|


 |
| CASE REPORT |
|
| Year : 2012 | Volume
: 4
| Issue : 2 | Page : 132-134 |
|
|
Management of Chronic Subdural Haematoma in a Case of Idiopathic Thrombocytopenic Purpura
Ashis Patnaik, Sudhansu S Mishra, Satya B Senapati, Acharya S Pattajoshi
Department of Neurosurgery, SCB Medical College and Hospital, Cuttack, Odisha, India
| Date of Web Publication | 8-Apr-2013 |
Correspondence Address:
Ashis Patnaik
Department of Neurosurgery, Flat No. 313, Metro Manorama Complex, Kathagola Sahi, Mangalabag, Cuttack 753 007, Odisha
India
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/2006-8808.110265

 Abstract Abstract | | |
Intracranial hemorrhage is a rare devastating complication of idiopathic thrombocytopenic purpura (ITP), mostly presenting as intraparenchymal or subarachnoid haemorrhage. Isolated chronic subdural haematoma (SDH) is still very rare and the optimal management is unsettled. Spontaneous resolution of chronic SDH in patients with idiopathic thrombocytopenic purpura is possible. We report a case of spontaneous chronic SDH in a patient with ITP with hemiparesis where the haematoma significantly decreased in size with complete resolution of hemiparesis as a result of platelet transfusions and continuing therapy with steroids. Surgical treatment of subdural haematoma with consequent bleeding complications can be avoided in this scenario. Keywords: Chronic subdural haematoma, hemiparesis, idiopathic thrombocytopenic purpura, platelet transfusion
How to cite this article:
Patnaik A, Mishra SS, Senapati SB, Pattajoshi AS. Management of Chronic Subdural Haematoma in a Case of Idiopathic Thrombocytopenic Purpura. J Surg Tech Case Report 2012;4:132-4 |
How to cite this URL:
Patnaik A, Mishra SS, Senapati SB, Pattajoshi AS. Management of Chronic Subdural Haematoma in a Case of Idiopathic Thrombocytopenic Purpura. J Surg Tech Case Report [serial online] 2012 [cited 2016 Jun 10];4:132-4. Available from: http://www.jstcr.org/text.asp?2012/4/2/132/110265 |
 Introduction Introduction | |  |
Idiopathic thrombocytopenic purpura is an autoimmune disease, more commonly found in women of reproductive age group where platelets undergo premature destruction as a result of autoantibody or immune complex deposition on their membranes and their subsequent removal by reticuloendothelial system. Platelet dysfunction predisposes the patients to various bleeding tendencies such as purpuric spots in the skin, gum bleeding, haemarthrosis, menorrhagia, excessive and prolonged bleeding from the wounds. Intracranial hemorrhages are one of the devastating complication of ITP, [1],[2] still it occurs in less than 1% of patients. Despite the fact that optimal management of symptomatic chronic subdural haematoma with mass effect and hemiparesis is usually surgical evacuation, treatment of this condition associated with ITP is guarded in view of increased risk of intra-operative and peri-operative bleeding. In this case conservative management has also resulted in clinico-radiological improvement.
 Case Report Case Report | |  |
A 19-year-old female patient was admitted with a history of headache and vomiting for last 1 month. Headache was more or less continuous and throbbing in nature, gradually increasing in intensity. There was history of right sided weakness since last 15 days. She had past history of menorrhagia at the time of menarche 5 years ago, for which she was treated conservatively and at this time she was diagnosed as a case of idiopathic thrombocytopenic purpura (ITP). She also had history of prolonged bleeding from wounds, gum bleeding, petechial rashes since birth. On examination she was conscious and normotensive, pallor present. Few purpuric spots were noted on her upper limbs. Patient was advised to take corticosteroids by her physician, but she was not taking any medication at the time of presentation. Neurologic examination showed an alert individual with normal higher functions with grade 2 power in both upper and lower limbs on right side. Hemiparesis developed gradually over a period of 20 days which corresponded to slow increase in the size of the chronic subdural haematoma and pressure effect over motor cortex. Ocular fundi showed bilateral papilloedema and cranial nerves were normal. Motor, sensory and cerebellar systems were normal. Deep tendon reflexes were exaggerated with plantars being up-going on right side. Spleen was not palpable.
At the time of admission, haematological investigations revealed haemoglobin of 9.0 gm/dl with normal total and differential leukocytic counts. Platelet count was 30,000/mm 3 . Liver and renal function tests were normal. Bone marrow aspiration cytology showed an increase in the megakaryocyte series, which consisted of monolobate and multilobate forms. CT scan of the brain showed a hypodense lesion at left posterior parietal and occipital region suggestive of chronic subdural haematoma with significant mass affect with effacement of ipsilateral ventricles [Figure 1]. She was given two units of platelet rich plasma (PRP) and three units of single donor platelet (SDP) with which the platelet count rose to 48,000/mm 3 over a period of 15 days. This was done so as to make the patient fit for surgery and reduce chances of intra- and perioperative bleeding. However, she showed steady improvement in her symptoms with headache decreasing in frequency and intensity and no vomiting. Motor power on right side improved to grade 4. All these occurred gradually over a period of 15 days. CT scan of the brain repeated 22 days after admission showed gross resolution of subdural haematoma with no mass effect [Figure 2]. Another 2 units of platelet transfusions given. Her platelet counts were serially monitored. At the time of discharge, the platelet count was 60,000/ml and she was able to walk with complete power on right side. She was started on maintenance dose of steroids (10 mg/day) to reduce the platelet destruction by auto-antibodies.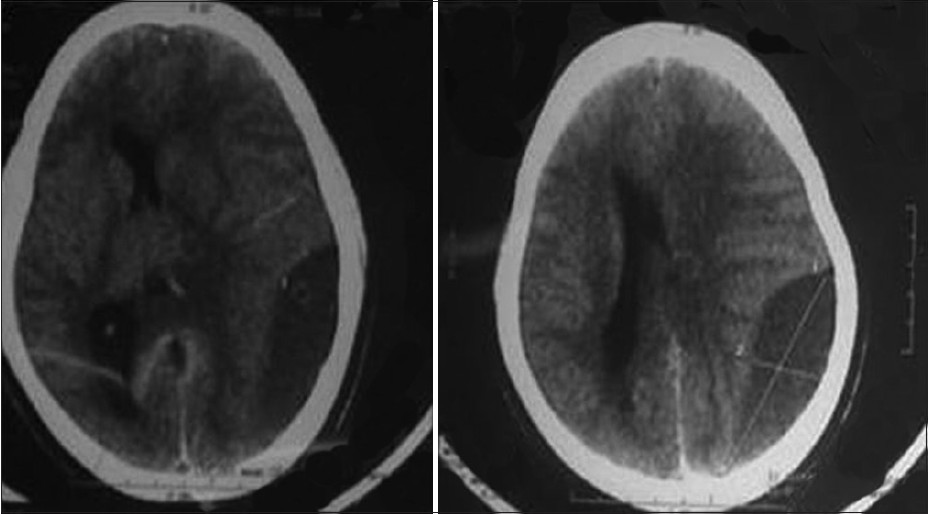 | Figure 1: Chronic subdural haematoma with midline shift and gross mass effect
Click here to view |
 Discussion Discussion | |  |
Platelets play a very important role in haemostasis by forming thrombic plugs which helps in occluding small vessels particularly capillaries. Platelet dysfunction leads to leaking capillaries and this may become confluent in longstanding cases to give rise to large haematoma. In central nervous system this usually leads to life threatening intracerebral or subarachnoid hemorrhage. Chronic subdural haematomas are extremely rare in ITP and a few number of cases have been reported in literature. [1],[2],[3],[4],[5]
Chronic subdural haematomas usually have a inner and a outer capsule. The capillary endothelial cells of these capsules have cytoplasmic protrusions and fenestrations. Previously according to Gardner's hypothesis, gradual enlargement of chronic subdural haematomas was thought to be due to passage of CSF due to osmolarity difference created by blood degradation products. But recently it has been proposed to be due to repeated microhaemorrhgaes into the haematoma cavity from the leaking capillaries. This may be the underlying pathology of chronic subdural haematoma in ITP where there is no trauma component, rather a dysfunctional platelet action promoting the capillary leak. This leaking component may overwhelm the normal resorptive course of chronic subdural haematomas leading to its enlargement. Repeated platelet transfusions can restore their count to normal thereby preventing repeated microhaemorrhgaes and giving the normal resorption course of chronic subdural haematomas, a chance. In addition corticosteroids prevent the formation of capsule of chronic subdural haematomas. Chronic subdural haematomas typically have concave shape, but presence a thick, vascular dural membrane forms that can be a source for repeated episodes of micro-hemorrhage in the setting of idiopathic thrombocytopenic purpura can explain the biconvex shape of the haematoma. Such biconvex shape of the chronis subdural haematoma has been described in the literature. [6]
In view of the rarity of the condition no definite guidelines exist, as to the management of chronic subdural haematomas associated with idiopathic thrombocytopenic purpura. The site, size, the presence of midline shift on CT scan as well as the patient's neurological status decide the management protocols. [2]
In our case the patient was complaining of severe headache, vomiting with hemiparesis with gross mass effect radiologically, requiring emergency evacuation of haematoma to prevent sudden deterioration due to herniation. So operative intervention was planned after raising the platelet to atleast 50,000/mm 3 . But as the patients' relatives were not willing to take the high risk associated with intra and post-operative bleeding, hence the patient was managed conservatively. Surprisingly patient's symptoms particularly motor weakness completely resolved over a period of 1 month after raising the platelet count. This may have been possible due to inhibition of repeated capillary micro-haemorrhages by improved platelet function.
Our case showed that trial of conservative management with elevation of platelet count can be suggested in a case of chronic subdural haematoma associated with idiopathic thrombocytopenic purpura as there is chance of spontaneous resolution with elevation of platelet count. Hemiparesis due to mass effect totally resolved thereby achieving our goal ultimately. This conservative management of chronic subdural haematoma in patients of idiopathic thrombocytopenic purpura and subsequent successful resorption prevents possible disastrous intra-operative bleeding and post-operative rebleeding.
 References References | |  |
| 1. | Sreedharan PS, Rakesh S, Sajeev S, Pavithran K, Thomas M. Subdural haematoma with spontaneous resolution-rare manifestation of idiopathic thrombocytopenic purpura. J Assoc Physicians India 2000;48:432-4. 
|
| 2. | Meena AK, Murthy JM. Subdural haematoma in a patient with immune thrombocytopenic purpura. Neurol India 1999;47:335-7. 
[PUBMED]  |
| 3. | Panicker JN, Pavithran K, Thomas M. Management of subdural hematoma in immune thrombocytopenic purpura: Report of seven patients and a literature review. Clin Neurol Neurosurg 2009;111:189-92. 
|
| 4. | Seçkin H, Kazanci A, Yigitkanli K, Simsek S, Kars HZ. Chronic subdural hematoma in patients with idiopathic thrombocytopenic purpura: A case report and review of the literature. Surg Neurol 2006;66:411-4. 
|
| 5. | Sebe A, Ohshima T, Ebisudani D, Oka H, Matsumoto K, Yoshizima S. A case of chronic subdural hematoma associated with idiopathic thrombocytopenic purpura (ITP). No Shinkei Geka 1990;18:761-5. 
|
| 6. | Agrawal A. Bilateral biconvex frontal chronic subdural hematoma mimicking extradural hematoma. J Surg Tech Case Rep 2010;2:90-1. 
|
[Figure 1], [Figure 2]
| This article has been cited by | | 1 |
Spontaneous Disappearance of a Large Chronic Subdural Hematoma: A Pleasant Surprise |
|
| Hanish Bansal,Anuj Mahajan,Apinderpreet Singh,Ashwani Chaudhary | | Indian Journal of Surgery. 2015; 77(6): 532 | | [Pubmed] | [DOI] | | | 2 |
Therapeutic Suggestions for Chronic Subdural Hematoma Associated with Idiopathic Thrombocytopenic Purpura: A Case Report and Literature Review |
|
| Hajime Takase,Junya Tatezuki,Naoki Ikegaya,Daisuke Yamamoto,Mizuki Hashimoto,Makoto Takagi,Yasuhiko Mochimatsu,Nobutaka Kawahara | | NMC Case Report Journal. 2014; 2(3): 118 | | [Pubmed] | [DOI] | |
|




 |
 |
|