|
 
 |
| CASE REPORT |
|
| Year : 2014 | Volume
: 9
| Issue : 3 | Page : 132-134 |
|
Ossiculum odontoideum
FU Uduma1, M Motah2, JKC Emejulu3
1 Department of Radiology, Faculty of Clinical Sciences, College of Health Sciences, University of Uyo, Uyo, Nigeria; Polyclinic Bonanlo, Douala, Cameroon
2 Department of Surgery, Neuro Surgical Unit, University of Douala; Polyclinic Bonanlo, Douala, Cameroon
3 Department of Surgery, Neuro Surgical Unit, Nnamdi Azikiwe University, Teaching Hospital, Awka, Nigeria
| Date of Web Publication | 15-Nov-2014 |
Correspondence Address:
F U Uduma
Department of Radiology, Faculty of Clinical Sciences, College of Health Sciences, University of Uyo, Uyo, Nigeria, Polyclinic Bonanlo, Douala, Cameroon
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/9783-1230.144777

Ossiculum (Os) odontoideum (OD) is a round or oval well corticated ossicle separated by a gap from the base of the dens of the axis vertebra. It is considered as a congenital or acquired condition. It could also be orthotropic or dystopic. We present an uncommon case of a 20-year-old male with OD and neck pain. Known complications of OD such as atlanto-axial instability, degenerative changes, spinal stenosis, and focal myelomalacia are also discussed. Keywords: Atlanto-axial, magnetic resonance imaging, ossiculum odontoideum
How to cite this article:
Uduma F U, Motah M, Emejulu J. Ossiculum odontoideum. J Med Investig Pract 2014;9:132-4 |
| Introduction | |  |
Ossiculum (Os) odontoideum (OD) is defined as a separate ossicle from C2 (axis) vertebra with a gap between the base of the dens and the ossicle above it. [1],[2] The etiology is controversial, as it is thought to be congenital or post-traumatic. [3] Most of the os OD are discovered incidentally in routine conventional cervical radiographs. [3]
| Case report | |  |
EB, is a 20-year-old Cameroonian boy with a chronic history of neck pain. No associated history of trauma nor road traffic accident. Motor and reflex testing were normal and symmetric in the upper and lower extremities.
Magnetic resonance imaging (MRI) was carried out. Sagital T1-weighted (T1-W) MRIs showed a hair-line signal void linear lesion located antero-superior to the 2/3 rd of the odontoid process of the axis vertebra [Figure 1]. This lesion is antero-central in coronal T1-W and T2-W images. The superior and inferior borders of this signal void lesion are smooth, but slightly heterogeneous in intensity in both sequences. The distance between the posterior margin of anterior arch of atlas and the anterior margin of the odontoid process of the axis vertebra (atlanto-axial distance) is within normal limits measuring 29 mm. Cervical vertebral heights, anterior and posterior vertebral lines were preserved. The disc cartilages are intact in all sequences. No spinal epidural defect, neural foraminal nor paraspinal lesions seen. A diagnosis of os OD was made. Patient was managed with non-steroidal anti-inflammatory drugs and short period of neck collar usage.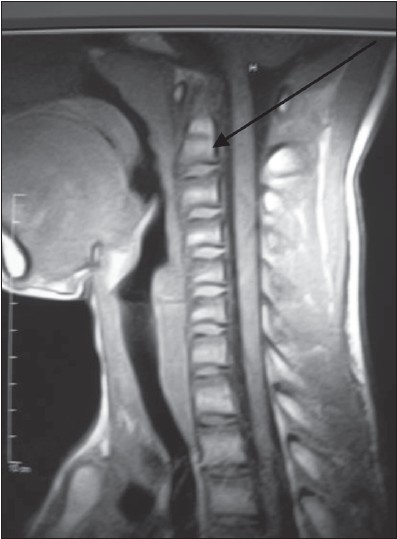 | Figure 1: T1-weighted mid-sagittal magnetic resonance imaging showing a hair-line signal void linear lesion located antero-superior to the odontoid process of the axis vertebra
Click here to view |
| Discussion | |  |
Ossiculum OD is an axial anomaly with an independent os cephalad to the axis body, or it could be in the location of the odontoid process with associated absence of the odontoid process. [4] Os OD appears as a round or oval ossicle with a smooth uniform cortex separated from the base of the axis by a wide gap and this ossicle border does not directly match up with the axis body. [5] The prevalence of cranio-vertebral anomalies remains unknown since they may remain clinically silent. [3]
Odontoideum is considered to be congenital or acquired. It could be part of congenital spectrum of persistent Os terminale (Bergman ossicle), odontoid aplasia, odontoid hypoplasia. [2],[4] The congenital type is thought to be associated with Down's syndrome and Laron syndrome. [1] However traumatic type might just be due to a minor trauma. [2]
There are two basic types of OD, namely the orthotopic and dystopic types. The orthotopic type remains at its normal place, whereas the dystopic type migrate near the foramen magnum. [2] A dystopic ossicle may be fixed to the clivus or to the anterior ring of the atlas. [5]
Odontoideum is usually clinically asymptomatic except if there are an accompanying complications. Such complications are multi-directional cervical instability (like atlanto-axial instability), degenerative changes of atlanto-axial joint, spinal stenosis, focal myelomalacia, cervical spondylotic cord compression, cord signal abnormality, vascular compression, and even death. Signs and symptoms may be mild local neck pain to transient or progressive myelopathy, vertebra-basilar ischaemia, quadriparesis, radiating upper limb pains and occipital neuralgia. [3]
Odontoideum whether congenital osseous malformations or a prior unrecognized trauma, requires same radiological work-ups. [3] Radiological investigations are to confirm the diagnosis and estimate the degree of spinal instability. Initial evaluation includes neutral cervical radiograph, open mouth view, anterior-posterior radiograph and flexion-extension lateral cervical radiographs (dynamic lateral radiographs). Dynamic lateral radiographs differentiate the un-fused neuro-central synchondrosis in children (<5 years whose synchondrosis often are not fused). In dynamic lateral radiograph, unfused synchondrosis do not move, whereas OD moves. [5] However, movement >3 mm of the space between a line projected superiorly from the anterior border of the axis and a line projected inferiorly from the posterior border of the anterior arch of the atlas is suggestive of atlanto-axial subluxation. [5] This occurs when pre-dental space is >2.5 mm in adults, >4.5 mm in children and retro-dental space (posterior atlanto dental index [PADI]) <18 mm. If PADI is reduced, patient complains of electric shocks radiating down the body (Lhermitte sign) and progressive weakness and ataxia. [5]
Odontoideum is differentiated from odontoid fracture as the margin of the ossicle is well defined and corticated. Atlanto-axial subluxation are of three types, type 1 is due to odontoid abnormality, type 2 is due to ligament deficiencies and type 3 is rotatory fixation. [6] Posterior atlanto-axial subluxation unlike anterior subluxation in a patient with os OD is extremely rare. [7]
Sectional imaging like computed tomography (CT) and MRI have revolutionized OD study. CT can show the ossicle and ossicle to spino-laminar distance (PADI) which is measured directly on reconstructed images. Also, CT can show the cortication of the os differentiating it from odontoid fracture. CT on reconstruction can easily show dystrophic ossicle to the clivus. Hypertrophy and sclerosis of the anterior tubercle of the atlas has been used to differentiate OD from acute fracture of dens. [8] MRI can evaluate the cord compression, canal stenosis, hyperintense T2-W of myelomalacia. MRA can show the compromise vertebra-basilar artery in vertebra-basilar ischemia. [3],[5] The thickened or hypertrophy of the ligament between the ossicle and axis is best demonstrated by MRI. CT and MRI have greatly advanced our understanding of os OD and its associated neuro-vascular compromise. [2] Another indicator of atlanto-axial instability is the instability index measuring the dynamic sagittal diameter of the spinal canal. It is calculated as the maximum diameter minus minimum diameter/maximum diameter multiply by 100. [3] Henderson and Henderson measured the maximum anterior-posterior diameter of the spinal canal as 28 mm and the minimum anterior posterior diameter of the spinal canal as 18 mm in their case studied yielding an index of 35.7% consistent with severe atlanto-axial dislocation. In severe cases, treatment option include operation for stabilization and fusion of the atlanto-axial articulation. It could be done with C1 lateral mass screws and rod instrumentation. [9] Surgical stabilization of C1-C2 articulation is indicated if there is neurological involvement >10 mm of instability on supervised extension films or persistent neck complaints. However, prophylactic surgery is controversial. [10]
| Conclusion | |  |
Ossiculum OD is a corticated ossicle separate from the dens and can be orthotopic or dystopic. Its origin is congenital or from minor trauma. It is usually asymptomatic and seen as an incidental radiological finding. Complications like atlanto-axial dislocation, cervical spinal stenosis and even death can occur.
| References | |  |
| 1. | Kornreich L, Horev G, Schwarz M, Karmazyn B, Laron Z. Laron syndrome abnormalities: Spinal stenosis, os odontoideum, degenerative changes of the atlanto-odontoid joint, and small oropharynx. AJNR Am J Neuroradiol 2002;23:625-31.  |
| 2. | Qureshi MA, Afzal W, Malik AS, Ullah JS, Aebi M. Os-odontoideum leading to atlanto-axial instability - report of surgery in four cases. J Pak Med Assoc 2008;58:640-2.  |
| 3. | Henderson S, Henderson D. Os odontoideum with associated multidirectional atlantoaxial instability: Imaging and clinical considerations. J Can Chiropr Assoc 2006;50:111-7.  |
| 4. | Dahnert W. Radiology Review Manual. 6 th ed.: Wolters Kluwer/Lippincort Williams and Wilkins; 2007. p. 183-4.  |
| 5. | Truumes E, Keenan ME. Os odontoideum treatment and management. Available from: http://www.emedicine.medscape.com/article/1265065-treatment. [Last accessed on 2013 May 25; Last updated on 2012].  |
| 6. | Fielding JW, Hawkins RJ, Ratzan SA. Spine fusion for atlanto-axial instability. J Bone Joint Surg Am 1976;58:400-7.  |
| 7. | Motosuneya T, Hirabayashi S, Yamada H, Kobayashi Y, Sekiya S, Sakai H. Posterior atlantoaxial subluxation due to os odontoideum combined with cervical spondylotic myelopathy: A case report. Eur Spine J 2008;17 Suppl 2:S275-9.  |
| 8. | Vickers ED. Atlantoaxial anomalies with particular emphasis on os odontoideum. J Manipulative Physiol Ther 1990;13:471-6.  |
| 9. | Images in spine surgery: Os odontoideum. JMPA 2006. Available from: http://www.jpma.org.pk/full_article_text.php?article_id=896. [Last accessed on 2013 Jun 38].  |
| 10. | Wills BP, Dormans JP. Nontraumatic upper cervical spine instability in children. J Am Acad Orthop Surg 2006;14:233-45.  |
[Figure 1]
|