|


 |
| SURGICAL TECHNIQUE |
|
| Year : 2012 | Volume
: 4
| Issue : 1 | Page : 15-18 |
|
|
Radiation-free insertion of distal interlocking screw in tibial and femur nailing: A simple technique
Ritesh Kumar Soni1, Surender Mohan Mehta1, Bhanu Awasthi1, Janith Lal Singh2, Amit Kumar3, Lokesh Thakur1, Sujit Kumar Tripathy2
1 Department of Orthopaedics, Dr. Rajender Prasad Government Medical College (RPGMC), Tanda, Kangra, India
2 Department of Orthopaedics, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
3 Department of Orthopaedics, Government Medical College, Chandigarh, India
| Date of Web Publication | 5-Sep-2012 |
Correspondence Address:
Ritesh Kumar Soni
Senior Resident, Department Of Orthopedics, Dr. RPGMC, Tanda, Kangra, H.P. - 176 001
India
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/2006-8808.100346

 Abstract Abstract | | |
Background: Distal interlocking screw insertion in intramedullary nailing of long-bone fracture is a challenging task for orthopedic surgeons. It is difficult particularly when the surgeon is in his learning stage or when image intensifier is not available. We describe a radiation-free technique of distal interlocking screw insertion which is easy and practicable. Materials and Methods: In this technique, a same length nail is placed over the skin (outer nail) and through its distal-most screw hole, a 3.2 mm drill bit is inserted to drill the distal locking screw hole of the intramedullary nail (inner nail). With a small skin incision over the distal screw holes, the distal-most screw hole is identified; the bone window overlying the screw hole is widened with an awl and a locking bolt is inserted with a washer under direct visualization. The other distal interlocking screw is simply drilled by matching the other three holes of the outer and inner nails. We have operated 86 patients (39 femoral shaft fracture and 47 tibial shaft fracture) in 1 year where this technique was used. There were 41 open fracture and 45 closed fracture. Results: Within 6 months of follow-up, bony union was achieved in 36 of 39 femur fractures and 45 of 47 tibial fractures. No unwanted complications were observed during the postoperative period and in follow-up. Conclusion: This method of radiation-free distal interlocking screw insertion is simple and can be used in third world country where image intensifier facility is not available. However, surgeons are encouraged to use image intensifier facility where the facility is available. Keywords: Intramedually nail, radiation, femur fracture, tibia frcature
How to cite this article:
Soni RK, Mehta SM, Awasthi B, Singh JL, Kumar A, Thakur L, Tripathy SK. Radiation-free insertion of distal interlocking screw in tibial and femur nailing: A simple technique. J Surg Tech Case Report 2012;4:15-8 |
How to cite this URL:
Soni RK, Mehta SM, Awasthi B, Singh JL, Kumar A, Thakur L, Tripathy SK. Radiation-free insertion of distal interlocking screw in tibial and femur nailing: A simple technique. J Surg Tech Case Report [serial online] 2012 [cited 2016 Jun 10];4:15-8. Available from: http://www.jstcr.org/text.asp?2012/4/1/15/100346 |
 Introduction Introduction | |  |
Intramedullary nailing is the standard treatment method for closed and most of the open fractures of the long-bone diaphysis. [1],[2] Targeting the distal holes of the intrameduallry (IM) nail for insertion of distal interlocking screws remain a challenge for the orthopedic surgeons. Proximally based distal targeting devices have not proved useful till date due to the deformation of the nail inside the medullary canal; [3] hence a free hand technique for insertion of distal interlocking screws under fluoroscopic guidance remains the most popular method. This process is technically demanding, time consuming, and afflicted to considerable radiation exposure of the patient and the surgical personnel. [4],[5],[6],[7],[8],[9],[10] Radiation induced cancer is a growing problem among orthopedic surgeons, associated with a relative risk for cancer of 5.37 with respect to the general population; [11] malignancies of exposed personnel range from cancers of solid organs (i.e., thyroid and pancreas), to skin and hematopoietic cancers. [12] In female orthopedic surgeons the standardized prevalence ratio for all cancers is 1.9 and 2.88 specifically for breast cancer when compared to the general population. According to Sanders et al. [5] who put dosimeter rings on the surgeon's hand for all orthopedic fluoroscopy cases, there is increased risk of positive reading with increased fluoroscopy time. The risk increased further during intramedullary nailing procedures. Gugala et al. reported a fluoroscopy time of 36 seconds for placement of two screws in the tibia, [13] whereas Suhm et al. stated intense use of fluoroscopy during freehand locking of 108 seconds per screw. [14] Factors such as experience level of the operator or experimental/clinical setup might contribute to this scattering. In the investigation of Kirousis et al. [15] a complete tibia nailing procedure required 72 seconds of radiation and resulted in an effective dose of 0.04 mSv for the operating surgeon and 0.11 mSv for the C-arm technician.
A number of techniques and systems have recently been developed to minimize the exposure of the radiation to the surgeons and the accompanying staff. [1],[3],[16],[17],[18],[19] Penning et al. have reported 100% accuracy for the placement of distal interlocking screws using Orthofix femoral and tibial intramedullary rods equipped with distal targeting devices. [20] All these techniques are either not available in developing countries or are still in their developmental stages. Secondly, insertion of distal interlocking screws requires an image intensifier and an experienced radiographer which sometimes are not available in developing and poor countries.
There is no study till date that describes the techniques of insertion of distal interlocking screws without the use of image intensifier or the X-rays. We hypothesized that our described technique in this article is a valid method of radiation-free insertion of distal interlocking screw in tibial and femoral nailing. The surgical technique, tips and pearls, and treatment outcome of a group of patients treated with IM nail without the help of image intensifier over a period of 1 year are described.
 Surgical Technique Surgical Technique | |  |
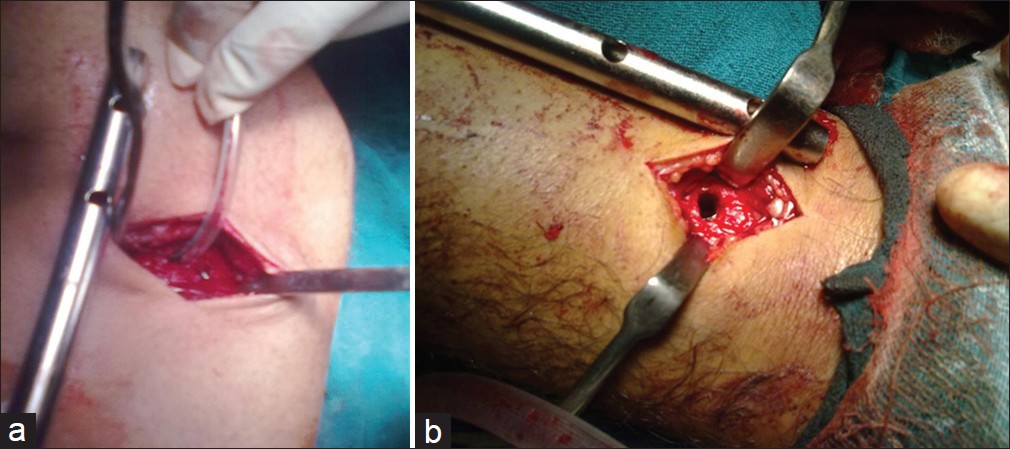
This technique in our setup had come more out of compulsion than anything else, due to lack of good intraoperative imaging modalities in the past. The method of inserting interlocking nails remains standard. After insertion to the fractured bone, a same length nail is juxtaposed over the limb and held in position with two long drill bits introduced through the proximal zig [as shown in the [Figure 1], [Figure 2] and [Figure 3]]. After aligning the outer nail with the proximal zig, a 5-6 cm long incision is given centering over the estimated site of the distal locking screws, the underlying long bone cortex is hence exposed [Figure 4]a. Now, through the distal most hole of the outer nail, the near cortex is drilled with a 3.2 mm drill bit. Using a corresponding bone awl, the hole is slightly enlarged [Figure 4]b. The intramedullary blood is then suctioned off from the hole with a Ryles tube (no. 12, 14) attached to a suction tube [Figure 5]a. Following this, the intramedullary nail and the distal hole could be clearly visualized [Figure 5]b. Once visualized, the tip of the awl is inserted into the hole and it is rotated perpendicular to the nail; this creates the entry point for the subsequent drill bit. A corresponding drill bit is then inserted through this hole and the opposite cortex drilled. The length of the screw is hence determined. Now, a free drill bit is passed through the distal locking holes of both the nails, this fixes the outer nail at three points [Figure 6]. With this alignment, the antecedent distal locking hole is usually a simple "drill and go." But, if doubt exists, a similar procedure could be applied for this hole as well. Since the hole in the near cortex is slightly enlarged, a washer is usually used to secure the locking screw heads [Figure 7], [Figure 8] and [Figure 9].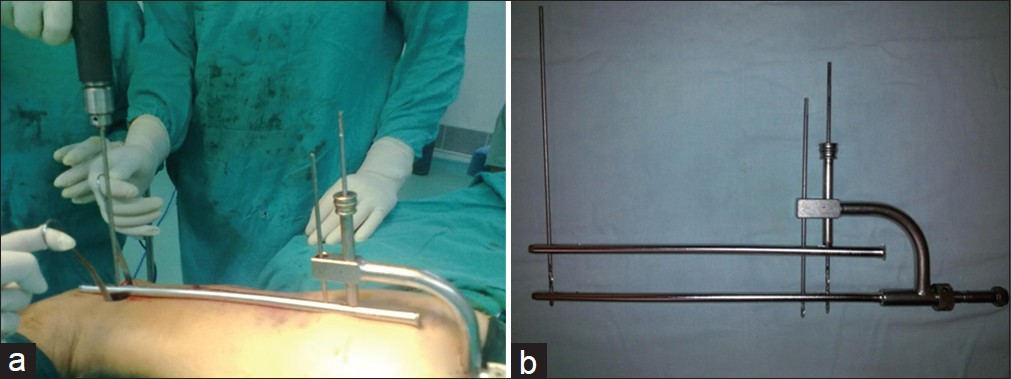 | Figure 2: (a) Picture depicting outer nail in juxtaposition (nail on nail); (b) Illustration showing the "nail on nail" technique with three point fixation
Click here to view |
 | Figure 4: (a) Incision given for tibial interlocking; (b) Enlargement of the near cortex using bone awl
Click here to view |
 | Figure 5: (a) Using Ryle's tube to suction intramedullary blood; (b) Enlarged distal tibial intramedullary nail hole
Click here to view |
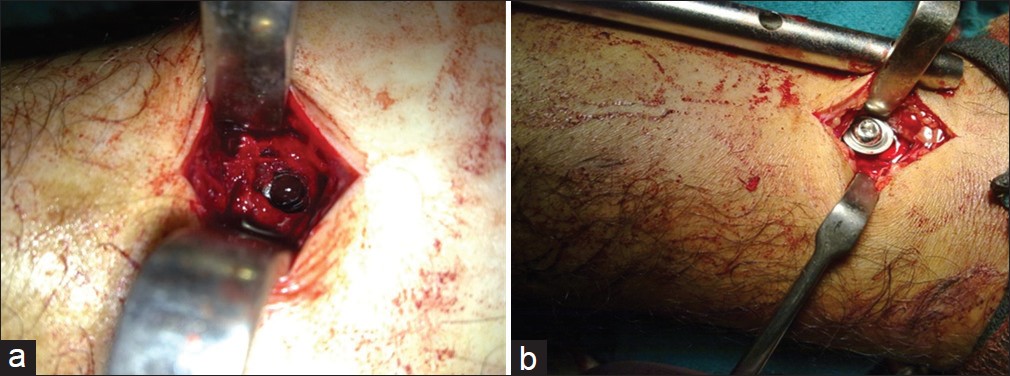 | Figure 6: (a) The distal hole in the intramedullary nail seen through bone; (b) Insertion of distal interlocking screw with washer
Click here to view |
 | Figure 9: (a) Wound site; (b) Postoperative photograph of fracture femur patient
Click here to view |
In summary, the key to our technique is the direct visualization of the distal locking holes combined with the use of corresponding bone awl and three point fixation of a juxtaposed outer nail.
 Materials and Methods Materials and Methods | |  |
Eighty-six cases of femoral and tibial shaft fractures were operated in our institute over a period of 1 year (January 2010-2011). Out of them, 73 were males and 13 were females. Of these, 39 had femoral shaft fractures and 47 had tibial shaft fractures. There were 41 open fractures (Gustilo Anderson grade 1-3B) and 45 closed fractures. Average age of the patients was 35.4 years (range 14-76 years). In all these cases, both of the distal screws were inserted without the use of image intensifier. Average time taken for inserting the distal screws was 11 minutes (range 5-18 minutes). More than two attempts of drilling near cortex were made in two cases. We resorted to placing bone grafts in addition to washers in these cases. All our patients were treated with the Simplified Universal Nails (SUN) supplied by the A.O. group. Interlocking was done in the lateral position in all cases of fracture femur and in supine position in fracture tibia. All the patients were mobilized immediately after surgery with partial weight bearing. Isometric quadriceps exercises and knee flexion were encouraged as tolerated by the patient. They were followed up after 3 weeks, 6 weeks, 3 months, and 6 months of surgery.
 Results Results | |  |
In the postoperative period, three patients had infection that needed debridement and antibiotic therapy. At the end of 6 months, radiographic union was observed in 36 of 39 femur fractures and 45 of 47 tibial fractures. The five patients with nonunion had open fracture. None of the patients complained of pain or tenderness at the distal screw sites. No clinical or radiological evidences of screw or nail breakage or fracture were noticed at the distal screw site.
 Discussion Discussion | |  |
When a nail is inserted into a long bone, it is likely to bend according to the curvature of the intramedullary canal. [3] Exact orientation of the distal interlocking holes is, hence, difficult to predict. Usually surgeons use repeated fluoroscopy to insert the screws in a freehand manner. In many centers of developing and poor countries, image intensifier facility is not available; hence surgeons adopt various indigenous techniques for distal screw insertion.
Our technique is especially suited for institutions where either image intensifier or expert radiographer is not available in the operation theatre. This technique is different from the "nail on nail" technique described by Rohilla et al., [3] because it does not involve the use of "sounding technique," rather it aims at direct visualization of the locking hole, drilling under vision and the use of corresponding bone awl. The major advantage of our technique is that since everything is being done under direct vision, the chance of misplaced screws is less and the operating time is less. Again under direct vision, the chance of slippage of the drill bit on the bone is less.
Tanna et al. [1] also described similar technique using K-wires which is image intensifier independent. However, it still depends on single radiographic imaging for estimating the location of the distal hole. In our technique, image intensifier or X-rays are very rarely used intraoperatively. While the success of their technique relies on interpretation of X-rays, our method relies on appropriate alignment of the outer nail and adequate widening of the near cortex so that the distal holes could be visualized.
There are few potential drawbacks of the proposed technique. The length of incision for interlocking distal screws is larger than that those given during the free hand technique (about 5-6 cm compared to 1-2 cm). We have not compared it with any other method of interlocking; hence claims of superiority are at present largely anecdotal. Further studies are needed to evaluate the effect of widening of the near cortex on fracture healing. So far, we have not encountered any fracture through distal screws with our technique. A big hole around distal screw may act as stress riser. The potential complications of iatrogenic fracture, delayed union or nonunion cannot be avoided with our proposed technique. Definitely this technique cannot be employed in situations where bone quality is poor or in osteoporotic individuals. A snugly fit screw provides better biomechanical strength and hence one may argue about the stability of the fixation with the described technique. Use of washer beneath the screw in larger hole may increase the stability. The cause of nonunion in five cases is difficult to explain in the present series. All patients with nonunion had open fracture which is an important cause for nonunion. Thus, it is difficult to explain whether the nonunion is because of open nature of injury or because of biomechanical disadvantage of distal screw interlocking in a wide hole.
Other than the risk of radiation exposure, distal screw insertion under fluoroscopy is definitely ideal and should be performed where the facility is available. Our described technique is particularly useful in situations where image intensifier or trained radiographers are not available. It is hence more suitable for rural hospitals and third world countries or in situations where image intensifier have failed technically. It does not need any special equipment and learning curve is also not very steep.
 Acknowledgment Acknowledgment | |  |
This study was conducted at Dr. RPGMC Tanda, Kangra, H.P. at the Department of Orthopedics. This paper was presented in NZIOACON 2011 in Feb 2011 and was awarded best paper award.
 References References | |  |
| 1. | Tanna DD. Interlocking tibial nailing without an image intensifier. J Bone Joint Surg 1994;76B:670. 
|
| 2. | Lam SW, Teraa M, Leenen LP, van der Heijden GJ. Systematic review shows lowered risk of nonunion after reamed nailing in patients with closed tibial shaft fractures. Injury 2010;41:671-5. 
[PUBMED] |
| 3. | Rohilla R, Singh R, Maggu N, Devgun A, Siwach R, Gulia A. Nail over nail technique for distal locking of femoral intramedullary nails. Int Orthop 2009;33:1107-12. 
|
| 4. | Miller ME, Davis ML, MacClean CR, Davies JG, Smith BL, Numpries JR. Radiation exposure and associated risks to operating room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg 1983;65A:1-4. 
|
| 5. | Riley SA. Radiation exposure from fluoroscopy during orthopaedic surgical procedures. Clin Orthop 1989;248:257-60. 
[PUBMED] |
| 6. | Sanders R, Koval KJ, DiPasquale T, Schmelling G, Stenzler S, Ross E. Exposure of the orthopaedic surgeon to radiation. J Bone Joint Surg 1993;75A:326-30. 
|
| 7. | Barry TP. Radiation exposure to an orthopaedic surgeon. Clin Orthop 1984;182:160-4. 
[PUBMED] |
| 8. | Levin PE, Schoen RW, Browner BD. Radiation exposure to surgeon during closed interlocking intramedullary nailing. J Bone Joint Surg 1987;69A:761-6. 
|
| 9. | Skjeldal S, Backe S. Interlocking medullary nails-radiation doses in distal targeting. Arch Orthop Trauma Surg 1987;106:179-81. 
[PUBMED] |
| 10. | Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy. J Orthop Trauma 1997;11:392-8. 
[PUBMED] |
| 11. | Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg 2005;13:69-76. 
[PUBMED] |
| 12. | Chou LB, Cox CA, Tung JJ, Harris AH, Brooks-Terrell D, Sieh W. Prevalence of cancer in female orthopaedic surgeons in the United States. J Bone Joint Surg Am 2010;92:240-4. 
[PUBMED] |
| 13. | Gugala Z, Nana A, Lindsey RW. Tibial intramedullary nail distal interlocking screw placement: Comparison of the free-hand versus distally-based targeting device techniques. Injury 2001;32:21-5. 
[PUBMED] |
| 14. | Suhm N, Messmer P, Zuna I, Jacob LA, Regazzoni P. Fluoroscopic guidance versus surgical navigation for distal locking of intramedullary implants. A prospective, controlled clinical study. Injury 2004;35:567-74. 
[PUBMED] |
| 15. | Kirousis G, Delis H, Megas P, Lambiris E, Panayiotakis G. Dosimetry during intramedullary nailing of the tibia. Acta Orthop 2009;80:568-72. 
[PUBMED] |
| 16. | Holistien S, Ruth JT. Electromagnetic distal targeting for the placement of transverse interlocking screws. Osteoporos Int 1996;3:196-203. 
|
| 17. | Hudson I. Locking nailing: An aid to distal targeting. Injury 1989;20:129-30. 
[PUBMED] |
| 18. | Kelly SS, Bonar S, Hussamy OD, Morrison JA. A simple technique for insertion of distal screws into interlocking nails. J Orthop Trauma 1995;9:227-30. 
|
| 19. | Krettek C, Koenemann B, Miclau T, Schanelmaier P, Blauth M, Tscherne H. A new method for distal locking of unreamed tibial nails. J Orthop Trauma 1996;11:446-51. 
|
| 20. | Krettek C, Manss J, Koenemann J, Miclau T, Schanelmaier P, Tscherne H. The deformation of small diameter solid tibial nails with unreamed intramedullary insertion. J Biomech 1997;30:391-4. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9]
|