|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 9
| Issue : 3 | Page : 102-107 |
|
Determinants of noninstitutional deliveries in an urban community in Nigeria
I Nduka1, EC Nduka2
1 Department of Community Medicine, Abia State University Teaching Hospital, Aba, Nigeria
2 Department of Obstetrics and Gynaecology, Federal Medical Center, Umuahia, Abia State, Nigeria
| Date of Web Publication | 15-Nov-2014 |
Correspondence Address:
I Nduka
Department of Community Medicine, Abia State University Teaching Hospital, Aba, Abia State
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/9783-1230.144770

Background: Maternal mortality in developing countries is an issue of global concern. Delivery attended to by skilled birth attendants is emphasized as an important strategy for reducing maternal deaths. Choice of birth place is determined by various factors. This study thus evaluates determinants of noninstitutional birth places and reasons for the choice among women in Aba, South-East, Nigeria. Materials and Methods: The study was descriptive cross-sectional in design carried out among 420 women in Aba, a commercial city in Abia state, Nigeria. Cluster and simple random sampling techniques were used to select the study participants. Data was collected using interviewer administered questionnaire and analysed by SPSS version 17 software. Logistic regression analysis was done to determine predictors of noninstitutional birth places and the result presented in tables. Result: One hundred and sixty-four respondents (39%) had their last deliveries in a nonhealth facility with unskilled attendants. These places included maternity homes (10.2%), traditional birth attendants (11.9%), religious home (7.4%) and home deliveries (9.5%). There was statistical significant difference between age, marital status, level of education, number of living children and noninstitutional birth places. Reasons cited for choice of nonhealth birth places included cost, friendly staff and perceived experience of birth attendant. Conclusion / Recommendation: Noninstitutional birth places are still prevalent in urban communities and women prefer these birth places for diverse reasons. This study recommends an address of reasons for the choice of birth places among women.Background: Maternal mortality in developing countries is an issue of global concern. Delivery attended to by skilled birth attendants is emphasized as an important strategy for reducing maternal deaths. Choice of birth place is determined by various factors. This study thus evaluates determinants of noninstitutional birth places and reasons for the choice among women in Aba, South-East, Nigeria. Materials and Methods: The study was descriptive cross-sectional in design carried out among 420 women in Aba, a commercial city in Abia state, Nigeria. Cluster and simple random sampling techniques were used to select the study participants. Data was collected using interviewer administered questionnaire and analysed by SPSS version 17 software. Logistic regression analysis was done to determine predictors of noninstitutional birth places and the result presented in tables. Result: One hundred and sixty-four respondents (39%) had their last deliveries in a nonhealth facility with unskilled attendants. These places included maternity homes (10.2%), traditional birth attendants (11.9%), religious home (7.4%) and home deliveries (9.5%). There was statistical significant difference between age, marital status, level of education, number of living children and noninstitutional birth places. Reasons cited for choice of nonhealth birth places included cost, friendly staff and perceived experience of birth attendant. Conclusion / Recommendation: Noninstitutional birth places are still prevalent in urban communities and women prefer these birth places for diverse reasons. This study recommends an address of reasons for the choice of birth places among women. Keywords: Nigeria, Noninstitutional birth places, Reasons, Urban community
How to cite this article:
Nduka I, Nduka E C. Determinants of noninstitutional deliveries in an urban community in Nigeria. J Med Investig Pract 2014;9:102-7 |
How to cite this URL:
Nduka I, Nduka E C. Determinants of noninstitutional deliveries in an urban community in Nigeria. J Med Investig Pract [serial online] 2014 [cited 2018 Aug 24];9:102-7. Available from: http://www.jomip.org/text.asp?2014/9/3/102/144770 |
| Introduction | |  |
Improving maternal health has been an issue of global concern. The fifth millennium development goal (MDG) addresses the reduction of maternal mortality ratio (number of maternal deaths per 100,000 live births) by 75% between 1990 and 2015. [1] In 2013, 289,000 maternal deaths occurred worldwide, most of which were in low-income and middle-income countries and were preventable. [2] Maternal deaths have however dropped by 45% since 1990 showing some progress towards the target, [3] but further improvements are needed to achieve the MDG required annual 5.5% decline in maternal mortality ratio. Risk of maternal mortality is highest for adolescent girls under 15 years [3] especially in developing countries where limited resources are available for adolescent reproductive health services. A woman's life-time risk of maternal death - the probability that a 15-year-old woman will eventually die from a maternal cause - is 1 in 3700 in developed countries when compared with 1 in 160 in developing countries. [3] Worldwide, 80% of maternal deaths arise from complications of severe bleeding, infections, hypertensive disorders and unsafe abortion in that order. [4] Other causes such as malaria and AIDS during pregnancies have been reported. [4]
Knowledge of the causes of maternal deaths is important in maternal mortality reduction. [5],[6] One of the key indicators in achieving MDG 5 is the proportion of women who had their deliveries with skilled birth attendants; [7] countries where more than 80% of women are taken care of by skilled birth attendants in pregnancy and delivery have low maternal mortality ratio. [8] Monitoring of pregnancy and delivery by trained health professionals is crucial in maternal mortality reduction. Antenatal care, for instance, provides an opportunity for mothers to acquire knowledge regarding pregnancy, child birth and post child birth period including family planning choices. During antenatal visits, pre-eclampsia is detected early and managed before the onset of eclampsia and other life-threatening complications. Skilled care during child birth can abort deaths from bleeding as well as prevent infections to mother and child thereby preserving two lives; mother and new born. [9],[10] Almost 3 million newborn babies die every year and an additional 2.6 million delivered as still birth. [11],[12]
Developing countries are faced with limited resources and, as a result, investment in health care delivery is little amidst other competing projects. [13],[14] Over 99% of maternal deaths occur in developing countries. [2] The maternal mortality ratio in 2013 was 230/100,000 live births as against 16/100,000 live births in developed countries. [2] In developing countries, a high proportion of women still deliver at home [15],[16],[17] with only 46% deliveries attended to by skilled attendants. [2] Various factors such a maternal age, parents education, residential area (urban/rural), available health facility, distance to health facility and perceived experiences of health professionals by mothers determine choice of place of delivery among women. [13] Many health professionals are ill-equipped in delivering reproductive services to young women, and this have been shown to contribute to reasons why women prefer noninstitutional birth places. [18] In most African countries, decisions to access maternity services are taken by mother-in-laws especially for women who have little or no education and are financially incapable. This is also possible in marriages where the women are still very young to take decisions regarding health and access to health care. [19]
Nigeria is one of the highest contributors of high maternal mortality in developing countries with an MMR of 560/100,000 in 2013. [20] There has been some reduction in the figure from 1990 to 2013 (1200-560/100,000 live births) which can be attributed to increasing government efforts to make maternal care available to women of reproduction age group with particular reference to the recent mid wives service scheme. Low use of maternal health services [MHS] has been reported as a major contributory factor to high maternal mortality in Nigeria. [16],[21],[22],[23] According to the National demographic and health survey of 2013, about three-fifth of mothers (61%) who participated in the 5 year study period attended antenatal care in a health facility by a skilled health provider - a doctor, nurse, midwife or a certified auxiliary midwife among whom were women aged 20-34 years. This data was higher in urban areas (86%) than rural areas (47%). The survey also showed that 67% of women in urban areas and 23% of women in rural communities had deliveries taken by a skilled health provider. This data varies among geopolitical zones; the South-East and South-West geopolitical zones reported a higher percentage of deliveries attended by skilled health providers (82% and 83% respectively) than the North-West and North-East (12% and 20% respectively). [24]
Decision to deliver with a skilled provider is dependent on a lot of factors and the understanding of which is vital to utilization of MHS. More studies have been carried out in rural communities than urban regarding birth place preferences of women. This study was, therefore, conducted to add to existing literature on the determinants of noninstitutional birthplaces among mothers in an urban community in Nigeria.
| Materials and methods | |  |
This was a descriptive cross sectional study conducted in Aba, Abia State in January, 2014. Aba is a major commercial town in South-East, Nigeria with trading as the main occupation. Aba is an Ibo speaking town though due to its commercial activities, other tribes reside in it.
The health facilities in the area include a tertiary health facility - Abia State University Teaching Hospital, which is owned by the Government, Primary Health Care Centres distributed in all the Local Government areas and privates hospitals. The primary health centres deliver health services including maternal and child health care with referrals to the tertiary hospital.
The study population comprised women who have had at least one pregnancy carried to term in the last 2 years. Interviewer-administered questionnaire was used to collect data from the participants. This was pre-tested in another community and adjusted thereafter. Information on sociodemographic, antenatal care attendant in the last pregnancy, place of delivery and reasons for the choice were obtained from the respondents. Women who delivered in private hospitals were excluded from the study. Women who lived within 2 km from any health facility owned by the government were included in the study.
Sample size determination was calculated using the formula n = Z 2 Pq/d 2 , where z is 1.96 at 95% confidence interval, prevalence of 47% was used based on previous studies of birth places in developing countries [14] and d, the tolerable standard error margin of 0.05. Calculated minimum sample size of 382 was obtained and adjusted to 420 using 10% nonresponse rate. Cluster sampling and simple random sampling techniques were used to select the study participants. With cluster sampling, the roads and streets were selected, while simple random sampling by balloting was used in choosing the women from each compound in cases with many eligible women living within the premises. Ethical approval was obtained from the Abia State University Research and Ethics committee and verbal consent from the respondents.
Data was analysed using SPSS version 17 (Chicago). Result was presented in tables. Chi-square was used to evaluate categorical variables and 0.05 accepted as statistically significant. Logistic regression was used to determine predictors of noninstitutional birth place choices of respondents.
| Results | |  |
A total of 420 women participated in the study. The age range was 15-59 years. Those 30-34 years were the highest in the study population 124 (29.5%) while women < 20 years of age were the fewest 39 (9.3%). Twenty-one of the respondents (5%) were single while a greater proportion, 345 (82.1%) married. Most had secondary education, 156 (37.1%), semi-skilled professions, 219 (52.1%) while 201 (47.9%) of their spouses were unskilled workers. Two hundred and one (47.9%) had three living children while 26 (6.2%) had none [Table 1]. One hundred and sixty-four women (39%) did not deliver with skilled birth attendants; 43 (10.2%) where in maternity homes, 50 (11.9%) with traditional birth attendants, 31 (7.4%) in religious places and 40 (9.5%) at home [Table 2]. [Table 2] also shows that 328 (78.1%) attended antenatal care at the primary health care centres while 269 (64.0%) attended antenatal at the tertiary health facility. There was statistical significant difference between noninstitutional birth place choices and age (χ2 = 21.2; P = 0.000), marital status (χ2 = 17.5; P = 0.000), level of education (χ2 = 74.5; P = 0.000), working category of both the woman and her spouse (P = 0.000) and number of living children (χ2 = 25.8; P = 0.000) [Table 3].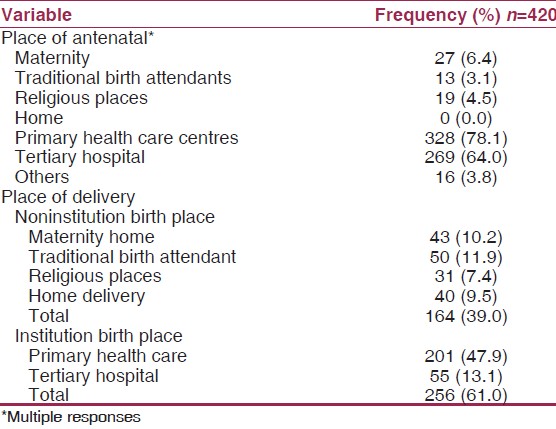 | Table 2: Distribution of respondents by place of antenatal care and delivery
Click here to view |
Mothers in age range 20-23-year-old were 5 times more likely to deliver in noninstitutional birth places than those 35-39 years of age (OR = 5.384, 95%CI: 2.201-13.158). Widows were 3 times more likely to deliver at noninstitutional birth places than the married women (OR = 3.226, 95% CI: 1.784-5.829). Women with no formal education were 6 times more likely to deliver in non health facilities than those with secondary education (OR = 6.284, 95% CI: 3.658-10.794). Regarding work categories, unskilled women were 23 times more likely to deliver in noninstitutional birth places than the highly skilled women (OR = 23.083, 95% CI: 10.623-50.149). Women with one living child were 1.9 times more likely to deliver with unskilled birth attendants than women with four living children [Table 4].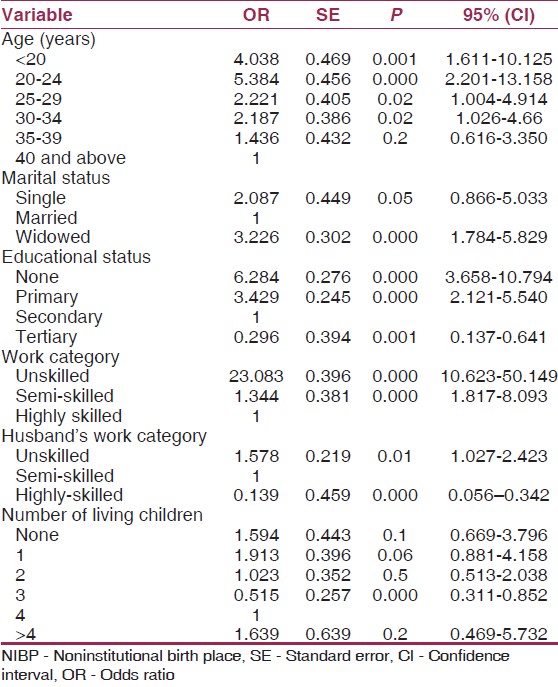 | Table 4: Multivariate regression analysis of NIBP preference
among respondents
Click here to view |
Reasons for choice of noninstitutional birth places included cost 125 (76.2%), staff availability 107 (65.2%), and friendly attendant 164 (100.0%) [Table 5].
| Discussion | |  |
The aim of this study was to evaluate the noninstitutional birth places in an urban community and reasons for the choice. Urban residential areas, usually, have more infrastructures in health care facilities than rural areas, and thus, usage of MHS is expected to be high. The findings from this study adds to existing literature in two facets; one the study area is an urban community with fairly equipped health facilities that deliver maternal services and good referral system to the tertiary hospital thus eliminating an unequipped health facility as a factor for non usage of MHS. Secondly, women who lived within 2 km of any health facility were included in the study so as to exclude distance that has been reported in previous studies as a known barrier for the utilization of MHS. [14],[15] This inclusion criterion enabled the researchers to determine other reasons other than distance as a limiting factor in institutional birth place choices.
Variations in socio-demographic characteristics have been reported to affect decisions on choice of birth places among women. [5],[15] Extreme age groups (young and older women) have a higher risk for birth complications [2],[25] and thus the need to have their deliveries attended to by skilled birth attendants; this does not however exclude women in other age groups. In this study, 9.3% of the respondents were less than 20 years and 11.7% were 40 years and above. One hundred and sixty-four (39%) respondents in this study utilized noninstitutional birth places in their last delivery, with traditional birth attendants (11.9%) being the highest patronised. This is similar to the 2013 National Demographic Health survey. [24] Choice of birth places in Nigeria varies among the geo-political zones and related to factors such as accessibility, culture, education and differences in maternal mortality within these zones. [24],[26],[27] A study conducted in South-West Nigeria, showed a high use of maternity services with only 20% of the respondents delivering with traditional birth attendants [28] while another study in Northern Nigeria reported a much lower use of maternal services. [22]
Most women in this study received antenatal care in health facilities; 78.1% in Primary health care facilities and 64% in the tertiary hospital. This finding is interesting considering the high proportion of women who had antenatal visits in health facilities as against a lower proportion (61%) who eventually gave birth in these health facilities. The women also reported registering for antenatal care in more than one health facility, although the reasons were not obtained in this study. Some women who registered in a health facility also registered in non health facility showing a prior preference for noninstitutional delivery. Further studies should be conducted to determine the reasons why women registered for antenatal care with unskilled attendants. Antenatal care is a key entry point for an uneventful pregnancy, child birth and post natal period. [5] Experiences of women during antenatal care can influence their decisions to deliver in health facilities. [29],[30] Antenatal care also provides an opportunity for early diagnosis and prompt intervention of diseases and complications. [31]
In this study, age, marital status, education, work category, number of living children and husband's work category were all statistically significant with use of noninstitutional birth place choices. Younger women from this study utilized noninstitution birth facility which differs from some other studies [5],[14],[18] but similar to a report in a Malawian study. [32] The reason for this observation can be explained by lower level of education, unskilled and semi-skilled work category of the respondents. These young women might also have been victims of early marriage when they had not completed their education nor adequately learnt any skill. Education is a proven factor affecting utilization of maternal services. [33],[34],[35] This study revealed that women with no formal education utilize noninstitutional birth places more than those with secondary or tertiary education. Educated women are, usually, better informed on the importance of skilled birth attendants in maternal health and are thus better equipped in decision taking regarding their health. Women who were single or widowed from this study were more likely to have deliveries with unskilled birth attendants than the married women. This is consistent with studies conducted elsewhere. [16],[17],[22],[25] Such women have autonomy in taking decisions regarding birth places since there was no spouse to influence the decisions. It also shows the role of the male partner in decisions regarding utilizations of MHS.
Parity was an important factor that affected birth place preferences from this study; women with more than four children (higher parity) delivered in noninstitutional birth places. This is similar to previous studies. [32],[33] Multiparous women are, usually, better experienced and have developed some level of confidence in child birth especially if they have not had birth complications in previous deliveries. Lower parity (0-1 living child) from the result of this study was also seen to be associated with a high preference for noninstitutional birth places. This however differs from previous studies, [32],[33] and may be related to lower educational status and unskilled status of the women who were ill-equipped before marriage. Socio-economic status of the family has been reported as a predictor to choice of health care. [34],[35] This study showed that women whose husbands were unskilled or semi-skilled utilized noninstitutional birth places than those with highly skilled spouses.
Reasons such as cost, husband's preference, mother-in-law's preference and perceived experience of staff were given for the choice of birth place among the mothers. This is similar to studies conducted elsewhere. [34],[35]
This study has some implications for policies and programs aimed at reducing maternal mortality in Nigeria. There is need to promote girl-child education. Secondly, health care professional should undergo continuous medical training in maternal care. Thirdly, there is need for adequately equipping health facilities with materials and medical personnel. Involvement of men in reproductive health services is important; services friendly to males should be encouraged in all health facilities that deliver maternal health care.
Further studies are recommended to evaluate reasons for choice of more than one health facility for antenatal care as well as reasons for choice of both non health (noninstitutional) facility and health (institutional) facility for antenatal care. Studies are recommended to evaluate women's perspectives of causes of maternal mortality as this might be of help in evaluating attitudes of women towards unskilled birth attendants.
This study is limited in the use of questionnaires for data collection that might have led to missing some important findings as a result of non-in depth questions. Temporality in the relationship between independent variables and the outcome is difficult to ascertain in a cross-sectional study like this one. However, in spite of these limitations, the findings from this study gave some insight into the various determinants of noninstitutional birthplace choices among respondents.
| Conclusion | |  |
Noninstitutional birth places are still prevalent in urban communities from the result of this study and women still prefer unskilled attendants to take their deliveries for various reasons.
| References | |  |
| 1. | United Nations. 2000. United Nations Millennium Declaration. Fifty-fifth session of the United Nations General Assembly. New York: United Nations; 18 September, 2000. (General Assembly document, No. A/RES/55/2).  |
| 2. | WHO. World Health Statistics 2014. Geneva: World Health Organisation; 2014. Available from: http://www.who.int/mediacentre/factsheet. [Last accessed on 2014 Jun 01].  |
| 3. | WHO. Maternal Mortality 2014. Geneva: World Health Organisation; 2014. Available from: http://www.who.int/mediacentre/factsheet. [Last accessed on 2014 Jun 01].  |
| 4. | Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health 2014;2:e323-33.  |
| 5. | Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, et al. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: Implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth 2007;7:29.  |
| 6. | UNICEF. Eastern and Southern Africa Regional Office: Maternal Mortality Reduction Strategy; 2003.  |
| 7. | United Nations. Millennium Development Goals Report. New York: United Nations; 2008.  |
| 8. | WHO. Maternal Mortality in 2005. Geneva: WHO, UNICEF and UNFPA; 2007.  |
| 9. | Koblinsky M, Matthews Z, Hussein J, Mavalankar D, Mridha MK, Anwar I, et al. Going to scale with professional skilled care. Lancet 2006;368:1377-86.  |
| 10. | Adegoke AA, van den Broek N. Skilled birth attendance-lessons learnt. BJOG 2009;116 Suppl 1:33-40.  |
| 11. | UNICEF, WHO. The World Bank, United Nations Population Division. The Inter-Agency Group for Child Mortality Estimation (UN IGME). Levels and Trends in Child Mortality. Report 2013. New York, USA: UNICEF; 2013.  |
| 12. | Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, et al. Stillbirths: Where? When? Why? How to make the data count? Lancet 2011;377:1448-63.  |
| 13. | Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: Examining the scale of the problem and the importance of context. Bull World Health Organ 2007;85:812-9.  |
| 14. | Montagu D, Yamey G, Visconti A, Harding A, Yoong J. Where do poor women in developing countries give birth? A multi-country analysis of demographic and health survey data. PLoS One 2011;6:e17155.  |
| 15. | Mrisho M, Schellenberg JA, Mushi AK, Obrist B, Mshinda H, Tanner M, et al. Factors affecting home delivery in rural Tanzania. Trop Med Int Health 2007;12:862-72.  |
| 16. | Osubor KM, Fatusi AO, Chiwuzie JC. Maternal health-seeking behavior and associated factors in a rural Nigerian community. Matern Child Health J 2006;10:159-69.  |
| 17. | Sobel HL, Oliveros YE, Nyunt US. Secondary analysis of a national health survey on factors influencing women in the Philippines to deliver at home and unattended by a healthcare professional. Int J Gynaecol Obstet 2010;111:157-60.  |
| 18. | Creel L, Perry RJ. Improving the Quality of Reproductive Health Care for Young People. Chicago: New Perspectives on Quality of Care; 2003. p. 4.  |
| 19. | World Health Organization, United Nations Population Fund. Married Adolescents: No Place of Safety. Geneva, Switzerland: World Health Organization, United Nations Population Fund; 2006.  |
| 20. | WHO, UNICEF, UNFPA, World Bank, United Nations Population Division. The Inter-Agency Group for Maternal Mortality Estimation. Maternal Moratlity in Nigeria 1990-2013. Report. New York, USA: UN Secretariat; 2013.  |
| 21. | Igberase GO, Isah EC, Igbekoyi OF. Awareness and perception of maternal mortality among women in a semi-urban community in the Niger Delta of Nigeria. Ann Afr Med 2009;8:261-5.  [ PUBMED]  |
| 22. | Kabir M, Iliyasu Z, Abubakar IS, Asani A. Determinants of utilization of antenatal care services in Kumbotso Village, northern Nigeria. Trop Doct 2005;35:110-1.  |
| 23. | Bawa SB, Umar US, Onadeko M. Utilization of obstetric care services in a rural community in southwestern Nigeria. Afr J Med Med Sci 2004;33:239-44.  |
| 24. | National Population Commission. Nigeria Demographic and Health Survey. Calverton, Maryland, USA: MEASURE DHS ICF International; 2013.  |
| 25. | Mekonnen Y, Mekonnen A. Factors influencing the use of maternal healthcare services in Ethiopia. J Health Popul Nutr 2003;21:374-82.  |
| 26. | Idris SH, Sambo MN, Ibrahim MS. Barriers to utilisation of maternal health services in a semi-urban community in northern Nigeria: The clients' perspective. Niger Med J 2013;54:27-32.  [ PUBMED]  |
| 27. | Awoyemi TT, Obayelu OA, Opaluwa HI. Effect of distance on utilization of health care services in rural Kogi State, Nigeria. J Hum Ecol 2011;35:1-9.  |
| 28. | Iyaniwura CA, Yussuf Q. Utilization of antenatal care and delivery services in Sagamu, south western Nigeria. Afr J Reprod Health 2009;13:111-22.  |
| 29. | Onah HE, Ikeako LC, Iloabachie GC. Factors associated with the use of maternity services in Enugu, southeastern Nigeria. Soc Sci Med 2006;63:1870-78.  |
| 30. | van Eijk AM, Bles HM, Odhiambo F, Ayisi JG, Blokland IE, Rosen DH, et al. Use of antenatal services and delivery care among women in rural western Kenya: A community based survey. Reprod Health 2006;3:2.  |
| 31. | Maternal and Child Health Division: Focused Antenatal Care: Providing Integrated, Individualized Care During Pregnancy. Office of Health Infectious Diseases and Nutrition, Bureau for Global Health U.S Agency for International Development; 2007.  |
| 32. | Palamuleni M. Determinants of non-institutional deliveries in Malawi. Malawi Med J 2011;23:104-8.  [ PUBMED] |
| 33. | Yar'Zever IS, Said IY. Knowledge and barriers in utilization of maternal health care services in Kano State, Northern Nigeria. Eur J Biol Med Sci Res 2013;191:1-14.  |
| 34. | Ezechi OC, Fasubaa OB, Obiesie LO, Kalu BK, Loto OM, Dubub VI, et al. Delivery outside hospital after antenatal care: Prevalence and its predictors. J Obstet Gynaecol 2004;24:745-9.  |
| 35. | Yanagisawa S, Oum S, Wakai S. Determinants of skilled birth attendance in rural Cambodia. Trop Med Int Health 2006;11:238-51.  |
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
|