|
 
 |
| CASE REPORT |
|
| Year : 2014 | Volume
: 9
| Issue : 4 | Page : 160-164 |
|
Malaria in non-immune travelers: A case report and reminder for increased awareness of the problem
Shadrach Awa Ukonye Offiah1, Onyesom Ekperi1, Franklin E Igwe2, Simeon O Nwosu2
1 Department of Anatomic Pathology, Abia State University Teaching Hospital, Aba, Nigeria
2 Department of Anatomical Pathology, University of Portharcourt Teaching Hospital, Portharcourt, Nigeria
| Date of Web Publication | 14-May-2015 |
Correspondence Address:
Dr. Shadrach Awa Ukonye Offiah
Department of Anatomic Pathology, Abia State University Teaching Hospital, PMB 7004, Aba, Abia State
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/9783-1230.157061

Malaria presents a serious hazard to travelers to endemic areas. With the current increase of international travel to tropical endemic countries, the fatality and incidence of malaria being imported into nonendemic countries has significantly increased. The risk of malaria infection varies depending on the destination and exposure to infected mosquitoes. A good knowledge of malarious areas and the frequency of infection acquired by nonimmune travelers are necessary when advice for prophylaxis is given by a physician to a prospective traveler. We discuss the case of a nonimmune, indigenous African from a malaria-free zone in Africa, who was not on prophylactics against malaria but visited a malaria-holoendemic region of Nigeria. Malaria remains a killer, especially to the nonimmune traveler; therefore, the need to carry a potent antimalarial drug for emergency treatment when traveling to a malarious country need not be overemphasized. Keywords: Malarious, Nonimmune, Shock, Slatey-grey
How to cite this article:
Offiah SU, Ekperi O, Igwe FE, Nwosu SO. Malaria in non-immune travelers: A case report and reminder for increased awareness of the problem. J Med Investig Pract 2014;9:160-4 |
How to cite this URL:
Offiah SU, Ekperi O, Igwe FE, Nwosu SO. Malaria in non-immune travelers: A case report and reminder for increased awareness of the problem. J Med Investig Pract [serial online] 2014 [cited 2018 Aug 24];9:160-4. Available from: http://www.jomip.org/text.asp?2014/9/4/160/157061 |
| Introduction | |  |
Malaria is a life-threatening disease caused by the protozoan parasites (Plasmodia) that are transmitted to people through the bites of infected mosquitoes. Four Plasmodium species that cause malaria in humans are Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale and Plasmodium malariae. It is well known that P. falciparum and P. vivax are the most common while P. falciparum is the most deadly.
The intensity of malaria transmission is dependent on factors related to the human host, his environment, the vector mosquitoes, and then the parasite. Transmission is more intense in places where the mosquitoes' life-span is longer (for the parasite to have enough time to complete its development inside the mosquitoes) and where it prefers to bite humans rather than other animals. [1]
Human immunity plays a vital role in malaria transmission, especially among adults, in areas of moderate to intense transmission conditions. Partial immunity is developed over years of exposure though it never provides complete protection; it does reduce the risk of severe disease. Most malaria deaths in the tropics, therefore, occur in children but all age groups are at risk in areas with less transmission and low level of immunity. Persons in malaria-endemic areas may develop partial immunity, allowing asymptomatic infections to occur.
Malaria presents as an acute febrile illness in nonimmune individuals. Symptoms appear within 14 days after an infective mosquito bite. Symptoms of fever, headache, vomiting, and chill may be very mild and hence difficult to recognize as malaria. P. falciparum malaria can progress to severe illness often leading to death if not treated within 24 h. Severe anemia, respiratory distress in relation to metabolic acidosis or cerebral malaria, is some symptoms of severe malaria in children. In adults, multiorgan involvement is frequent.
Approximately half of the world population is at risk of malaria. Most malaria cases and deaths occur in tropical Africa; however Asia, Latin America, and to a lesser extent the Middle East and parts of Europe are also affected. In the year 2013, 97 countries and territories had on-going malaria transmission. [1] Specific population groups at risk include: Young children in stable transmission areas, nonimmune pregnant women, Semi-immune pregnant women in areas of high transmission, semi-immune HIV-infected pregnant women in stable transmission areas, people with HIV/AIDS, international travelers from nonendemic areas, immigrants from endemic areas and their children living in nonendemic areas and returning to their endemic home countries for a visit.
In this series, we present a case of fatal malaria in a nonimmune traveler, an under-reported phenomenon. Our aim is to create reasonable awareness and accentuate the magnitude of the health problem. Although malaria is very common in Nigeria, cases are usually reported and autopsied, but there is paucity of publications in the literature on cases and/or fatality of malaria in nonimmune visitors to this environment, thus making this case worth reporting so as to avail tool for heightening preventive measures.
| Case Report | |  |
ABC is a 31-year-old, P1 +0 black female from Cape Town region of South Africa, married to a Nigerian of Southeastern extraction. The family was on a visit to the husband's native home for a Christmas festive period. After a total of 14 days stay in Nigeria, preparation was in top gear for family to return to their base in Cape Town, subject is alleged to have suddenly developed fever, headache, diarrhea and vomiting for which 2 tablets (1000 mg) of paracetamol was given. When her condition worsens, and she became drowsy and diaphoretic, subject was rushed to a peripheral private clinic from where she was referred to our establishment (Abia State University Teaching Hospital) where she was certified dead-on-arrival. Death occurred within 48 h of onset of symptoms.
At autopsy, the body received was that of an obese black woman with no external marks of violence. There was central and Peripheral cyanosis as shown in [Figure 1]. Dehydration could not be elicited because the body was embalmed. Internal examination showed a left ventricular wall thickness of 1.5 cm; there was no coronary atherosclerosis. Both lungs were congested and edematous, the cut surfaces were wet and oozing frothy fluid on compression. There was congestive hepatosplenomegaly with Slatey-grey spleen as shown in [Figure 2]. Both kidneys showed Shock changes as illustrated in [Figure 3], and the intestinal mucosa was unremarkable. The brain was autolyzed while other organs remained essentially anatomic. | Figure 3: Cortical pallor with clear corticomedullary differentiation (shock kidneys)
Click here to view |
Commentary
The slatey-grey color of the spleen is typical of malaria. The shock kidneys are as a result of fluid loss from diarrhea and vomiting.
Diagnosis
Based on pertinent clinical history and anatomical findings; death was ascribed to hypovolemic shock due to severe malaria.
| Discussion | |  |
Malaria is designated the most dangerous parasitic disease of humans. It infects about 5% of the world's population. Being resurgent, malaria causes about one million deaths each year. [2] The disease's strong resurgence is attributed to the effects of war, climatic change, mass population movement, rapid drug and insecticide resistance and poor public health infrastructure. Malaria is currently endemic in over 100 countries of the world. [3],[4]
The key facts about malaria are that the disease is life-threatening and that it is caused by parasites that are transmitted to people through the bites of infected mosquitoes. In the year 2012, malaria is said to have caused an estimated death of 627,000 (with an uncertainty range of 473,000-789,000), mostly among African children. [4] Increased malaria prevention and control measures are drastically reducing the burden of the disease in many places, but the malady still remains a menace to travelers, especially the nonimmune from malaria-free areas. This is because this group of people is very vulnerable to the disease when they get infected.
The 2011 International Travel and Health Book posits that about 125 million travelers visit malaria endemic countries annually and that over 10,000 malaria cases are reported after returning home. [5] Not all these travelers have similar risks; the risk of acquiring malaria for travelers varies from region to region and it depends on many factors, such as type and intensity of transmission, the style of travel, the duration of stay at the endemic area, the preventive measures adopted if any, and the individual's susceptibility. [6]
With the current increase of international travels to tropical endemic regions, the fatality of malaria especially to the nonimmune travelers and the incidence of malaria importation into the nonendemic countries have substantially increased. [7] The risk of infection is obviously highest in the tropical Africa and the fatality peaks in the nonimmune travelers that are not on prophylactic medication. Our subject in this report is a nonimmune, nonprophylactic traveler from a malaria-free region (Cape Town in South Africa) on a visit to a malaria-holoendemic region (South-eastern Nigeria).
The latest estimates released by WHO in December 2013 shows that 207 million malaria cases (with uncertainty range of 135 million - 287 million) was reported in 2012; and that an estimated 627,000 deaths occurred from this reported cases. Though malaria mortality rate is said to have fallen by 42% and 49% globally and in African region, respectively, since the year 2000, [1] but today the disease still presents a serious hazard to mankind especially the nonimmune. Askling et al. in the article of their study in Sweden, [6] posited that the risk of malaria to travelers is 302/100,000 for visitors to West Africa; 7.2/100,000 for visitors to South America; and 2/100,000 for visitors to Thailand. This risk seems not to have abated today, compared to the time of their report.
Geographical distribution
The 2010 distribution of malaria in the world, as published by WHO is as shown on the map in [Figure 4].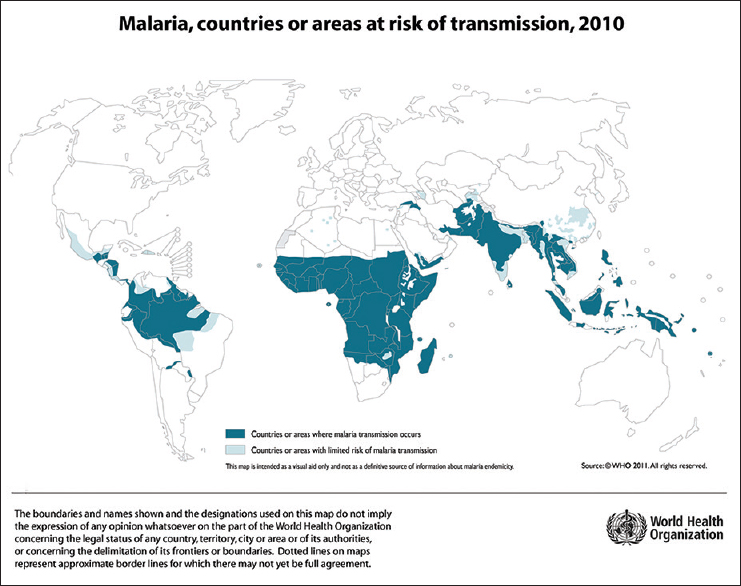 | Figure 4: Malaria, countries or areas at risk of transmission (WHO, 2010)
Click here to view |
The affected countries and territories are as delineated on the map. The variability of malaria contracting risk must be put into consideration in any suggestion concerning appropriate preventive measures. The urban areas are relatively free of malaria transmission in many countries. However, countries in sub-Saharan Africa and India are of serious concern; these countries are characterized by high levels of malaria transmission and wide spread reports of insecticide resistance by mosquitoes. [1] Malaria is, therefore, known to occur in the main urban areas of Africa and India.
The risk of malaria is drastically less at altitudes above 3000 m. [7] There is no malaria risk in many tourists' destinations in Southeast Asia, the Caribbean, and Latin America. Four countries have recently been certified by the WHO Director General as having eliminated malaria; these include the United Arab Emirate (2007), Morocco (2010), Turkmenistan (2010) and Armenia (2011). [7],[8]
Transmission
Malaria is exclusively transmitted through the bites of female Anopheles mosquitoes. The intensity of transmission depends on factors related to the parasite itself, the mosquito vector, the human host, and the environment. About 3200 mosquito species have so far been described, 430 of these are estimated to belong to the genus Anopheles. About 70 of the Anopheline species are known to transmit malaria, and about 40 species are considered important vectors. [9] All mosquitoes feed on nectar; only the gravid females of the mosquitoes of medical importance (with the exception of megharine mosquitoes) are blood suckers. Once they are fertilized, they are wholly or partly dependent on obtaining blood-meal to ripen their eggs before laying them for the propagation of their species. The source of the blood meal varies according to the species and subspecies. Most Anophelines are night feeders and anthropophilic; the diseases they transmit are most commonly acquired during the night, and in the case of a man, are most often contracted indoors than out-doors. [10]
These vectors fly high and long searching for the scent trail of a suitable host, [10],[11] and are attracted to their human host over a range of 7-20 m via a variety of stimuli such as warmth, moisture, exhaled carbon dioxide, lactic acid, and other host odors. [12],[13],[14] Mosquitoes have been shown to bite larger people more than smaller individuals, and women receive more bites in trials than men. [14],[15],[16] Our index case is a large obese woman. The reason for this sex disparity in bites is not known. Children have been shown to usually receive lower mosquito bites than adults; [15] this may be as a result of their secreting lower levels of chemical attractants than adults.
Malaria transmission hardly occurs at temperatures above 35°C or below 16°C, or at altitudes >3000 m above sea level at the equator. [16] This is because the development of the sporozoites in the mosquito does not take place at these climatic conditions, and the mosquito population and survival are also adversely affected. The optimal conditions for transmission, therefore, are ambient temperature of 25-30°C and a humidity of over 60%. Transmission is seasonal in many places, and peaks during, and/or, just after the rainy season. [16],[17]
Epidemics of malaria are usually observed when the climatic and other conditions suddenly favor transmission, especially in areas where people have little or no immunity against the disease. It is also observed when people with little or low immunity migrate into an endemic/holoendemic areas either to find work or as refugees. [18]
Clinical presentation
Signs and symptoms of malaria are caused by the presence in the red blood cells of the erythrocytic stages of the parasite. In the falciparum malaria, only the blood forms of the parasite exist. There is an additional persistent infection in the liver (the exoerythrocytic form) in all other forms of malaria, and it is the factor responsible for relapses. Clinical picture is that of recurrent rigors, anemia, toxemia, and splenomegaly.
Pathological changes
The pathological changes in malaria are related to the development of asexual parasites in the blood. Several organs of the body are affected by the Plasmodium species, which parasitize erythrocytes. The small blood vessels ramifying the major organs are usually filled with parasitized red blood cells. This represents the major morphological changes seen in malaria. Other findings include congestion, hyperemia, and widespread hemozoin deposition in organs and scattered petechial hemorrhages in various organs of the body. More specific findings are ring hemorrhages and durck granuloma in the brain, hyaline membranes in the lungs, fatty changes in the liver, brown atrophy in the heart, and fatty degeneration of the myofibrils.
Immunity against malaria
Human immunity against malaria is an important factor to reckon with when considering the transmission, susceptibility, morbidity, and mortality of the disease. The complex multistage life cycle of malaria parasite is characterized by its expression of a great variety of proteins at different stages. These proteins keep changing often, and, as a result, natural infection with the malaria parasite often leads to a partial and short-lived immunity unable to protect the host against a new infection. The complex interplay of these parasite proteins with the host's immune system makes it difficult to develop an effective vaccine against the infection. [19]
Natural or innate immunity, an inherent ability of the host to prevent the establishment of an infection, is not dependent on any previous exposure to the parasite. Red cells' Duffy negativity, widely prevalent in Africa, protects against P. vivax infection, and this may be responsible for the virtual elimination of P. vivax from the African continent. Active or acquired immunity develops following infections, and it varies in efficacy depending on the host's characteristics, the intensity of infection, and place of stay. When this immunity protects against clinical disease it is referred to as anti-disease immunity; if it protects against high parasitemia-antiparasite immunity; when against new infection by maintaining a low grade asymptomatic parasitemia, it is referred to as premunition or sterilizing immunity (characterized by asymptomatic presence of small quantity of residual parasites in the liver during the exoerythrocytic stage.). In nonimmune individuals, very low levels of parasitemia following infection results in acute clinical illness and may progress to severe disease and death. [20]
The acquisition of immunity against malaria is very slow, poorly effective, and is both species and strain specific with cross-reactivity. This is as a result of the presence of genetically/antigenically distinct strain of the parasite in a given locality and also the occurrence of clonal antigenic variation during the course of an infection. [20],[21] The level of antimalarial immunity tend to influence the clinical outcome of the disease with respect to age groups, conditions, and locations. [22] The underlying mechanisms and antigenic specificity of protections against malaria are yet to be elucidated. Malaria parasites have been shown to evade the host's immune response by their antigenic diversity, clonal antigenic variation, and by modulation of the immune response, thereby causing immune suppression. The parasitized red cells have been shown to inhibit the maturation of antigen presenting cells, and hence reducing their interaction with T-cells eventually leading to immunosuppression. Immunity is also rendered less effective in pregnancy, especially during the 1 st and 2 nd pregnancies. This is due to physiological immunosuppression and the cytoadherence of erythrocytes to chondroitin-sulfate receptors on the placenta. Thus the pregnant woman is rendered more susceptible to malaria and its complications. [20],[22]
| Conclusion | |  |
Malaria still remains a global health problem, especially to the nonimmune travelers that are not on prophylactic medication and are moving from a malaria-free region to malaria-endemic area. The disease is as preventable as it is curable. It is advisable for travelers to carry a potent antimalarial drug for emergency treatment. Long-term travelers and frequent visitors to malarious countries should be advised and informed about the symptoms, signs and diagnosis of the disease; access to and identification of medical assistance and qualified staff, and advice on measures against mosquito bites. Chemoprophylaxis should be adapted to each traveler's individual susceptibility, the plan of journey and types of drugs used.
| References | |  |
| 1. | WHO. Malaria Fact Sheet. World Malaria Report; 2013. p. 87-92.  |
| 2. | Ashley MC. Malaria prevention in travelers. BMJ Clin Evid 2007;903:1-5.  |
| 3. | WHO. International Travel and Health. 2003 rd ed. Geneva: WHO; p. 65-82. available from: http://www.whoint/ith/en. [Last accessed on 2012 May].  |
| 4. | Martens P, Hall L. Malaria on the move: Human population movement and malaria transmission. Emerg Infect Dis 2000;6:103-9.  |
| 5. | WHO. International Travel and Health. 2011 th ed. Geneva: WHO; p. 125-48. available from: http://www.whoint/ith/en. [Last accessed on 2014 Apr].  |
| 6. | Askling HH, Nilsson J, Tegnell A, Janzon R, Ekdahl K. Malaria risk in travelers. Emerg Infect Dis 2005;11:436-41.  |
| 7. | Jelinek T, Nothdurft HD, Löscher T. Malaria in nonimmune travelers: A synopsis of history, symptoms, and treatment in 160 patients. J Travel Med 1994;1:199-202.  |
| 8. | WHO. International Travel and Health. 2014 th ed. Geneva: WHO; p. 216-42. available from: http://www.whoint/ith/en. [Last accessed on 2015 Feb].  |
| 9. | Renshaw M, Silver JB. Malaria, human. In: Service MW, editor. Encyclopedia of Arthropod-transmitted Infections of Man and Domesticated Animals. New York: CABI Publishing; 2001. p. 314-27.  |
| 10. | Gilles MT. Anopheline mosquitoes: Vector behavior and bionomics. In: Wernsdorfor WH, McGregor I, editors. Malaria: Principles and Practice of Malariology. Edinburgh: Churchill Livingstone; 1988. p. 453-85.  |
| 11. | Baudon D. Malaria and travelers - Practical aspects. Trop Med Parasitol 1993;44:246-9.  |
| 12. | de Glanville H. Bilingual dialogue on malaria. Lancet 1994;343:593.  |
| 13. | Service MW, Townson H. The anopheles vector. In: Warreck DA, Gilles HM, editors. Essential Malariology. 4 th ed. London: Arnold; 2002. p. 59-84.  |
| 14. | Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes AM, Yohannes M, et al. Incidence of malaria among children living near dams in northern Ethiopia: Community based incidence survey. BMJ 1999;319:663-6.  |
| 15. | White GB. Medical acarology and entomology. In: Cook GC, Zumla AI, editors. Manson′s Tropical Diseases. 21 st ed. London: Saunders; 2003. p. 1717-825.  |
| 16. | Steffen R, Behrens RH. Travellers′ malaria. Parasitol Today 1992;8:61-6.  |
| 17. | Goodyer LT. Travel Medicine for Health Professionals. London: Pharmaceutical Press; 2004. p. 126-9.  |
| 18. | Golenda CF, Solberg VB, Burge R, Gambel JM, Wirtz RA. Gender-related efficacy difference to an extended duration formulation of topical N, N-diethyl-m-toluamide (DEET). Am J Trop Med Hyg 1999;60:654-7.  |
| 19. | Carter R, Mendis KN. Evolutionary and historical aspects of the burden of malaria. Clin Microbiol Rev 2002;15:564-94.  |
| 20. | Perlmann P, Troye-Blomberg M. Malaria and the immune system in humans. Chem Immunol 2002;80:229-42.  |
| 21. | Stevenson MM, Riley EM. Innate immunity to malaria. Nat Rev Immunol 2004;4:169-80.  |
| 22. | Doolan DL, Dobaño C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev 2009;22:13-36.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|