of education, and occupation and RSB was explored with Chi-square test. Results: The mean age of respondents was 38.6 8.6 years while 43.6% were male. At least one RSB was reported in 42.4% (n = 314). RSBs such as nonconsistent condom use was reported by 25.2%, multiple sexual partners by 4.8%, not knowing partner's HIV status (16.1%), and nondisclosure of status to sexual partner (12.1%). Females (47.5%) were more likely to engage in RSB compared to males (35.8%), P = 0.038. Nonconsistent condom use was reported by 32.2% of females compared to 16.1% of males, P = 0.001. Not being sure of partner's status was responsible for RSB in 21.5% of females compared to 10.2% of males, P = 0.008. Having multiple sexual partners was more in male 10.9%, P < 0.001. Conclusion: RSB occurs more in females and the risk of transmitting HIV to serodiscordant partner exists. Counseling and targeted behavioral change intervention should be instituted to reduce RSB. Keywords: Condom, disclosure, multiple partners, sex behavior
How to cite this article:
Adebayo AM, Ilesanmi OS, Alele FO. Risky sexual behavior and associated factors among married people receiving antiretroviral therapy in a tertiary hospital in Ondo State, Nigeria. J HIV Hum Reprod 2015;3:29-33 |
How to cite this URL:
Adebayo AM, Ilesanmi OS, Alele FO. Risky sexual behavior and associated factors among married people receiving antiretroviral therapy in a tertiary hospital in Ondo State, Nigeria. J HIV Hum Reprod [serial online] 2015 [cited 2018 Aug 6];3:29-33. Available from: http://www.j-hhr.org/text.asp?2015/3/2/29/186338 |
| Introduction | |  |
Lifesaving antiretroviral therapy (ART) helps reduce the number of new human immunodeficiency virus (HIV) infections. From 1995 to 2012, ART averted 6.6 million acquired immune deficiency (AIDS)-related deaths worldwide, including 5.5 million deaths in low- and middle-income countries and improved the quality of life of people living with HIV/AIDS (PLWHA). [1] Sub-Saharan Africa has the most serious epidemic of HIV and AIDS with an estimated 24.7 million people living with HIV, a prevalence of 4.7%, and 1.1 million AIDS-related deaths in 2013. Research shows that almost 90% of people who tested positive for HIV in Sub-saharan Africa went on to access ART and 76% of people on ART have achieved viral suppression, whereby they are unlikely to transmit the virus to their sexual partners. [2]
According to the UNAIDS report, the current prevalence of HIV in Nigeria is 3.2% and approximately 210,000 people died from AIDS-related illnesses in 2013. [3] There has been no reduction in the number of annual deaths since 2005 which is possibly due to the extremely low provision of ART. Currently, only an estimated 21% of adults living with HIV are receiving treatment. [2] Factors associated with the HIV epidemic in Nigeria include multiple concurrent sexual partnerships, transactional and intergenerational sex, low personal risk perception, ineffective and inefficient services for sexually transmitted infections, and inadequate access to and poor quality of health-care services. Entrenched gender inequalities and inequities, chronic and debilitating poverty, and persistence of HIV/AIDS-related stigma and discrimination also significantly contribute to the spread of the infection. [4]
The global use of ART has been of clinical benefit, significantly reducing the viral load of HIV to undetectable levels. However, its efficacy and efficiency have led to the general belief that there is an increased likelihood of risky sexual behavior (RSB) among individuals living with HIV. The reduction in the viral load may cause these individuals to believe that they are no longer infectious. [5] Safe sex practices such as consistent and correct use of condom and limiting sexual intercourse to one uninfected partner are part of the preventive services that have become a priority in the global fight against HIV/AIDS and are recommended and encouraged among PLWHA. [6],[7]
Research has been conducted in industrialized and developed countries on the use of ART and RSB among PLWHA. [8],[9] This is not the case in sub-Saharan Africa where only a few documented studies on the use of ART and RSB among PLWHA have been conducted. [10] Knowledge of risky sexual practices of sexually active and married HIV clients on ART will help to decide better ways of curbing the spread of HIV. This study assessed risky sexual practices of sexually active and married HIV clients on ART at the Federal Medical Centre (FMC), Owo, Ondo State.
| Methods | |  |
Study area
This study was conducted at the ART Clinic of FMC, Owo, Ondo State. The hospital provides health-care services at the primary, secondary, and tertiary levels to patients who reside in the state and also to patients from other states who could have left their states as a result of stigma and discrimination. The HIV/AIDS program of the hospital provides services such as care and support and laboratory and clinical services. Since inception, an average of 20-25 new cases of HIV-positive patients is attended per week, and as in May 2014, the clinic had recruited about 3500 PLWHA, of whom about 2250 were on HAART apart from cases who were transferred out and those who died.
A cross-sectional design was used to study 314 sexually active PLWHA. Sample size was calculated using the formula for cross-sectional study (n = z 2 pq/d 2 ). The prevalence used for the calculation was 25% of noncondom use among PLWHA. [11] Only clients who had used ART for at least 1 month were interviewed. Data collection was over 3 months. A semi-structured interviewer-administered questionnaire was used to collect information from the clients. Medical officers from the Department of Community Health of the hospital were engaged as interviewers; they were trained in ethics of HIV/AIDS research and techniques of questionnaire administration.
Data were analyzed using Statistical Package for Social Scientist version 21.0 (IBM corporation, Armonk, USA). Descriptive statistics were done. Any client having at least one of the following: nonconsistent condom use, nondisclosure of status to sexual partner(s), not sure of sexual partner(s)' HIV status, and multiple sexual partners was categorized to have had RSB. Chi-square test was used to explore the association between sociodemographic characteristics of respondent and presence of RSB. The association between sex and occurrence and number of different RSBs was also tested using Chi-square test. The level of statistical significance was 5%.
Ethical clearance was obtained from the Health Research Ethics Committee of FMC, Owo. Informed consent was obtained from respondents after the objective of the study was explained to them. Each respondent was given information on the benefit of the study and that he/she could participate voluntarily and had the right to withdraw at any time without any negative effect.
| Results | |  |
[Table 1] describes the sociodemographic characteristics of the respondents. Of the 314 respondents, 43.6% were male whereas 56.4% were female. The mean age of respondents was 38.6 ± 8.6 years; 38 (12.1%) study respondents were <30 years, only 18 (5.7%) had no formal education. Students were 65 (20.7%), and others had some form of employment or occupation.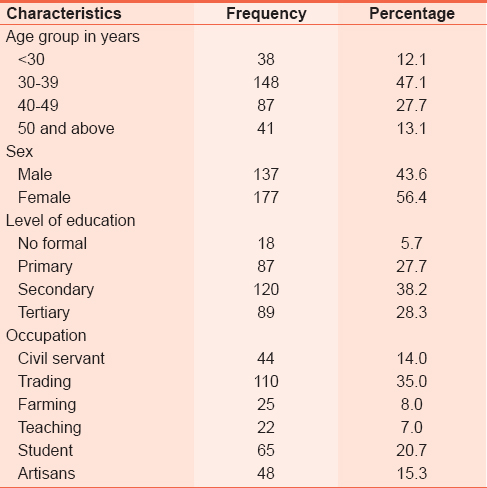 | Table 1: Sociodemographic characteristics of HIV positive married clients at the Federal Medical Centre, Owo
Click here to view |
The median duration on ART was 20 months, ranging 1-75 months.
[Figure 1] shows when respondents were first diagnosed to be HIV-positive. More than half, 204 (65%) respondents were diagnosed when they presented with illness. Only 39 (12.4%) were diagnosed during screening or outreach session.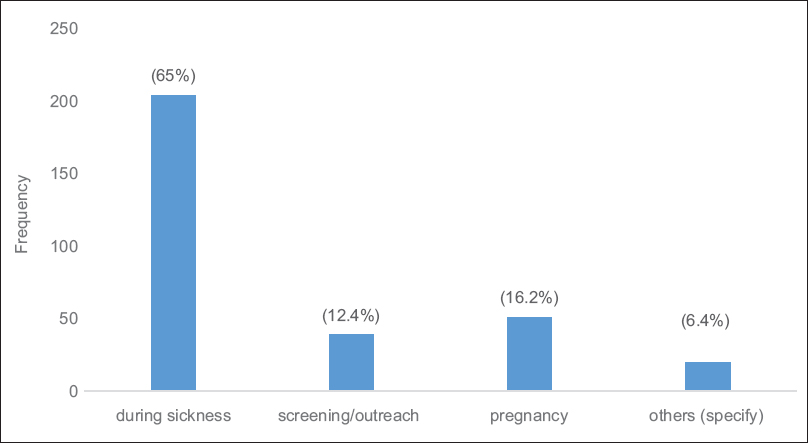 | Figure 1: When patients were diagnosed to be HIV positive virus-positive
Click here to view |
[Table 2] shows the association between sociodemographic characteristics and RSB. At least one RSB was found in 133 (42.4%). RSB was found in 84 (47.5%) females compared to 49 (35.8%) males, P = 0.038.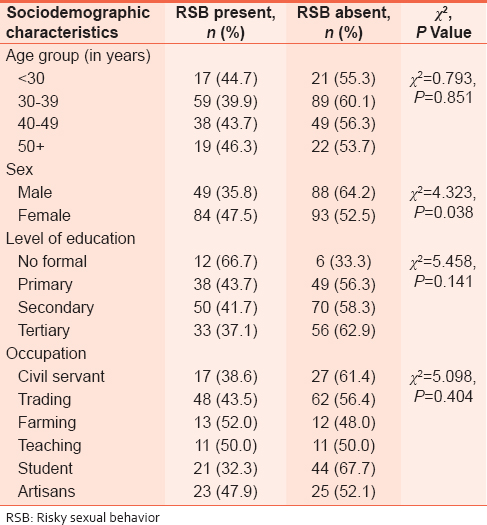 | Table 2: Sociodemographic characteristics and risky sexual behavior among HIV positive married clients at the Federal Medical Centre, Owo
Click here to view |
Inconsistent condom use was reported by 57 (32.3%) females compared to 22 (16.1%) males, P = 0.001. Not being sure of partner's status was responsible for RSB in 38 (21.5%) females compared to 14 (10.3%) males, P = 0.008. Having multiple sexual partners was more in males 15 (10.9%), P < 0.001. [Table 3] shows the association between RSB and sex of respondents.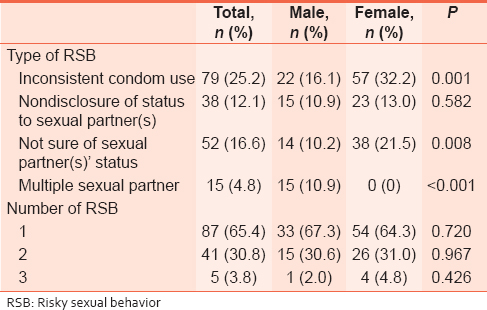 | Table 3: Association between risky sexual behavior and sex of HIV positive clients at the Federal Medical Centre, Owo
Click here to view |
| Discussion | |  |
In the study population, RSB was more common among the female respondents. This finding can be attributed to the dominant patriarchal culture and society in Africa which exacerbates women's inferiority and their disparate health status. Women often play no part in sexual decision-making, and there may be violent consequences if a woman was to take initiative in sex, suggest condom use, or refuse sexual advances. [12] Limited voice, subservience, violence, and economic powerlessness, all barriers to HIV prevention make women's existence difficult and oppressive according to a study conducted in Zimbabwe. [13]
Many structural vulnerabilities such as gender inequality and gender-based violence, [14] migration and health-seeking-related stigma, [15] and place women at risk of contracting HIV. Culturally acceptable roles and conducts for men and women such as the low social value and power of women and ideas of manhood linked to the control of women result in lower levels of education among women; few public roles for women; lack of family, social and legal support for women; and the lack of economic power. [16] Institutionalized economic inequalities keep money, land, and other resources out of women's reach, causing women to be financially dependent on men, more likely to practice transactional sex, less likely to be able to negotiate safe sex or condom use with a partner, and more at risk of violence. [17],[18],[19],[20] Female respondents reported to lower condom use in this study; other studies conducted among patients on ART in Kenya showed that inconsistent use of condoms was significantly likely to occur among women than men. [21]
One of the factors affecting RSB among female respondents was lack of awareness of the HIV status of their partners. This was reported in some other studies conducted among people living with HIV on HAART in Uganda, Kenya, and South Africa. [22],[23],[24] Other factors that have been attributed to sexual risk behavior include lack of control over sexual decisions, desire and pressure to bear children, partner's objection, and inconvenience. [25],[26]
A key risk factor for HIV transmission is multiple sexual partners; in this study, the male gender was significantly more likely to have more than one sexual partner compared to the female gender. In some other studies, male gender was a predictor and important determinant of multiple sexual partners; this is possible because some or most societies allow the male gender to have as many sexual partners as possible, either as wives or as concubines. [18],[25]
| Conclusion | |  |
This study showed that sexual risk behavior was common among PLWHA. We found that the use of condom was not consistent among the females while the male respondents were more likely to have multiple sexual partners. The risk of transmitting HIV to serodiscordant partner exists. Adequate interventions to insure safe sex practice among clients already on ART and those who are about to initiate ART are important. This will reduce the risk of transmitting HIV to serodiscordant partner.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | |
| 2. | |
| 3. | UNAIDS. Epidemiology Fact Sheets of HIV and AIDS in Nigeria; 2014. Available from: . [Last accessed on 2015 Oct 26].  |
| 4. | Nigeria National Agency for the Control of AIDS. Country Progress Report; 2014. Available from: . [Last accessed on 2016 Feb 26].  |
| 5. | Shafer LA, Nsubuga RN, White R, Mayanja BN, Chapman R, O′brien K, et al. Antiretroviral therapy and sexual behavior in Uganda: A cohort study. AIDS 2011;25:671-8.  |
| 6. | World Health Organization. Global Update on the Health Sector Response to HIV, WHO/HIV/2014.15. Geneva;Switzerland: World Health Organization; 2014. Avaliable from: . [Last accessed on 2015 Oct 15].  |
| 7. | UNFPA. UNFPA′s Definition of Condom Programming in HIV Prevention Now, Programme Brief No. 6. Condom Programming for HIV Prevention; 2002. Available from: . [Last accessed on 2014 Nov 25].  |
| 8. | Crepaz N, Hart TA, Marks G. Highly active antiretroviral therapy and sexual risk behavior: A meta-analytic review. JAMA 2004;292:224-36.  |
| 9. | Martin Hilber A, Hull TH, Preston-Whyte E, Bagnol B, Smit J, Wacharasin C, et al. A cross cultural study of vaginal practices and sexuality: Implications for sexual health. Soc Sci Med 2010;70:392-400.  |
| 10. | Olise P. Control of endemic diseases. In: Primary Health Care for Sustainable Development. Abuja: Ozege Publications; 2007. p. 263-5.  |
| 11. | Adebayo AM, Ilesanmi OS, Omotoso BA, Ayodeji OO, Kareem AO, Alele FO. Disclosure to sexual partner and condom use among HIV positive clients attending ART clinic at a tertiary health facility in South West Nigeria. Pan Afr Med J 2014;18:245.  |
| 12. | Duffy L. Culture and context of HIV prevention in rural Zimbabwe: The influence of gender inequality. J Transcult Nurs 2005;16:23-31.  |
| 13. | Buvé A, Bishikwabo-Nsarhaza K, Mutangadura G. The spread and effect of HIV-1 infection in sub-Saharan Africa. Lancet 2002;359:2011-7.  |
| 14. | Murphy EM, Greene ME, Mihailovic A, Olupot-Olupot P. Was the "ABC" approach (abstinence, being faithful, using condoms) responsible for Uganda′s decline in HIV? PLoS Med 2006;3:e379.  |
| 15. | Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet 2008;372:764-75.  |
| 16. | Gupta GR. How men′s power over women fuels the HIV epidemic: It limits women′s ability to control sexual interactions. Br Med J 2002;324:183.  |
| 17. | |
| 18. | Pettifor AE, Measham DM, Rees HV, Padian NS. Sexual power and HIV risk, South Africa. Emerg Infect Dis 2004;10:1996-2004.  |
| 19. | Leclerc-Madlala S. Age-disparate and intergenerational sex in Southern Africa: The dynamics of hypervulnerability. AIDS 2008;22 Suppl 4:S17-25.  |
| 20. | Ackermann L, Klerk GW. Social factors that make South African women vulnerable to HIV infection. Health Care Women Int 2002;23:163-72.  |
| 21. | Ragnarsson A, Ekström AM, Carter J, Ilako F, Lukhwaro A, Marrone G, et al. Sexual risk taking among patients on antiretroviral therapy in an urban informal settlement in Kenya: A cross-sectional survey. J Int AIDS Soc 2011;14:20.  |
| 22. | Osinde MO, Kaye DK, Kakaire O. Sexual behaviour and HIV sero-discordance among HIV patients receiving HAART in rural Uganda. J Obstet Gynaecol 2011;31:436-40.  |
| 23. | Sarna A, Luchters SM, Geibel S, Kaai S, Munyao P, Shikely KS, et al. Sexual risk behaviour and HAART: A comparative study of HIV-infected persons on HAART and on preventive therapy in Kenya. Int J STD AIDS 2008;19:85-9.  |
| 24. | Mlambo M, Peltzer K. HIV sero-status disclosure and sexual behaviour among HIV positive patients who are on antiretroviral treatment (ART) in Mpumalanga, South Africa. J Hum Ecol 2011;35:29-41.  |
| 25. | Myer L, Morroni C, Rebe K. Prevalence and determinants of fertility intentions of HIV-infected women and men receiving antiretroviral therapy in South Africa. AIDS Patient Care STDS 2007;21:278-85.  |
| 26. | Stevens PE, Galvao L. He won′t use condoms: HIV-infected women′s struggles in primary relationships with serodiscordant partners. Am J Public Health 2007;97:1015-22.  |
[Figure 1]
[Table 1], [Table 2], [Table 3]
|