|
 
 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 10
| Issue : 1 | Page : 30-32 |
|
Cystolithiasis with coexisting nephrolithiasis: A radiodiagnostic discovery in an adult Nigerian male with lower urinary tract symptoms
Olufunso Simisola Aduayi, Olusola Comfort Famurewa
Department of Radiology, Obafemi Awolowo University Teaching Hospital, Ile-Ife, Osun State, Nigeria
| Date of Web Publication | 4-Nov-2015 |
Correspondence Address:
Dr. Olufunso Simisola Aduayi
P.O. Box 2039, Obafemi Awolowo University, Ile-Ife, Osun State
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/9783-1230.169055

Urolithiasis is a broad term for the presence of calculi or stones along the urinary tract and these may be found in the kidneys (nephrolithiasis), ureters (ureterolithiasis), bladder (cystolithiasis) or urethra (urethrolithiasis). A 50-year-old man presented with lower urinary tract symptoms which had progressively worsened over a period of 10 years. He had radiological, and laboratory investigations done. Imaging findings revealed the presence of calculi in the bladder and right kidney. The role of radiological imaging in the management of the patient is discussed. Keywords: Calculi, intravenous urography, plain radiography, ultrasonography
How to cite this article:
Aduayi OS, Famurewa OC. Cystolithiasis with coexisting nephrolithiasis: A radiodiagnostic discovery in an adult Nigerian male with lower urinary tract symptoms. J Med Investig Pract 2015;10:30-2 |
How to cite this URL:
Aduayi OS, Famurewa OC. Cystolithiasis with coexisting nephrolithiasis: A radiodiagnostic discovery in an adult Nigerian male with lower urinary tract symptoms. J Med Investig Pract [serial online] 2015 [cited 2018 Aug 17];10:30-2. Available from: http://www.jomip.org/text.asp?2015/10/1/30/169055 |
| Introduction | |  |
Urolithiasis refers to the calcifications that form in the urinary system, primarily in the kidney or ureter, and may also form in or migrate into the lower urinary system (bladder or urethra).[1] It is synonymous with urinary calculi or urinary stones. The medical terms vary depending on the location, and these include kidneys (nephrolithiasis), ureters (ureterolithiasis), bladder (cystolithiasis), or urethra (urethrolithiasis). The world prevalence is estimated to be between 1% and 5% and prevalence in developing countries is 0.5–1%.[2],[3] It occurs more often in males, and most of urinary stone diseases are diagnosed at the fifth decade of life.[3] In males, lower urinary tract symptoms (LUTS) often draws attention to existing obstructive uropathy. This is associated with urinary stasis which in turn predisposes the individual to stone formation and urinary tract infection. Hence, the need for proper radiological evaluation to detect the cause and associated complications of LUTS cannot be overemphasized.
| Case Report | |  |
A 50-year-old man presented with recurrent right-sided lower abdominal pain of 10 years duration. The pain was dull aching and radiated occasionally to the groin and back. No known relieving or aggravating factors. There was associated dysuria, occasional total hematuria, straining on micturition, terminal dribbling, and feeling of incomplete emptying of the bladder.
Past medical history revealed the occurrence of similar pains for almost two decades prior to the current presentation. It was associated with nausea and vomiting but resolved following the spontaneous passage of a ureteric stone. On examination, his general condition was stable. He had radiological, and laboratory investigations done.
Plain abdominal X-ray of the kidney, ureter, and bladder (KUB) showed an oval shaped opacity within the pelvis and another smaller opacity in the right renal bed [Figure 1]. | Figure 1: A plain radiograph is showing an oval shaped calculus within the pelvis (bigger arrow). A calculus is also seen within the right renal bed (smaller arrow)
Click here to view |
An abdominopelvic ultrasound scan showed a large curvilinear echogenic structure casting posterior acoustic shadow within the urinary bladder [Figure 2]. The bladder wall thickness was 4 mm. The prostate gland was moderately enlarged and measured 5.4 cm × 4.0 cm × 5.9 cm in its length, antero-posterior and transverse dimensions with an estimated weight of 70 g. An echogenic foci was also noted within the lower moiety of the right calyceal system, casting a posterior acoustic shadow, associated with moderate calyceal dilatation.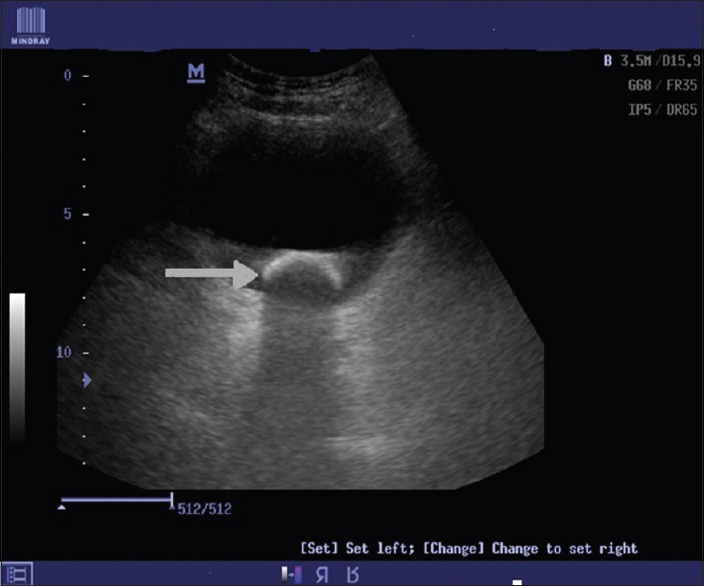 | Figure 2: A transverse pelvic ultrasound scan demonstrating the echogenic rim of a calculus (arrow) casting a posterior acoustic shadow within the bladder
Click here to view |
Intravenous urography (IVU) demonstrated the prompt excretion of contrast bilaterally with moderate right hydronephrotic changes [Figure 3]. | Figure 3: A 30 min intravenous urogram. The stones are obscured; note the right sided pelvicalyceal dilatation
Click here to view |
Electrolyte and urea results were as follows: Bicarbonate - 20 mmol/L, potassium - 3.4 mmol/L, sodium - 138 mmol/L, urea - 5.6 mmol/L, and creatinine 63 μmol/L.
The full blood count was within the normal limits. Urinalysis was also within the normal limits. However, urine microscopy, culture, and sensitivity (MCS) suggested the presence of urinary tract infection as culture yielded significant growth of Klebsiella, which was sensitive to cefixime, ofloxacin and ciprofloxacin. After the patient had completed a course of antibiotics, repeat urine MCS was done and found to be normal.
The patient subsequently had open cystolithotomy, pyelolithotomy, and an excision of the middle lobe of the prostate with diathermy. Findings at surgery included a thickened bladder wall, a vesical stone measuring 8 cm × 4 cm × 3 cm and a prominent median lobe of the prostate. Patient recovered well postoperatively and was discharged home to continue follow-up at the outpatient clinic.
| Discussion | |  |
Calculi vary considerably in size and may stay in the position in which they are formed or migrate down the urinary tract producing the symptoms along the way.[4]
Prostate enlargement predisposes men to urinary stasis which creates a favorable environment for stone formation and urinary tract infection. This was demonstrated in this patient. Other predisposing factors to development of bladder stones include spinal cord injury,[5] paralysis, kidney stone, bladder inflammation secondary to external beam radiation, or schistosomiasis, congenital or acquired vesical diverticula, intravesical foreign bodies, sliding inguinal hernias containing the urinary bladder.[6]
Imaging features of urolithiasis vary depending on the stone composition and imaging modalities utilized. In resource-limited settings, plain radiography of the abdomen will be thefirst in a line of imaging in suspected cases of urolithiasis. This is targeted at viewing the location of the KUB for the possible presence of urinary stones. About 75% of stones are of calcium and so will be radio-opaque. Pure uric acid and ammonium urate stones are radiolucent but may be coated with a layer of opaque calcium sediment. Laminations are common, with the layers stratified according to metabolic and infectious status and the degree of periodic hematuria.[7] On plain radiographs, the bladder stones are seen as well delineated radio-opaque structures within the pelvis and may vary in number, size, and shape. The above patient had a solitary stone in the urinary bladder.
Ultrasound scanning identifies the calculi and detects obstruction. Sonograms are effective in identifying both radiolucent and radio-opaque stone and typically shows a classic hyperechoic object with posterior shadowing,[8] mobility can also be demonstrated. They may be associated with the bladder wall thickening due to the inflammation. In this patient, ultrasound was useful in assessing the prostate gland and complications that were associated with his condition in addition to identify the presence and location of the calculi.
After contrast administration on IVU, the radiolucent stone appears as a filling defect in the urinary bladder while the radio-opaque stone will be obscured. IVU may also be used to identify the associated abnormalities such as upper urinary tract calculi, ureterocele, cystocele, enlarged prostate and bladder diverticula [7] in the index patient the coexisting hydronephrotic changes in the right renal collecting system as a result of the upper urinary tract calculi was demonstrated on IVU.
Nonenhanced computed tomography (NECT) scanning is now the imaging modality of choice and has replaced IVU [9] especially in the western world. Unenhanced CT scanning is highly sensitive and specific in diagnosing calculi along the urinary tract. Even pure urate calculi can be detected with this method.[9] However, it may not be possible to have NECT done due to nonavailability of the machine and high costs for patients in resource-limited settings.
Cystoscopy allows the examiner to visualize the stones and assess their number, size, and position. Additionally, examination of the urethra, prostate, bladder wall, and ureteral orifices allows the identification of strictures, prostatic obstruction, bladder diverticula, and bladder tumors.[9]
A bladder stone is in itself a sign of an underlying problem, hence, inorder to prevent a recurrence, removal of the stone and treatment of the underlying abnormality are nearly always indicated. In addition to removal of the urinary tract calculi, the patient had an excision of the enlarged median lobe of the prostate in order to relieve the obstructive uropathy which is a major risk factor for calculi formation that was identified in him.
| Conclusion | |  |
LUTS with resultant urinary stasis and predisposition to the stone formation are common among the middle aged and elderly men in our environment and this article highlights the role of basic radiological imaging in the clinical evaluation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Bernier F. Management of clients with urinary disorders. In Black J, Hawks J, editors. Medical- surgical nursing: Clinical management for positive outcomes. 7 th ed. St. Louis: Elsevier 2005.p. 857-911.  |
| 2. | Kim HH, Jo MK, Kwak C, Park SK, Yoo KY, Kang D, et al. Prevalence and epidemiologic characteristics of urolithiasis in Seoul, Korea. Urology 2002;59:517-21.  |
| 3. | Lee YH, Huang WC, Tsai JY, Lu CM, Chen WC, Lee MH, et al. Epidemiological studies on the prevalence of upper urinary calculi in Taiwan. Urol Int 2002;68:172-7.  |
| 4. | Parmar MS. Kidney stones. J Urol 2004;328:1420-4.  |
| 5. | Kawu AA, Olawepo A, Salami O, Kuranga SA, Shamsi H, Jeje EA. Bladder stones in catheterized spinal cord-injured patients in Nigeria. Niger J Clin Pract 2012;15:156-8.  [ PUBMED]  |
| 6. | Ng AC, Leung AK, Robson WL. Urinary bladder calculi in a sliding vesical-inguinal-scrotal hernia diagnosed preoperatively by plain abdominal radiography. Adv Ther 2007;24:1016-9.  |
| 7. | Wein A, Kavoussi L, Novick A, Partin A, Peters C. Lower urinary tract calculi. Campbell-Walsh Urology. 9 th ed. Philadelphia, Pa: Saunders Elsevier; 2007. p. 2663-73.  |
| 8. | Huang WC, Yang JM. Sonographic appearance of a bladder calculus secondary to a suture from a bladder neck suspension. J Ultrasound Med 2002;21:1303-5.  |
| 9. | Kambadakone AR, Eisner BH, Catalano OA, Sahani DV. New and evolving concepts in the imaging and management of urolithiasis: Urologists' perspective. Radiographics 2010;30:603-23.  |
[Figure 1], [Figure 2], [Figure 3]
|