|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 9
| Issue : 3 | Page : 126-129 |
|
Prevalence of adenocarcinoma among cervical cancer patients in Igbos of Nigeria
KO Ngwogu1, AC Ngwogu2, GIN Ndubuka3
1 Department of Chemical Pathology, Faculty of Clinical Medicine, College of Medicine and Health Sciences, Abia State University, Uturu, Abia State, Nigeria
2 Department of Medical Microbiology, Faculty of Clinical Medicine, College of Medicine and Health Sciences, Abia State University, Uturu, Abia State, Nigeria
3 Department of Biomedical Technology, Federal University of Technology, Owerri, Ihiagwa, Nigeria
| Date of Web Publication | 15-Nov-2014 |
Correspondence Address:
K O Ngwogu
Faculty of Clinical Medicine, College of Medicine and Health Sciences, Abia State University, Uturu, Abia State
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/9783-1230.144775

Background: Adenocarcinoma of the cervix, although a common problem among females in Nigeria is often poorly screened and consequently under-detected. There is a need for improved awareness and early screening to stem the trend of increasing mortality. Objective: To determine the prevalence of adenocarcinoma among cervical cancer patients in Igbos of Nigeria. Design: Data sources from surgical specimens from 40 hospitals spread across the five states of South Eastern Nigeria. Setting: National Orthopedic Hospital, Enugu, in South Eastern Nigeria. Materials and Methods: A total of 206 cervical histopathology reports obtained from patients of the Igbo ethnic group of Nigeria between January 2007 and December 2010 were selected and studied. Results: Prevalence of adenocarcinoma is 11.5% with a mean age of presentation at 62 ± 6.4 years. It is associated with irregular vaginal bleeding (60%), vaginal discharge (15%), lower abdominal pains (13%), and post-coital bleeding (12%). Age and parity of the patients appeared to be significantly associated with the prevalence of the disease. Conclusion: There is a need for increased awareness and periodic screening to ensure early detection and institution of therapy. Keywords: Adenocarcinoma, Cervical Cancer, Igbos, Nigeria
How to cite this article:
Ngwogu K O, Ngwogu A C, Ndubuka G. Prevalence of adenocarcinoma among cervical cancer patients in Igbos of Nigeria. J Med Investig Pract 2014;9:126-9 |
How to cite this URL:
Ngwogu K O, Ngwogu A C, Ndubuka G. Prevalence of adenocarcinoma among cervical cancer patients in Igbos of Nigeria. J Med Investig Pract [serial online] 2014 [cited 2018 Aug 24];9:126-9. Available from: http://www.jomip.org/text.asp?2014/9/3/126/144775 |
| Introduction | |  |
Cervical cancer is an important public health problem. It is the second leading cause of cancer death among women world-wide, resulting in 275,000 deaths annually. [1] It is also the most common gynecological malignant neoplasm all over the world. [2] According to recent data, an estimated 500,000 new cases occur annually worldwide, with the vast majority in the developing countries. [3] Over 80% of the estimated deaths which occur annually due to cervical cancer also occur in these countries. In Nigeria, the age-adjusted incidence rate of cervical cancer is approximately 24.1/100,000 from Ibadan Cancer Registry data (1998-1999). This is probably an under estimation as there is general under reporting of cancer cases. In general, women of low socio-economic status have higher rates. [2]
Cervical cancer is a potentially preventable disease. While screening programs have decreased the incidence of squamous cell cervical cancer, the incidence of adenocarcinoma of the cervix has risen from 5% to 24%. [3],[4] It is, therefore, important to be aware of the risk factors, screening techniques and available diagnostic options with special attention to the management of the pre-invasion disease. [2] The risk factors of cervical cancer include women with multiple sex partners, early age of first intercourse, history of venereal disease, [5] women whose male partners have multiple partners, [6] association with Human papilloma virus, [7] (a sexually transmitted virus, especially of the type 16, 18, 31,33), smoking [8],[9] and early marriage. [10]
Cervical cancer is associated with a broad age range. [11] In contrast, cervical intraepithelial neoplasm, which are the precursors of invasive disease frequently occur in younger women, often under 35 years of age. The observation that the precursor lesions occur at a younger age than does invasive disease is consistent with the notion that the malignant transformation of squamous epithelial cells requires a longer latency period. Significant declines in the incidence and mortality of cervical cancer have been noted in the last 20 years, particularly in advanced countries of the world where screening programs are better organized. Accessibility to treatment, early detection, reduction in parity, sexual behavioral change and awareness have contributed to its decline. Unfortunately, there has been no significant change in most developing countries like Nigeria. This is because the risk factors are still prevalent, and the awareness, as well as the huge material and human resources required for mass screening, are lacking.
Diagnosis of cervical carcinoma depends on a high index of suspicion. However, prime clinical findings may include irregular vaginal bleeding, vaginal discharge, lower abdominal pains, and post-coital bleeding. This study is aimed at determining the prevalence of adenocarcinoma among the Igbos with cervical cancer and to assess the relative associations of such factors as age and parity on the disease.
| Materials and methods | |  |
A total of 206 cervical histopathology reports of surgical specimens obtained from patients of the Igbo ethnic group of Nigeria, between January 2007 and December 2010 were used for the study. The tissue blocks for these reports were also retrieved for the study. The surgical specimens with accompanying histopathological forms were obtained from 40 hospitals spread across the five states of South Eastern Nigeria. The reports on specimen taken from patients at National Orthopedic Hospital, Enugu, venue of the study, were excluded in order to demonstrate the true geographical pattern.
Each specimen was properly labeled with the name, age, ethnic group, address of hospital, date of operation and the referring doctor. Other data obtained from each patient histopathological form included a clinical diagnosis, complaints and its duration, clinical signs, parity and last menstrual period. The already processed paraffin wax blocks were sectioned at 5 μm with rotary microtome and sections were stained with hematoxylin and eosin techniques for general tissue architecture and diagnosis. The stained slides were then viewed and confirmed under high power microscope.
| Results | |  |
Four-year archival records of surgical biopsies, dating from January 2007 to December 2010, and containing 206 cases of diagnosed cervical cancer, were reviewed. The specimens retrieved for the study were from various Government, Mission and private hospitals situated in Eastern Nigeria. The patients' ages, which ranged from 30 to 78 years, were grouped into six age grades. The age and cervical cancer occurrence within these years is shown in [Table 1] and [Figure 1].
None of the cervical cancer patients was nulliparous, 19.5% had 1-4 pregnancies, 45% had 5-8 pregnancies while 35.5% delivered 9 or more children. Eighty and a half percent (80.5%) of the cervical cancer patients were grand multiparous as seen in [Table 2]. A relationship between parity and the incidence of the disease may exist.
Sixty percent (124) of the patients presented with a history of irregular vaginal bleeding alone while 72% (148) presented with a history of irregular vaginal bleeding and post-coital bleeding. Vaginal bleeding was, therefore, a major significant clinical finding (P < 0.05). Fifteen percent (30) of the patients presented with vaginal discharge alone as shown in [Table 3].
Adenocarcinoma was seen in a total of 23 cases (11.5%).
| Discussion | |  |
Approximately 70-75% of cervical carcinomas are squamous cell; the remainder are composed of various types of adenocarcinoma (20-25%), adenosquamous carcinomas (3-5%), and undifferentiated carcinomas. Adenocarcinoma of the cervix is derived from the glandular elements of the cervix [Figure 2]. The incidence of adenocarcinomas, including the mucinous, endometrioid, clear cell, and serous types, has been rising over the last several decades, especially in women younger than 35 years of age. [12] Part of this increase may be a result of an increasing prevalence of HPV infection and part may be a result of improvements in screening and prevention of squamous preinvasive disease, thus leading to a histologic shift towards adenocarcinoma. [3] The villiglandular-papillary variety of adenocarcinoma of the cervix tends to occur in younger women and have a more favorable prognosis. [13]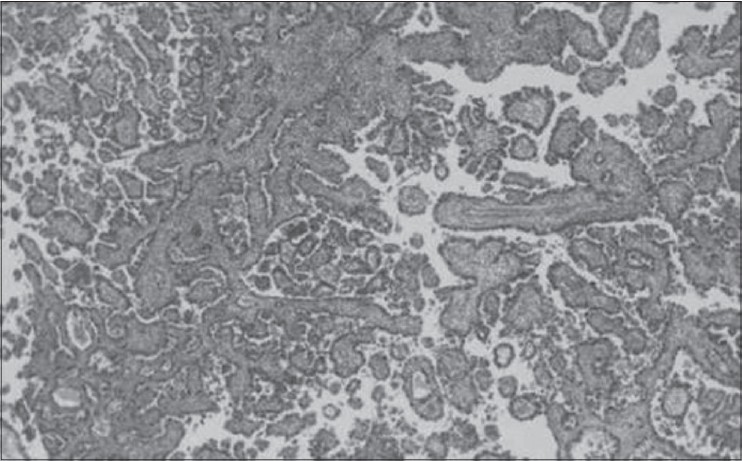 | Figure 2: Photomicrograph of clear cell adenocarcinoma of the cervix showing numerous glands and cancer cell infi ltration (H and E, ×40)
Click here to view |
Most of the cases of cervical cancer in this study were seen in the peri-menopausal or post-menopausal periods. According to Edington and Gilles, peri-menopausal women are frequently affected by cervical carcinoma in the tropics. [14] This is true of the Igbos. [15] Cervical cancer is the second commonest malignancy seen in females in Nigeria and East Africa after breast cancer. [14] It is therefore of national importance as the present mortality from the disease is appalling. The mean age of presentation of cervical carcinoma in this study was in the sixth decade of life, about 20 years above the age reported in advanced countries like USA. [16] Most patients present too late at the hospital for curative therapy as the facilities for early screening and detection are grossly inadequate. The resources used in carrying out the hysterectomies in patients with the attendant high mortality may be better channeled to the preventive stage of the disease. The high incidence rate and the late presentation of the disease emphasize the importance of the tumor in Nigeria. [15]
The age of the patient was given in 200 (97.1%) of the histopathological reports. All histopathological forms must be filled correctly and must contain the patients' age and another clinical date as contained in the form. Errors in omitting the age or giving a wrong age will affect future screening programs. Future screening programs and awareness campaigns should include all girls above 20 years since the disease is beginning to appear in much younger women <30 years. [12],[17]
The steady increase in the yearly occurrence of the disease from 2007 to 2010 is worrisome. The number of cervical cancer patients seen in 2007 had doubled by 2010 [Table 2]. In all probability, with increasing morbidity and mortality, there is decreasing workforce and productivity. Hence, more awareness should be created by the relevant government agencies and more screening centres established to check the rising trend.
The finding that none of the cervical cancer patients in the study was nulliparous is very significant and agrees with earlier studies. [18] The disease is very rare in nuns.
The percentage of adenocarcinoma seen in this study is similar to that noted in the series from other parts of the world where it accounts for approximately 20% of malignant cervical tumors. [18] The screening based on exfoliative cytology introduced in the 1950s by Papanicolau, followed by colposcopy in appropriate patients, is an effective method for identifying squamous intraepithelial lesions. [19],[20] The goals of colposcopy are to identify suspicious areas that require biopsy and to determine the extent of the lesions. Treatment of intraepithelial lesion is determined on the basis of the histological diagnosis and the extent of the lesions on colposcopic examination. [20] Unfortunately, the Pap-smear screening is less efficient or even of no benefit in cervical adenocarcinomas [Figrue 2]. [21] A marked decrease in the incidence of cervical squamous cell carcinoma in the last decades in advanced countries, thanks to the screening, appears to be in contrast to the increasing rate of cervical adenocarcinomas. [3],[4]
The question whether cervical clear cell adenocarcinoma and adenocarcinoma have worse prognosis than squamous cell carcinoma of the uterine cervix remains open. [22] Korhonen suggested, after the analysis of 163 cases of primary cervical adenocarcinoma of different subtypes that the prognosis of clear cell carcinomas is similar to that of non-clear cell cervical adenocarcinomas. [23]
While the antecedents of adenocarcinoma of the cervix and its natural history are uncertain, clinical opinion holds that the prognosis for survival is less than that of patients with squamous cell carcinoma. [24] Several studies have shown that adenocarcinoma confers a worse prognosis with higher rates of nodal involvement, distant metastasis, and decreased survival across stages, compared with squamous cell carcinoma. [4],[25],[26] Few studies have demonstrated the distinct molecular profiles between squamous cell carcinoma and adenocarcinoma that explain the observed clinical differences. [27] A graver prognosis may be expected in a disease which is not usually discovered in the pre-invasive stage by screening techniques, which may remain clinically undetected while advancing in the endocervical canal and which is said to be more resistant to radiotherapy than squamous cell carcinoma. [25] Patients treated with irradiation and conservative hysterectomy may have a better 5-year survival rates, up to 85%. [26]
If parity reflects the coital etiological factors associated with squamous cell carcinoma, then these factors are of lesser importance in the development of adenocarcinoma. Reports have suggested that adenocarcinoma of the cervix is perhaps related to the use of hormonal contraceptives by women. [27] There is an absolute lack of clinical data on the use of hormonal contraceptives in the histopathological forms used in this study. Further studies are necessary to clarify this issue, especially the role of prolonged use of the contraceptives.
| Conclusion | |  |
In view of the increasing prevalence and mortality of adenocarcinoma amongst the Igbos of Nigeria, early and periodic screening is inevitable. This will ensure early detection and commencement of therapy and a better survival rate.
| Acknowledgment | |  |
The authors would like to thank the management of National Orthopaedic Hospital, Enugu for allowing us make use of their Histopathology laboratory.
| References | |  |
| 1. | Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:69-90.  |
| 2. | Thomas J, Ojemakinde O, Izebvaye I. Current concepts in cervical carcinogenesis and new perspectives in prevention. Arch Ib Med Reprod Health 2002;3:36-7.  |
| 3. | Wang SS, Sherman ME, Hildesheim A, Lacey JV Jr, Devesa S. Cervical adenocarcinoma and squamous cell carcinoma incidence trends among white women and black women in the United States for 1976-2000. Cancer 2004;100:1035-44.  |
| 4. | Galic V, Herzog TJ, Lewin SN, Neugut AI, Burke WM, Lu YS, et al. Prognostic significance of adenocarcinoma histology in women with cervical cancer. Gynecol Oncol 2012;125:287-91.  |
| 5. | Kessler II. Human cervical cancer as a venereal disease. Cancer Res 1976;36:783-91.  |
| 6. | Hendershot GE. Coitus-related cervical cancer risk factors: Trends and differentials in racial and religious groups. Am J Public Health 1983;73:299-301.  |
| 7. | Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999;189:12-9.  |
| 8. | Winkelstein W Jr. Smoking and cervical cancer - current status: A review. Am J Epidemiol 1990;131:945-57.  |
| 9. | Luesley D, Blomfield P, Dunn J, Shafi M, Chenoy R, Buxton J. Cigarette smoking and histological outcome in women with mildly dyskaryotic cervical smears. Br J Obstet Gynaecol 1994;101:49-52.  |
| 10. | Kai LJ, Raju K, Malligere Lingaiah HK, Mariyappa N. Significance of blood group and social factors in carcinoma cervix in a semi-urban population in India. Asian Pac J Cancer Prev 2013;14:4811-4.  |
| 11. | Barber HR. Incidence, prevalence and medicine survival rate of gynecologic cancer. In: Wright J, editor. Modern Concepts of Gynecologic Oncology. Boston: PSG; 1982. p. 1-19.  |
| 12. | Liu S, Semenciw R, Mao Y. Cervical cancer: The increasing incidence of adenocarcinoma and adenosquamous carcinoma in younger women. CMAJ 2001;164:1151-2.  |
| 13. | Utsugi K, Shimizu Y, Akiyama F, Umezawa S, Hasumi K. Clinicopathologic features of villoglandular papillary adenocarcinoma of the uterine cervix. Gynecol Oncol 2004;92:64-70.  |
| 14. | Edington GM, Gilles HM. Pathology in the Tropics. London: Arnold Pub; 1969. p. 546-58.  |
| 15. | Onuigbo WI. Carcinoma of the uterine cervix in Nigerian Igbos. Gynecol Oncol 1976;4:255-8.  |
| 16. | Benedet JL, Bender H, Jones H, Ngan HY, Pecorelli S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet 2000;70:209-62.  |
| 17. | La Veechi C, Franceschi S. Invasive cervical cancer in young women. Br J Obstet Gynaecol 1984;91:1149-50.  |
| 18. | Macleod A, Kitchener HC, Parkin DE, Sarkar T, Miller ID, Mann E, et al. Cervical carcinoma in the Grampian region (1980-1991): A population-based study of survival and cervical cytology history. Br J Obstet Gynaecol 1994;101:797-803.  |
| 19. | Cannistra SA, Niloff JM. Cancer of the uterine cervix. N Engl J Med 1996;334:1030-8.  |
| 20. | Quinn MA. Adenocarcinoma of the cervix. Ann Acad Med Singapore 1998;27:662-5.  |
| 21. | Freitag P, Macku J, Nouzová K. Adenocarcinoma of the uterine cervix - retrospective clinico-pathologic study. Ceska Gynekol 1996;61:162-4.  |
| 22. | Gottwald L, Korczynski J, Góra E, Kusinska R, Rogowska E, Wójcik-Krowiranda K, et al. Clear cell adenocarcinoma of the uterine cervix in a 24-year-old woman. Case report and review of the literature. Arch Med Sci 2012;8:578-81.  |
| 23. | Korhonen MO. Adenocarcinoma of the uterine cervix. Prognosis and prognostic significance of histology. Cancer 1984;53:1760-3.  |
| 24. | Tasker JT, Collins JA. Adenocarcinoma of the uterine cervix. Am J Obstet Gynecol 1974;118:344-8.  |
| 25. | Eifel PJ, Burke TW, Morris M, Smith TL. Adenocarcinoma as an independent risk factor for disease recurrence in patients with stage IB cervical carcinoma. Gynecol Oncol 1995;59:38-44.  |
| 26. | Lee YY, Choi CH, Kim TJ, Lee JW, Kim BG, Lee JH, et al. A comparison of pure adenocarcinoma and squamous cell carcinoma of the cervix after radical hysterectomy in stage IB-IIA. Gynecol Oncol 2011;120:439-43.  |
| 27. | Wright AA, Howitt BE, Myers AP, Dahlberg SE, Palescandolo E, Van Hummelen P, et al. Oncogenic mutations in cervical cancer: Genomic differences between adenocarcinomas and squamous cell carcinomas of the cervix. Cancer 2013;119:3776-83.  |
[Figure 1], [Figure 2]
[Table 1], [Table 2], [Table 3]
|