|


 |
| REVIEW ARTICLE |
|
| Year : 2011 | Volume
: 3
| Issue : 2 | Page : 68-75 |
|
|
Surgical management of hemorrhoids
SP Agbo
Department of Surgery, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
| Date of Web Publication | 11-Feb-2012 |
Correspondence Address:
S P Agbo
Department of Surgery, Usmanu Danfodiyo University Teaching Hospital, Sokoto
Nigeria
 Source of Support: None, Conflict of Interest: None  | 3 |
DOI: 10.4103/2006-8808.92797

 Abstract Abstract | | |
Hemorrhoids are common human afflictions known since the dawn of history. Surgical management of this condition has made tremendous progress from complex ligation and excision procedures in the past to simpler techniques that allow the patient to return to normal life within a short period. Newer techniques try to improve on the post-operative complications of older ones. The surgical options for the management of hemorrhoids today are many. Capturing all in a single article may be difficult if not impossible. The aim of this study therefore is to present in a concise form some of the common surgical options in current literature, highlighting some important post operative complications. Current literature is searched using MEDLINE, EMBASE and the Cochrane library. The conclusion is that even though there are many surgical options in the management of hemorrhoids today, most employ the ligature and excision technique with newer ones having reduced post operative pain and bleeding. Keywords: Hemorrhoids, hemorrhoidectomy, surgical
How to cite this article:
Agbo S P. Surgical management of hemorrhoids. J Surg Tech Case Report 2011;3:68-75 |
 Introduction Introduction | |  |
Hemorrhoids are common clinical conditions. About half of the population has hemorrhoids by the age of 50 years. It is estimated that 58% of people aged over 40 years have the disease in the USA. [1] Almost one third of these patients present to surgeons for treatment. [1] Hemorrhoids can occur at any age, and they affect both men and women. Exact incidence in developing countries is unknown, but the disease is being more frequently encountered, perhaps due to westernized life style. Report of first recorded treatment for hemorrhoids comes from the Egyptian papyrus dated 1700 bc: "… Thou shouldest give a recipe, an ointment of great protection; Acacia leaves, ground, titurated and cooked together. Smear a strip of fine linen there -with and place in the anus, that he recovers immediately. [2]
Hippocrates in 460 bc wrote of hemorrhoids treatment similar to today's rubber band ligation procedure thus: "And hemorrhoids in like manner you may treat by transfixing them with a needle and tying them with very thick and woolen thread, for application, and do not forment until they drop off, and always leave one behind; and when the patient recovers, let him be put on a course of Hellebore." [2]
A Roman physician named Celcus (25 bc - ad 14) described the ligation and excision surgeries, as well as possible complications. Galen (ad 13I - 201) also promoted the use of severing the connection of the arteries to veins in order to reduce pain and avoid spreading gangrene.
The Indian Susruta Samhita, an ancient Sanskrit text dated between the fourth and fifth century ad, described treatment procedures comparable to those in the Hippocratic treatise, but with advancement in surgical procedures and emphasis on wound cleanliness. [2]
By the 13 th century, there was great progress in the surgical procedure, led by European Master Surgeons,' notable among whom were Lanfrank, of Milan; and Guy de Chauliac, Henri de Mondeville and John, of Ardene.
During the 19 th century, another mode of treatment for hemorrhoids, called anal stretching or rectal bouginage, became popular. In the USA, Mitchell (of Illinois) first used carbolic acid for injecting hemorrhoids, in 1871. In 1888, Fredrick Salmon, the founder of St. Marks' Hospital, expanded the surgical procedure for hemorrhoids into a combination of excision and ligation, where the peri-anal skin is incised, the hemorrhoidal plexus and the muscles are dissected, and the hemorrhoid is ligated. [2],[3] Today's Ferguson and Milligan-Morgan procedures are considered a modification of the Salmon's techniques. The diathermy hemorrhoidectomy by Alexander Williams, rubber band ligation by Barron, and the stapled hemorrhoidectomy by Longo were three additional developments in the late 20 th century.
 Etiology Etiology | |  |
Hemorrhoids are cushion sinusoids thought to function as part of the continence mechanism and aid in complete closure of the anal canal at rest. [4] The main cushions lie at the left lateral, right anterior and right postero-lateral portions of the anal canal. Secondary cushions may be present. Bleeding and thrombosis of the pre-sinusoidal arterioles may occur in association with prolapse. Proposed etiological factors include constipation, prolonged straining, pregnancy, obesity, ageing, hereditary, derangement of the internal anal sphincter, weak blood vessels and absent valves in the portal vein. The erect posture of humans is also a predisposing factor. Despite several studies, the pathogenesis of hemorrhoids still remains unclear. [5]
 Classification Classification | |  |
Hemorrhoids can either be external or internal [Figure 1]. The external variety is covered by skin below the dentate line, while the internal variety lies proximal to the dentate line. Combination of the two varieties constitutes interoexternal hemorrhoids. Internal hemorrhoids are further classified into the following grades:
Grade I - Hemorrhoids bleed and may protrude into, but do not prolapse out of, the anal canal.
Grade II - Hemorrhoids prolapse on defecation but reduce spontaneously.
Grade III - Hemorrhoids require manual reduction.
Grade IV - Hemorrhoids cannot be reduced. They are permanently prolapsed [Figure 2].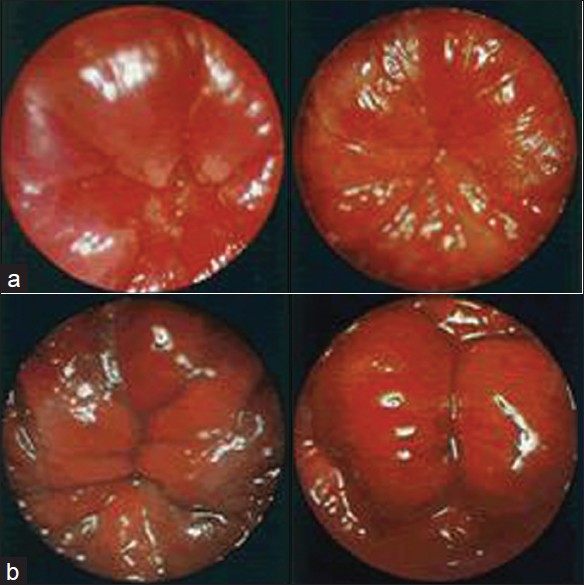 | Figure 2: (a) Proctoscopic grades I and II; (b) Proctoscopic grades III and IV
Click here to view |
There is no similar classification for external hemorrhoids; they are considered to be swellings of the skin and endoderm around the anus.
 Symptoms Symptoms | |  |
The main complaints are bleeding during or after defecation, pain, prolapse, itching and peri-anal soiling. Diagnosis is made by examining the anus and anal canal, and it is important to exclude more serious causes of bleeding, like rectal cancer.
 Differential Diagnosis Differential Diagnosis | |  |
Differential diagnosis of hemorrhoids includes anal skin tags, fibrous anal polyp, peri-anal hematoma, rectal prolapse, anal fissure, dermatitis and rectal tumor.
 Treatment Treatment | |  |
Prevention is the best treatment for hemorrhoids. The disease once established tends to get worse over time. [5]
Medical application of creams and suppositories can relieve irritation and pain but rarely provide long-term benefit. [5] A high-fiber diet and bulk laxatives prevent constipation and worsening of the disease without achieving a cure. The mainstay of treatment therefore is surgical. But unfortunately, operative hemorrhoidectomy is usually associated with significant postoperative complications, including pain, bleeding and anal stricture, which can result in protracted period of convalescence. [6] This has therefore stimulated continuing efforts to develop new techniques with less painful course and faster recovery. Recent advances in instrumental technology have led to the development of the bipolar electro-thermal devices - ultrasonic scalpel, circular stapler and the ligasure vessel-sealing systems. It is now possible to vaporize' hemorrhoids, with the advent of the atomizer wand. Some of the surgical options for treating hemorrhoids include the following:
Nonoperative (conservative) options: Rubber band ligation, sclerotherapy, infrared photocoagulation, cryotherapy, manual anal dilatation, LASER hemorrhoidectomy, the harmonic ultrasonic scalpel hemorrhoidectomy, Doppler-guided hemorrhoidal artery ligation, and the new atomizing technique that uses the atomizer wand to excise and vaporize hemorrhoids.
Most nonoperative procedures are reserved for first- and second-degree hemorrhoids and are usually carried out on outpatient basis.
Operative options: The clamp and cautery hemorrhoidectomy, open hemorrhoidectomy, closed hemorrhoidectomy, submucosal hemorrhoidectomy, whitehead circumferential hemorrhoidectomy, stapled hemorrhoidectomy, radiofrequency ablation and suture fixation hemorrhoidectomy, pile suture' method, the bipolar diathermy hemorrhoidectomy, and the ligasure hemorrhoidectomy. Operative hemorrhoidectomies are reserved mainly for third- and fourth-degree hemorrhoids.
Nonoperative procedures
Rubber band ligation
Bleeding from first-, second- and some selected third-degree hemorrhoids can be treated by rubber band ligation. By this method, mucosa 1-2 cm above the dentate line is grasped and pulled into a rubber band applier (the Barron gun). After firing the gun, the rubber strangulates the underlying tissue causing scarring and preventing further bleeding and prolapse. Generally, only one or two quadrants are banded per visit. No anesthesia is required. Results are superior to those of injection sclerotherapy. [6]
A recent meta-analysis of hemorrhoidal treatment concluded that rubber band ligation was the initial mode of therapy for first- to third-degree hemorrhoids. [7]
Injection sclerotherapy (Mitchell technique)
Mitchell (of Illinois, USA) first used carbolic acid for injecting hemorrhoids in 1871. [8] The method offers effective day care treatment for first-, second- and some third-degree hemorrhoids. A quantity of 1-3 mL of a sclerosing agent (5% phenol in almond or Arachis oil, sodium morrhuate or quinine urea) is injected into the submucosa of each hemorrhoid. The objective is to cause thrombosis of the vessels and promote fibrosis, which retracts the prolapse. Where possible, the Gabriel's syringe should be used. It is specially adapted to pass through the proctoscope. Disposable syringes have however now replaced the Gabriel's syringe. Not more than 3 injections at 6-week intervals should be given in one phase of treatment. [8] A course of several injections may be required. Complications are few, though infection and fibrosis have been reported.
Infrared photocoagulation
Infrared photocoagulation is an effective outpatient treatment for first- and second-degree hemorrhoids. [9] The infrared probe is applied to the base of the hemorrhoids through a proctoscope to produce a circular burn 2 mm deep. Exposure is for 1 second at each site. Results are similar to those of banding and sclerotherapy, but the procedure is less painful. [10] Repeated therapy has however been found to be necessary for photocoagulation. [10] It is an expensive procedure.
Cryosurgery
This procedure is indicated for first-, second- and some selected third-degree hemorrhoids.
The cryoprobe of liquid nitrogen is applied to the hemorrhoid for about 3 minutes to produce liquefaction of frozen tissue, over the ensuing 2-3 weeks. [11] This procedure is painless and requires no anesthesia, but edema and profuse discharge are a problem in this procedure. O'Callaghan et al. in 1982 concluded in their studies that cryosurgery gave results similar to those of open hemorrhoidectomy in patients with prolapsing hemorrhoids, but there were fewer complications and shorter hospital stay with cryosurgery. [12]
Manual anal dilatation (Lord's procedure)
This procedure indicated mostly for second- and third-degree hemorrhoids was advocated by Lord in 1969. It aims to dilate the anal sphincter to accept 4 fingers of each hand and to maintain sphincter laxity by regular use of a dilator. [13] General anesthesia is required, but the patient can go home the same day. It is now largely abandoned due to the frequently occurring complication of incontinence, especially when combined with open hemorrhoidectomy. [14],[15]
LASER hemorrhoidectomy
The hemorrhoid is vaporized or excised using carbon dioxide or NdYag LASER. [16] The smaller LASER beam allows for precision and accuracy; and, usually, rapid, unimpaired healing. It is painless. LASER therapy may be used alone or in combination with other modalities. In a study of 750 patients undergoing LASER treatment for hemorrhoids, 98% successful result was reported. Patient satisfaction was 99%. [17] It is an outpatient procedure reserved mostly for first-, second- and some third-degree hemorrhoids.
The harmonic ultrasonic scalpel hemorrhoidectomy
The harmonic scalpel uses ultrasonic energy, which allows for both cutting and coagulation of hemorrhoidal tissue at precise points of application, resulting in minimal lateral thermal damage. [18] It uses temperatures lower than those of electro-surgery or LASERs. [18] Coaptive coagulation of bleeding vessels is achieved at temperatures between 50°C and 100°C compared to the obliterative coagulation (burning) by electrocautery at 150°C. The vibrating blade at 55, 500 Hz couples with protein and denatures it to form a coagulum that seals bleeding vessels. It is an outpatient procedure reserved for first- and second-degree hemorrhoids. It however has longer operating time and more pain when compared to the ligasure hemorrhoidectomy. [19]
Atomizing hemorrhoids
The atomizer wand is an innovative wave form of electrical current wherein a specialized electrical probe excises or vaporizes one or more cell layers at a time, reducing the hemorrhoids to minute particles of fine mist or spray, which are immediately vacuumed away. [20] The hemorrhoids are essentially disintegrated into an aerosol of carbon and water molecules. Results are similar to those of LASER hemorrhoidectomy except that there is less bleeding using the atomizer and that the atomizer costs less. [20] The procedure is suitable for hemorrhoids of grades I, II and III. Patient does not require hospital stay. Presently, atomizing hemorrhoids is offered exclusively in Arizona, USA. [20]
Doppler-guided hemorrhoidal artery ligation
This is also a new technique first described by the Japanese surgeon Kazumasa Morinaga in 1995, who identified the hemorrhoidal arteries by means of a Doppler (ultrasound) technique. [21] The specially designed proctoscope contained a Doppler transducer and a window through which the surgeon can identify and ligate the hemorrhoidal arteries by placing a suture around them. [22] All the hemorrhoidal arteries are ligated in this procedure. It is a day care procedure suitable for first-, second- and some selected third-degree hemorrhoids, and the patient goes home after sedation wears off. There is little or no bleeding postoperatively. George et al. concluded in their study that the procedure is a safe and effective alternative to hemorrhoidectomy. [22] Pure external hemorrhoids would not respond to this procedure.
Operative procedures
Bowel preparation before operation minimizes fecal contamination and keeps the colon quiet for the first few days of the operative period.
Clamp and cautery hemorrhoidectomy
This method is now obsolete but has the advantage in not having any form of dissection of tissue planes. The hemorrhoid is grasped in-between the insulated blades of Smith's pile clamp. The greater part of the hemorrhoid mass is then cut away with scissors, leaving only a stump, which is burned with heated copper cautery to arrest bleeding. [23] The copper cautery is usually heated over a gas ring, which is seldom available in a modern operation theatre today. The electric cautery or diathermy knives are unsatisfactory substitutes because they are ineffective in arresting hemorrhage and because the coagulating current may penetrate tissues too deeply. The operation is reserved for second- to fourth-degree hemorrhoids and it is done under general anesthesia.
Open hemorrhoidectomy (Milligan-Morgan method)
This is the most commonly used technique and is widely considered to be the most effective surgical technique for treating hemorrhoids. [24] We routinely carry out open hemorrhoidectomy at our center. Adotey and Jebbin in PortHarcourt, Nigeria, showed that open hemorrhoidectomy was the predominant surgical method for treating hemorrhoids. [25] Uba et al. in Jos, Nigeria, also concluded in their studies that open hemorrhoidectomy was safe, simple and cost-effective, with postoperative pain, acute urine retention and bleeding being the commonest complications. [26],[27]
It is the procedure of choice for third- and fourth-degree hemorrhoids [Figure 3].
This method was developed in the United Kingdom by Drs. Milligan and Morgan in 1937, mainly for hemorrhoids of grades II-IV. [28] A V-shaped incision by the scalpel in the skin around the base of the hemorrhoid is followed by scissors dissection in the submucous space to strip the entire hemorrhoid from its bed. The dissection is carried cranially to the pedicle, which is ligated with strong catgut and the distal part excised [Figure 4]. Other hemorrhoids are similarly treated, leaving a skin bridge in-between to avoid stenosis. The wound is left open and a hemostatic gauze pad left in the anal canal [Figure 5]. The procedure is done under general or epidural anesthesia. Postoperative pain and acute urine retention are common complications.
Closed hemorrhoidectomy (Ferguson's technique)
Developed in the United States by Drs. Ferguson and Heaton in 1952, this is a modification of Milligan-Morgan method described above. [29] The indications for this procedure are similar to those of Milligan-Morgan procedure. Here the incisions are totally or partially closed with absorbable running suture, following surgical excision of the hemorrhoids [Figure 6]. The Ferguson method has no advantage in terms of wound healing because of the high rate of suture breakage at bowel movement. [29] There are several modifications of this method.
Submucosal hemorrhoidectomy (Parks procedure)
This procedure was developed in the 1950s by Parks, who published results and details of the technique in 1956. [30] It was designed to reduce postoperative pain and avoid anal and rectal stenosis. It is indicated for second- to fourth-degree hemorrhoids. A Parks retractor is inserted. A point just below the dentate line at the hemorrhoid is grasped with a hemostat. A 30-40-mL saline containing 1:400,000 parts adrenaline is injected submucosally to open up tissue planes and to reduce bleeding. Scissors are used to excise a small diamond of anal epithelium around the hemostat. The incision is continued cranially for 2.5 cm, creating two mucosal flaps on each side, which are each grasped with further hemostats, and submucosal dissection is commenced to remove the hemorrhoidal plexus from underlying internal sphincter muscle and overlying mucosa. This dissection is continued into the rectum, where the resulting broad base of tissue is suture-ligated and divided. The mucosal flaps are then allowed to flop back into position. No suture or any intra-anal dressing is used. Parks advocated use of suture for only prolapsed hemorrhoid to reconstitute the mucosal ligament,' but most contemporary descriptions advocate suturing the mucosal flaps loosely together and to the underlying internal sphincter. The same procedure is carried out on the other hemorrhoids. Parks hemorrhoidectomy is done under general or epidural anesthesia. It is safe and associated with low rates of complications and recurrence. [30] It however takes longer time and is more difficult to learn. A recent study by Yang et al., 2005, concludes that the modified lift-up submucosal hemorrhoidectomy is an easier operative method compared with the procedure originally developed by Parks. [31]
Whitehead's circumferential hemorrhoidectomy
This procedure, also known as total or circumferential hemorrhoidectomy, was first described by Dr. Walter Whitehead in 1882. [32] After initial success, the procedure was later abandoned due to the high complication rates encountered: hemorrhage, anal stenosis, and ectropion (Whitehead's deformity). The procedure entails circumferential removal of the hemorrhoid, hemorrhoid-bearing. rectal mucosa just proximal to the dentate line. Incisions are made by curved double-operating scissors just proximal to the dentate line and continued along this path around the anal canal in stages. Clamps are used to lift the cut edge of the hemorrhoid rectal -bearing mucosa and mucosal prolapse. The hemorrhoidal masses are then suture-ligated and excised, followed by closure of the incisions by suture. Here, a retractor is used to stretch the internal sphincter, so that the suture goes through the endoderm to the neo-dentate line. A hemostatic sponge is left in the anal canal. The procedure is reserved only for circumferential hemorrhoids, and it is done under general or epidural anesthesia. Recent works by Maria et al. have shown that the Whitehead's hemorrhoidectomy still has a place in selected cases of circumferential hemorrhoids. [32]
Stapled hemorrhoidectomy
This procedure is also known as circumferential mucosectomy or 'procedure for prolapse and hemorrhoids' (PPH). It was first described in 1998 by Longo for prolapsing second- to fourth-degree hemorrhoids. [33] He suggested that stapled resection of a complete circular strip of mucosa above the dentate line lifts the hemorrhoidal cushions into the anal canal. [33] In PPH, the prolapsed tissue is pulled into a circular stapler that allows the excess tissue to be removed while the remaining hemorrhoidal tissue is stapled. A circular anal dilator is introduced into the anal canal. The prolapsed mucous membrane falls into the lumen after removing the dilator. A purse-string suture anoscope is then introduced through the dilator, to make a submucosal purse-string suture around the entire anal canal circumference [Figure 7]. The circular stapler is opened to its maximum position. Its head is introduced and positioned proximal to the purse-string suture, which is then tied with a closing knot [Figure 8]. The entire casing of the stapler is then pushed into the anal canal, tightened and fired to staple the prolapse. Firing the stapler releases a double-staggered row of titanium staples through the tissue [Figure 9]. A circular knife excises the redundant tissue, thereby removing a circumferential column of mucosa from the upper anal canal. The staple line is then examined with the anoscope for bleeding, which if present may be controlled by placement of absorbable sutures. The staple line should be maintained at a distance of 3-3.5 cm from the anal verge to avoid postoperative rectal stenosis and pain. Patients experience less pain and achieve a quicker return to work compared to conventional procedures; and bleeding is less. [33]
Radiofrequency ablation and suture fixation of hemorrhoids
It is an innovative procedure designed in 1998 by Gupta for hemorrhoids of grades III and IV. [34] The procedure entails the use of an Ellman dual-frequency, 4-MHz radiofrequency generator for ablation of hemorrhoids. Radiofrequency waves ablate tissue by converting radio waves into heat. The alternating current generates changes in the direction of ions within the tissue fluid. This creates ionic agitation and frictional heating, leading to coagulative necrosis of tissue. Thereafter, the hemorrhoids are plicated using strong absorbable sutures. The plication begins from the most distal end of the hemorrhoid at the anal verge and is carried towards the pedicle in a continuous locking manner and knotted at the pedicle, thereby fixing the hemorrhoidal mass. [35] It gives better results in terms of postoperative pain and bleeding than stapled hemorrhoidectomy and Doppler-guided hemorrhoidal artery ligation. [36]
Pile 'suture' method
Also called the pile stitching method, it was first described in 1978 by Faraq for hemorrhoids of grades II and III. The method entails use of three interrupted sutures to secure the hemorrhoids in place without excision. [37]
Recurrence is a common postoperative complication of this procedure.
Bipolar diathermy hemorrhoidectomy
This operation is indicated mostly for second- to fourth-degree hemorrhoids. With the aid of a bipolar diathermy set on cutting and coagulation, dissection is carried from a V-shaped incision in the skin around the base of the hemorrhoid unto the pedicle, which is dissected and divided [Figure 10]. The diathermy is set on coagulation only during dissection and division of the pedicle. No ligature is used. A randomized trial study by Andrews et al. showed that diathermy hemorrhoidectomy has no significant advantage over the Milligan-Morgan procedure. [38]
Ligasure and Starion hemorrhoidectomy with submucosal dissection
The ligasure vessel-sealing generator is an isolated-output electrosurgical generator that provides power for vessel sealing and bipolar surgery. [39] It provides precise thermal energy delivery and electrode pressure to vessels to achieve complete and permanent fusion of the vessel lumen. The Starion thermal welding system is similar to the ligasure generator but uses the tissue-welding technology to simultaneously fuse vessels and tissue structures closed. The operating temperature is less than 100°C, thereby producing less heat and collateral tissue damage. The operation is done under general or epidural anesthesia. A V-shaped incision at the junction of the hemorrhoid and the peri-anal skin is made by a scalpel, followed by dissection of the hemorrhoidal bundles off the underlying sphincter. The ligasure or Starion handset is applied to the dissected hemorrhoids and activated to seal mucosal edges and divide the pedicle. A hemostatic sponge is inserted into the anal canal. Wang et al. demonstrated that the Starion hemorrhoidectomy has less postoperative pain and parenteral analgesic requirement than ligasure hemorrhoidectomy, but both have the same advantages of shorter operating time and less blood loss. [39]
Postoperative complications of hemorrhoidectomy
Early - severe postoperative pain lasting 2-3 weeks; wound infection; bleeding; edema of the skin bridges; major short-term incontinence; difficult urination or urinary retention; delayed hemorrhage, usually 7-16 days postoperatively, [40] which is probably due to sloughing of vascular pedicles or infection.
Late - anal stenosis, formation of skin tags, recurrence. [40]
 Conclusion Conclusion | |  |
The surgical options for the treatment of hemorrhoids are many; and even though the majority of surgical techniques are based on the ligation and excision principles, newer techniques are designed to minimize tissue dissection with the aim of reducing postoperative pain and bleeding.
 References References | |  |
| 1. | Cohen Z. Alternatives to surgical haemorrhoidectomy. Can J Surg 1985;28:230-1. 
[PUBMED] |
| 2. | Ellesmore S, Windsor AC. Surgical History of Haaemorrhoids. In: Charles MV, editor. Surgical Treatment of Haemorrhoids. London: Springer; 2002. p. 1-4. 
|
| 3. | Shampo MA. Brief history of colorectal surgery. J Pelvic Surg 1998;4:259 - 267 
|
| 4. | Beck DE. Hemorrhoidal disease. In: Beck DE, Wexner SD, editors. Fundamentals of anorectal surgery. 2 nd ed. London: W B Saunders; 1998. p. 237-53. 
|
| 5. | Brisinda G. How to treat haemorrhoids. BMJ 2000;321:582-3. 
[PUBMED] [FULLTEXT] |
| 6. | Gartell PC, Sheridan RJ, McGinn FP. Outpatient treatment of haemorrhoids: A randomized clinical trial to compare rubber band ligation with phenol injection. B J Surg 1985;72:478-9. 
|
| 7. | Macrae HM, McLeod RS. Comparison of hemorrhoidal treatments: A Meta - analysis. Can J Surg 1997;40:14-7. 
[PUBMED] |
| 8. | Mann CV, Russell RC, Williams NS. Bailey and Love's Short Practice of Surgery. 22 nd ed. London: Chapman and Hall; 1995. p. 873-4. 
|
| 9. | Charua GL, Avendano EO, Hernandez CF. Infrared photocoagulation in the treatment of hemorrhoids. Rev Gastroenterol Mex 1998;63:131-4. 
|
| 10. | Ambrose NS, Morris D, Alexander-Williams J, Keighley MR. A randomized trial of photocoagulation or injection sclerotherapy for the treatment of first-and second - degree hemorrhoids. Dis Colon Rectum 1985;28:238-40. 
[PUBMED] |
| 11. | Mashiah A, Mashiah T. Cryosurgery for life-threatening bleeding hemorrhoids in the elderly. J Am Geriatr Soc 1984;32:62-3. 
[PUBMED] |
| 12. | O'Callaghan JD, Matheson TS, Hall R. Inpatient treatment of prolapsing piles: Cryosurgery versus Milligan -Morgan haemorrhoidectomy. Br J Surg 1982;69:157-9. 
[PUBMED] |
| 13. | Konsten J, Baeten CG. Hemorrhoidectomy Vs Lord's method: 17-year follow-up of a prospective randomized trial. Dis Colon Rectum 2000;43:503-6. 
[PUBMED] |
| 14. | Mortensen PE, Olsen J, Pedersen LK, Christiansen J. A randomized study on haemorrhoidectomy combined with anal dilatation. Dis Colon Rectum 1987;30:755-7. 
|
| 15. | Creve U, Hubens A. The effect of Lord's procedure on anal pressure. Dis Colon Rectum 1979;22:483-5. 
[PUBMED] |
| 16. | Zahir KS, Edwards RE, Vecchia A, Dudrick SJ, Tripodi G. Use of the NdYag laser improves quality of life and economic factors in the treatment of hemorrhoids. Conn Med 2000;64:199-203. 
[PUBMED] |
| 17. | Hodgson WJ, Morgan J. Ambulatory hemorrhoidectomy with CO 2 LASER. Dis Colon Rectum 1995;38:1265-9. 
[PUBMED] |
| 18. | Armstrong DN, Ambrose WL, Schertzer ME, Orangio GR. Harmonic scalpel Vs electro-cautery hemorrhoidectomy: A prospective evaluation. Dis Colon Rectum 2001;44:558-64. 
|
| 19. | Kwok SY, Chung CC, Tsui KK, Li MK. Double blind randomized trial comparing Ligasure and Harmonic Scalpel hemorhoidectomy. Dis Colon Rectum 2005;48:344-8. 
[PUBMED] |
| 20. | Atomizing Hemorrhoids. Available From: www.proctology.us/atomizing.php. [Last accessed on 2010 July 10]. 
|
| 21. | Morinaga K, Hasuda K, Ikeda TA. Novel therapy for hemorrhoids: Ligation of the hemorrhoidal artery with a newly devised instrument(Moricorn) in conjunction with a Doppler flow meter. Am J Gastroenterol 1995;90:610-3. 
|
| 22. | Felice G, Privitera A, Ellul E, Klaumann M. Doppler- Guided Haemorhoidal Artery ligation: An alternative to Haemorrhoidectomy. Dis Colon Rectum 2005;48:2090-3. 
[PUBMED] |
| 23. | Chamberlain J, Johnstone JM. The results of hemorrhoidectomy by clamp and cautery. Surg Gynaecol Obstet 1970;131:745-7. 
|
| 24. | Milligan ET, Morgan CN, Jones LE, Officer R. Surgical anatomy of the anal canal and operative treatment of haemorrhoids. Lancet 1937;11:1119-94. 
|
| 25. | Adotey JM, Jebbin NJ. Anorectal disorders requiring surgical treatment in the University Teaching Hospital, PortHarcourt. Niger J Med 2004;13:350-4. 
[PUBMED] |
| 26. | Uba AF, Ihezue CH, Obekpa PO, Iya D, Legbo JN. Open haemorrhoidectomy revisited. Niger J Med 2001;10:185-8. 
[PUBMED] |
| 27. | Uba AF, Obekpa PO, Ardill W. Open versus closed haemorrhoidectomy. Niger Postgrad Med J 2004;11:79-83. 
[PUBMED] |
| 28. | Pokharel N, Chhetri RK, Malla B, Joshi HN, Shrestha RK. Haemorrhoidectomy: Ferguson's(closed) Vs Milligan-Morgan's technique(open). Nepal Med Coll J 2009;11:136-7. 
[PUBMED] |
| 29. | Pescatori M. Closed hemorrhoidectomy. Ann Ital Chir 1995;66:787-90. 
[PUBMED] |
| 30. | Khosrovaninejad C, Marchal P, Daligaux S, Blaustein M, Martane G, Bodiou Ch. Submucosal hemorrhoidectomy with Parks technique: Prospective study of 327 patients. J Chir(Paris) 2008;145:37-41. 
|
| 31. | Yang HK, Lim CH, Shin HK, Kang CH, Jeong SK, Choi JP. Lift-up sub mucosal Hemorrhoidectomy. J Korean Soc Colo proctol 2005;21:145-51. 
|
| 32. | Maria G, Alfonsi G, Nigro C, Brisinda G. Whiteheads' hemorrhoidectomy. A useful surgical procedure in selected cases. Tech Coloproctol 2001;5:93-6. 
[PUBMED] [FULLTEXT] |
| 33. | Longo A. Treatment of haemorrhoidal disease by reduction of mucosa and haemorrhoidal prolapse with a circular stapling device: A new procedure. 6 th world congress of Endoscopy Surgery. Naples: Mundozzi Editore; 1998. p. 777-84. 
|
| 34. | Gupta PJ. Radio-ablation of advanced grades of hemorrhoids with radiofrequency. Curr Surg 2003;60:452-8. 
[PUBMED] [FULLTEXT] |
| 35. | Gupta PJ. Radio-frequency ablation and plication of hemorrhoids. Tech Coloproctol 2003;7:45-50. 
[PUBMED] [FULLTEXT] |
| 36. | Gupta PJ. Radio-ablation and suture fixation of advanced grades of hemorrhoids. An effective alternative to staplers and Doppler-Guided ligation of hemorrhoids. Rev Esp Enferm Dig 2006;98:1- 20. 
|
| 37. | Faraq AE. Pile Suture: A new technique for the treatment of hemorrhoids. Br J Surg 1978;65:293-5. 
|
| 38. | Andrew BT, Layer GT, Jackson BT, Nicholls RJ. Randomized trial comparing diathermy hemorrhoidectomy with the scissor dissection Milligan-Morgan operation. Dis Colon Rectum 1993;36:580-3. 
|
| 39. | Wang JY, Tsai HL, Chen FM, Chu KS, Chan HM, Huang CJ, et al. Prospective randomized, controlled trial of Starion Vs Ligasure hemorrhoidectomy for prolapsed hemorrhoids. Dis Colon Rectum 2007;50:1146-51. 
[PUBMED] |
| 40. | Sayfan J. Complications of Milligan-Morgan hemorrhoidectomy. Dig Surg 2001;18:131-3. 
[PUBMED] [FULLTEXT] |
[Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10]
[Figure 1]
| This article has been cited by | | 1 |
The Second Razavi International Proctology Congress |
|
| Afshin Heydari,Pier paolo Dalmonte,Reza Fazlalizadeh,Saeed Hashemzadeh,Aldo Infantino Sanvito,Filippo La Torre,Piercarlo Meinero | | Razavi International Journal of Medicine. 2013; 1(1): 38 | | [Pubmed] | [DOI] | | | 2 |
Elective surgery for hemorrhoidal complaints: The decision to operate |
|
| Hackford, A.W. and Lamb, M.N. and Miller, P.E. | | Seminars in Colon and Rectal Surgery. 2013; 24(2): 81-85 | | [Pubmed] | | | 3 |
Short term outcome of rubber band ligation versus open hemorrhoidectomy in terms of postoperative complications |
|
| Asghar Khan, M. and Khan, H. and Imran Khan, M. and Khan, A. and Naeem, M. and Muhammad Khan, S. and Alam Jan, W. | | Journal of Medical Sciences (Peshawar). 2013; 21(1): 19-22 | | [Pubmed] | | | 4 |
Elective surgery for hemorrhoidal complaints: The decision to operate |
|
| Alan W. Hackford,Melinda Nicole Lamb,Peter E. Miller | | Seminars in Colon and Rectal Surgery. 2013; 24(2): 81 | | [Pubmed] | [DOI] | | | 5 |
The Second Razavi International Proctology Congress |
|
| Afshin Heydari,Pier paolo Dalmonte,Reza Fazlalizadeh,Saeed Hashemzadeh,Aldo Infantino Sanvito,Filippo La Torre,Piercarlo Meinero | | Razavi International Journal of Medicine. 2013; 1(1): 38 | | [Pubmed] | [DOI] | |
|




 |
 |
|