|
 
 |
| CASE REPORT |
|
| Year : 2013 | Volume
: 1
| Issue : 3 | Page : 107-112 |
|
Periodontics and orthodontics team-work in the treatment of gingival recession: Two case reports
Arzu Alkan1, Omer Cakmak2, Ilhan Ramoglu3, Gulsah Yagan4, Banu KiliÁ5
1 Erciyes University, Faculty of Dentistry, Department of Periodontology, Kayseri, Turkey
2 Kocatepe University, Faculty of Dentistry, Department of Periodontology, Afyon, Turkey
3 Bezmi Alem Vakif University, Faculty of Dentistry, Department of Orthodontics, Istanbul, Turkey
4 Faculty of Dentistry, Department of Orthodontics, Kayseri, Turkey
5 Orthodontist, Private Practice, Kayseri, Turkey
| Date of Web Publication | 20-Dec-2013 |
Correspondence Address:
Arzu Alkan
Department of Periodontology, Faculty of Dentistry, Erciyes University, 38039, Melikgazi, Kayseri
Turkey
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-3825.123322

In this report, we presented two cases in which orthodontic treatment played the role both in the etiology and treatment of gingival recession at mandibular anterior teeth. Subepithelial connective tissue graft was used in order to cover the exposed root surfaces. Residual recession after mucogingival periodontal surgery was further reduced by orthodontic intrusion of the incisors in both of the cases. The periodontics and orthodontics team-work satisfied both patients and the clinicians from the point of maintaining periodontal health, ideal occlusal relationships and masticatory function despite the prolonged treatment period. Keywords: Orthodontics, periodontics, root coverage, subepithelial connective tissue graft
How to cite this article:
Alkan A, Cakmak O, Ramoglu I, Yagan G, KiliÁ B. Periodontics and orthodontics team-work in the treatment of gingival recession: Two case reports. J Orthod Res 2013;1:107-12 |
How to cite this URL:
Alkan A, Cakmak O, Ramoglu I, Yagan G, KiliÁ B. Periodontics and orthodontics team-work in the treatment of gingival recession: Two case reports. J Orthod Res [serial online] 2013 [cited 2017 Mar 7];1:107-12. Available from: http://www.jorthodr.org/text.asp?2013/1/3/107/123322 |
| Introduction | |  |
Gingival recession occurs due to several factors including mechanical trauma, periodontal disease, traumatic bad habits, faulty restorations, abnormal tooth positioning outside the labial alveolar plate resulting in bone dehiscence or fenestration, uncontrolled orthodontic tooth movement and high muscle attachments. [1]
Pedicle soft-tissue grafts (double-papillae and coronally and laterally positioned flaps), free gingival and subepithelial connective tissue grafts (SCTG), guided tissue regeneration and acellular dermal matrix allografts combined with coronally positioned flaps are the main surgical techniques that have been used to obtain the root coverage. [2] The SCTG has proven to be a gold standard among these procedures with highly predictable outcome and excellent final color match. [3],[4]
Interdisciplinary treatment approach is imperative for some of the challenging and complex dental situations in order to improve esthetics and prognosis. In some particular cases, one of the treatment disciplines acts as a complementary phase in solving the problem in a more ideal situation. Treatment of gingival recession may serve as an example in this sense. In other words, while an orthodontic therapy may improve the outcome of a root coverage procedure, a mucogingival surgery may serve to eliminate a gingival recession defect resulting from an orthodontic therapy. When the literature regarding this issue was reviewed, it was observed that reports were mainly focused on the establishment of maxillary anterior esthetics. [5],[6]
An interdisciplinary treatment approach for the predictable treatment of two patients with gingival recession was presented in this paper. One case was referred by a general dental practitioner and the other by a private practice orthodontist to the Department of Periodontology, Faculty of Dentistry, Erciyes University.
| Case Reports | |  |
Case 1
A 33-year-old female who had a chief complaint of recurrent gingival abscess in the region of right and left mandibular central incisors was initially seen at the clinic of a general dental practitioner and the extraction of the teeth was planned. However, the patient applied to our clinic and indicated that she wanted to save the teeth, if possible. Patient was in good health and her medical history was unremarkable. She was a non-smoker. Clinical examination revealed a Miller Class 3 [7] gingival recession at teeth #41 and 42 [Figure 1]. Baseline clinical measurements including bleeding on probing, probing depth, recession depth and width of keratinized tissue are listed in [Table 1].
The initial treatment included scaling and root planning (SRP) and many oral hygiene instruction (OHI) sessions. However, gingival inflammation persisted especially at mid-buccal gingiva [Figure 2]. A SCTG was planned to cover the exposed root surfaces and increase the width and thickness of keratinized gingiva. Before surgery, segmental orthodontic treatment was initiated to align and retrude the mandibular anterior teeth in order to increase the success of the surgical procedure and improve prognosis and esthetical outcome. Upon the elimination of rotations and minimizing diastemas at 7 months orthodontic therapy, it was observed that the recession at tooth #42 progressed from 3 to 5 mm [Figure 3]. A SCTG with coronally advanced flap was performed at this stage of the treatment. Briefly, under local anesthesia, a split thickness flap was raised on labial aspect of teeth #41 and 42 with vertical incisions. Following root planning, a SCTG harvested from the palate was placed over the exposed root surfaces and a coronally positioned flap was secured with 4.0 silk sutures (Dogsan Medical Equipment Industry, Trabzon/Turkey). The post-operative period was problem free, but clinical examination performed at 6 months after surgery revealed a residual recession of 2.5 mm [Figure 4] and premature contact at tooth #41 in anterior guidance. Orthodontic treatment was reinitiated in order to intrude both first incisors for further root coverage and elimination of premature contact. Light intrusive forces of 10-12 g were applied for 8 months until the leveling of incisal edges of the incisors were achieved. At the end of orthodontic treatment, almost complete root coverage was obtained [Figure 5]. A total of 33 months clinical measurements are listed in [Table 2]. | Figure 2: Clinical view after initial periodontal therapy (scaling and root planning + oral hygiene instruction)
Click here to view |
 | Figure 3: Seven months at segmental orthodontic treatment before subepithelial connnective tissue grafting. Note the increase in the amount of recession at tooth 42
Click here to view |
 | Figure 4: A residual recession of 2.5 mm after 6 months following surgery
Click here to view |
Case 2
A 24-year-old systemically healthy female was referred to our clinic by her Orthodontist. She had been on fixed orthodontic therapy for 18 months for canine distalization and the next step of the treatment was leveling of the lower incisors. On clinical examination, tooth #41 presented a Miller Class 2 [7] gingival recession with a strong mucogingival stress [Figure 6]. Patient experienced pain in this region during brushing her teeth. Baseline clinical measurements are listed in [Table 1]. | Figure 6: A Miller Class 2 gingival recession at tooth #41. Note the absence of mid-buccal keratinized tissue. Prior to anterior bracket placement after canine distalization
Click here to view |
Patient's orthodontist informed the clinicians that canine distalization was completed and 0.16 × 0.16 CuNiti was placed for the correction of mandibular canine rotations. Following initial periodontal treatment (OHI + SRP), a SCTG harvested from the palate was placed into the tunnel-like recipient bed extending to the adjacent teeth to cover the exposed root surface [Figure 7] and [Figure 8] and secured with sling sutures (4.0 silk [Dogsan Medical Equipment Industry, Trabzon/Turkey]). Interproximal sutures were also used since the papillae lacerated during the placement of the graft into the tunnel due to the thin biotype of the gingiva. 3 weeks after surgery, vestibular region of tooth #41 was deepened by a split thickness dissection of alveolar mucosa in order to eliminate the re-established mucogingival stress and the resultant mobility in the gingival margin [Figure 9]. Nine months after, SCTG surgery and leveling of the incisors, a keratinized tissue of 2 mm and partial root coverage of 1 mm was gained [Figure 10]. Orthodontic intrusion of the incisor was initiated at 9 months after surgery in order to obtain further root coverage. At the end of orthodontic treatment, a residual recession of 1 mm existed [Figure 11].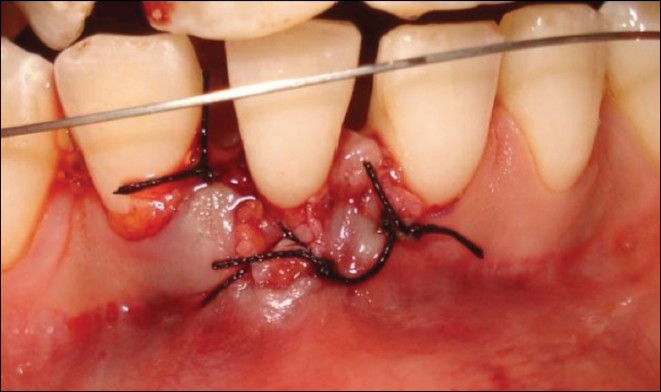 | Figure 8: Subepithelial connective tissue graft secured with sling and interproximal sutures
Click here to view |
 | Figure 10: Partial root coverage obtained at 9 months following mucogingival surgery
Click here to view |
 | Figure 11: Completion of the orthodontic therapy. Note the minor amount of gingival recession
Click here to view |
| Discussion | |  |
Gingival recession regardless of etiology is a debilitating situation for the individual, which may cause dentinal hypersensitivity, root caries, dental abrasion, unsatisfactory esthetics and ineffective tooth brushing. The two cases presented in this paper are examples for such gingival recession defects in which orthodontic therapy played the role both in its etiology and treatment.
High success rate in the previous studies [4] and achievement of both goals, i.e., root coverage and creation of keratinized gingival tissue [8] with one surgical procedure were the reasons for choosing SCTG in the present cases.
Orthodontic therapy may have a dual effect on the morphology of the bone and gingiva with respect to the final position of the teeth. While severe labial inclination causes gingival recession and bone dehiscences, [9],[10] retraction of anterior teeth stops or even reverses the progressive recession process. [11],[12],[13],[14],[15]
In Case 1, during orthodontic alignment and retrusion of the incisors, an increase in recession depth was noted at tooth #42. This could be explained by the further resorption of the thin facial bone plate covered by the gingiva with thin biotype that served as a locus minorus resistentia. [16] This finding is also in agreement with the findings of Melsen and Allais who suggested that the presence of baseline recession and a thin gingival biotype may be possible predictors of recession following orthodontic therapy. [17] SCTG without orthodontics could have been attempted in the treatment of Case 1 but the Periodontist and Orthodontist established a consensus regarding segmental orthodontic treatment as they thought it would increase the success of the surgical procedure and improve the long term prognosis. Zucchelli et al. successfully treated a patient similar to Case 1 by SCTG performed after fixed orthodontic treatment resulting in a resolution of root malposition. [18] Free gingival graft might have been an alternative surgical technique but, graft survival over the avascular root surfaces of two adjacent teeth could have been jeopardized and color match of the graft with the surrounding tissues would not be achieved.
Our treatment approach in Case 2 was to perform mucogingival surgery before proceeding with the next steps of the orthodontic therapy in order to eliminate the mucogingival stress at the gingival margin of tooth #41 and to create a thick band of keratinized tissue at the labial aspect of the tooth. The newly formed keratinized tissue after SCTG, was surprisingly thin, but it responded favorably to intrusive forces corroborating with the study of Re et al. [19] which showed predictable reduction in recession in periodontally compromised patients following intrusive orthodontic therapy regardless of the gingival biotype. A recession reduction of 1 mm in Case 1 and Case 2 was achieved by intrusing the teeth 2 mm in both of the cases. These findings confirmed those of a study, [20] which also demonstrated that buccal gingiva seemed to be capable of following the vertical tooth displacement by 50%.
Investigators claimed that intrusion could be a reliable therapeutic approach [21] in terms of improving the quantity of new attachment [22] in patients with healthy periodontal tissues because it does not result in a decrease of marginal bone level, provided that gingival inflammation is controlled [23] and is performed with light forces (5-15 g/tooth). [24] In Case 1 and 2, residual recession defects after SCTG were further treated by an unplanned orthodontic intrusion for the achievement of maximum root coverage. The final outcome, while not excellent, was quite acceptable in both cases. Similarly, Re et al. evaluated the role of orthodontic intrusion and alignment in the reduction of gingival recession around maxillary incisors of adult periodontal patients and reported a predictable reduction of recession in the presence of both thin and thick gingiva. [19]
A controversy exists on the timing of mucogingival surgery in cases of preorthodontic gingival recession. [25] Some authors claim that mucogingival surgery should be performed before orthodontic therapy, particularly in patients presenting less than 2 mm width of keratinized tissue combined with thin-scalloped gingival biotype to prevent recession. [9],[26] Since, a thicker marginal gingiva is expected to be less susceptible to tooth brushing trauma and biofilm-induced gingival inflammation that may cause labial recession or increase its severity. [25] On the other hand, the other investigators prefer to postpone root coverage surgery due to reason that the orthodontic movement of the tooth back into its alveolus may cover the exposed root surface in some cases. [14],[27] In 30 years follow-up case by Pini-Prato et al., [28] the coverage of gingival recession was achieved by orthodontic tooth repositioning that resulted in reestablishment of soft tissues surrounding incisors without any mucogingival surgery. As the incisors would be aligned and leveled and would not be retruded in Case 2, this treatment option did not apply to this patient. In this context, a SCTG before the initiation of the orthodontic treatment could have been a preventive measure in this case since the authors claim that the increased thickness of the keratinized gingiva is important in recession development rather than tooth inclination. [29]
| Conclusion | |  |
Orthodontic treatment may play a role both in the etiology and treatment of gingival recession in such cases, a periodontics and orthodontics team-work may be required in which one acts as a complementary phase for the other. The final outcome frequently satisfies both patients and the clinicians from the point of maintaining periodontal health, esthetics, occlusal relationships and long-term prognosis despite the longer time needed for completion of the treatment.
| References | |  |
| 1. | Agudio G, Pini Prato G, Cortellini P, Parma S. Gingival lesions caused by improper oral hygiene measures. Int J Periodontics Restorative Dent 1987;7:52-65. 
[PUBMED] |
| 2. | Harris RJ. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: Results of 107 recession defects in 50 consecutively treated patients. Int J Periodontics Restorative Dent 2000;20:51-9. 
[PUBMED] |
| 3. | Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal plastic surgery for treatment of localized gingival recessions: A systematic review. J Clin Periodontol 2002;29 Suppl 3:178-94. 
[PUBMED] |
| 4. | Chambrone L, Pannuti CM, Tu YK, Chambrone LA. Evidence-based periodontal plastic surgery. II. An individual data meta-analysis for evaluating factors in achieving complete root coverage. J Periodontol 2012;83:477-90. 
|
| 5. | Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc 2006;137:160-9. 
[PUBMED] |
| 6. | Maurer S, Leone CW. Use of a serially layered, double connective tissue graft approach to enhance maxillary anterior esthetics. Int J Periodontics Restorative Dent 2001;21:497-503. 
[PUBMED] |
| 7. | Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent 1985;5:8-13. 
|
| 8. | Wennström JL, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2-year prospective clinical study. J Clin Periodontol 1996;23:770-7. 
|
| 9. | Dorfman HS. Mucogingival changes resulting from mandibular incisor tooth movement. Am J Orthod 1978;74:286-97. 
[PUBMED] |
| 10. | Wennström JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol 1987;14:121-9. 
|
| 11. | Parfitt GJ, Mjor IA. A clinical evaluation of local gingival recession in children. J Dent Child 1964;31:257-62. 
|
| 12. | Engelking G, Zachrisson BU. Effects of incisor repositioning on monkey periodontium after expansion through the cortical plate. Am J Orthod 1982;82:23-32. 
[PUBMED] |
| 13. | Karring T, Nyman S, Thilander B, Magnusson I. Bone regeneration in orthodontically produced alveolar bone dehiscences. J Periodontal Res 1982;17:309-15. 
[PUBMED] |
| 14. | Ngan PW, Burch JG, Wei SH. Grafted and ungrafted labial gingival recession in pediatric orthodontic patients: Effects of retraction and inflammation. Quintessence Int 1991;22:103-11. 
[PUBMED] |
| 15. | Wennström JL. Mucogingival considerations in orthodontic treatment. Semin Orthod 1996;2:46-54. 
|
| 16. | Khurana P, Soni VP. Orthodontic intervention to resolve periodontal defects: An interdisciplinary approach. J Indian Soc Periodontol 2010;14:287-9. 
[PUBMED]  |
| 17. | Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: A retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop 2005;127:552-61. 
[PUBMED] |
| 18. | Zucchelli G, Parenti SI, Ghigi G, Bonetti GA. Combined orthodontic - mucogingival treatment of a deep post-orthodontic gingival recession. Eur J Esthet Dent 2012;7:266-80. 
[PUBMED] |
| 19. | Re S, Cardaropoli D, Abundo R, Corrente G. Reduction of gingival recession following orthodontic intrusion in periodontally compromised patients. Orthod Craniofac Res 2004;7:35-9. 
[PUBMED] |
| 20. | Murakami T, Yokota S, Takahama Y. Periodontal changes after experimentally induced intrusion of the upper incisors in Macaca fuscata monkeys. Am J Orthod Dentofacial Orthop 1989;95:115-26. 
[PUBMED] |
| 21. | Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent 2000;20:31-9. 
[PUBMED] |
| 22. | Melsen B, Agerbaek N, Eriksen J, Terp S. New attachment through periodontal treatment and orthodontic intrusion. Am J Orthod Dentofacial Orthop 1988;94:104-16. 
[PUBMED] |
| 23. | Melsen B. Tissue reaction following application of extrusive and intrusive forces to teeth in adult monkeys. Am J Orthod 1986;89:469-75. 
[PUBMED] |
| 24. | Melsen B, Agerbaek N, Markenstam G. Intrusion of incisors in adult patients with marginal bone loss. Am J Orthod Dentofacial Orthop 1989;96:232-41. 
[PUBMED] |
| 25. | Tanaka OM, Avila AL, Silva GM, Añez MC, Taffarel IP. The effects of orthodontic movement on a subepithelial connective tissue graft in the treatment of gingival recession. J Contemp Dent Pract 2010;11:E073-9. 
|
| 26. | Mathews DP, Kokich VG. Managing treatment for the orthodontic patient with periodontal problems. Semin Orthod 1997;3:21-38. 
[PUBMED] |
| 27. | Yared KF, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop 2006;130:6.e1-8. 
|
| 28. | Pini-Prato GP, Cozzani G, Magnani C, Baccetti T. Healing of gingival recession following orthodontic treatment: A 30-year case report. Int J Periodontics Restorative Dent 2012;32:23-7. 
[PUBMED] |
| 29. | Busschop JL, Van Vlierberghe M, De Boever J, Dermaut L. The width of the attached gingiva during orthodontic treatment: A clinical study in human patients. Am J Orthod 1985;87:224-9. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10], [Figure 11]
[Table 1], [Table 2]
|