|


 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 7
| Issue : 1 | Page : 1-3 |
|
|
Female urethral duplication: Rare anomaly with unusual presentation
Shailesh Solanki, M Narendra Babu, Vinay Jadhav, Gowrishankar, S Ramesh
Department of Pediatric Surgery, Indira Gandhi Institute of Child Health Hospital, Bengaluru, Karnataka, India
| Date of Web Publication | 29-Jun-2016 |
Correspondence Address:
Shailesh Solanki
Indira Gandhi Institute of Child Health Hospital, Bengaluru, Karnataka
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2006-8808.184939

 Abstract Abstract | | |
Urethral duplication (UD) in females is a rare congenital anomaly and requires a high degree of clinical suspicion for diagnosis. The preoperative evaluation requires thorough investigations to delineate anatomy which is imperative for surgical reconstruction to provide excellent functional and cosmetic outcome. We describe the successful management of a 6-year-old girl with UD (presented as ambiguous genitalia and urinary incontinence) along with a review of pertinent literature. Keywords: Ambiguous genitalia, female pseudohermaphroditism, urethral duplication
How to cite this article:
Solanki S, Babu M N, Jadhav V, Gowrishankar, Ramesh S. Female urethral duplication: Rare anomaly with unusual presentation. J Surg Tech Case Report 2015;7:1-3 |
How to cite this URL:
Solanki S, Babu M N, Jadhav V, Gowrishankar, Ramesh S. Female urethral duplication: Rare anomaly with unusual presentation. J Surg Tech Case Report [serial online] 2015 [cited 2018 Jul 1];7:1-3. Available from: http://www.jstcr.org/text.asp?2015/7/1/1/184939 |
 Introduction Introduction | |  |
Urethral duplication (UD) is a rare congenital anomaly and is characterized by two urethras, which may be either partial or complete. The UD anatomy is different in males and females and hence the surgical management. The male UD divided into three types according to Effman's classification.[1] The females UD is classified according to plane (frontal or sagittal) of duplication into different types: (1) Double urethra and double bladder, (2) double urethra with single bladder, (3) accessory urethra posterior to the normal channel, (4) double proximal urethra and single distal urethra, and (5) single proximal urethra and duplicated distal urethra.[2] We are discussing a case of type five females UD presented as ambiguous genitalia with incontinence over continence.
 Case Report Case Report | |  |
A six-year-old child presented with ambiguous genitalia and urinary incontinence. The child had normal voiding and dribbling of urine from the abnormal perineal orifice (vaginal orifice) and had abnormal genitalia (hypertrophied clitoris). Physical examination revealed posterior displacement of the vaginal introitus and prominent clitoris with a narrow opening at the tip. No scrotal or labial structures were present and the perineum appeared flat and fused [Figure 1]. On further evaluation, the child had female karyotype (46XX) and sonography revealed normal Mullerian structures with normal kidneys and bladder. Retrograde urethrogram (RGU) was attempted through the opening at the clitoris but catheter could not be passed through it. Subsequently, evaluation under anesthesia, cystogenitoscopy, and contrast study was done; we could identify one tiny opening at the clitoral tip, which was very narrow and only admitting guide wire for 2 cm. During vaginoscopy, the vagina was roomy with the normal cervix. A urethral opening was present on the anterior wall of the vagina (2 cm proximal to vaginal orifice) and it (urethra) led into the normal bladder. Urethrogram and genitogram were done under fluoroscopy and delineated the anatomy, suggestive of UD [Figure 1], Inset]. Subsequently, the patient underwent feminizing genitoplasty with urethral reconstruction. The dorsal urethra was dissected, the distal 2 cm of the urethra was very narrow and atretic hence excised. The proximal portion of the dorsal urethra was well developed (good caliber), joined to the ventral urethra near its confluence into the vagina [Figure 2]a. The ventral urethra was dissected till communication to the vaginal wall and disconnected. The rent in the anterior vaginal wall and ventral urethra was repaired and soft tissue interposed in between the two suture lines [Figure 2]b. The distal continuity of the ventral urethra with the dorsal urethra (good caliber) was maintained and neourethra (i.e., proximal part consisted of the ventral urethra and the distal part consisted of the dorsal urethra) reconstructed [Figure 2]. Postoperative period was uneventful and the child was discharged after removal of all the catheters. On subsequent follow-up, the child had developed urethrovaginal fistula of 0.5 cm × 0.5 cm size, 2 cm distal to the bladder neck, and presented as postmicturition dribbling. Six months later, urethrovaginal fistula was repaired successfully from the perineal approach. The child is under follow-up and continent for urine (no urinary dribbling) at last visit with normal upper tracts.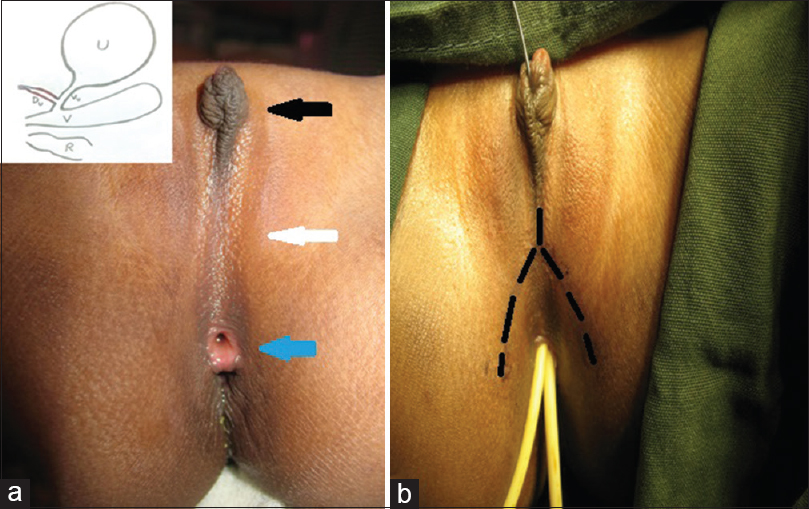 | Figure 1: (a) Hypertrophied clitoris (black arrow), flat perineum (white arrow), and vaginal orifice (blue arrow). (b) Black dotted mark represents incision. Inset showing preoperative anatomy. U: Urinary bladder, V: Vagina, R: Rectum, Du: Dorsal urethra (red color), Vu: ventral urethra
Click here to view |
 | Figure 2: (a) Distal dorsal urethra (black arrow) and proximal dorsal urethra (white arrow). The vagina (blue arrow) and its confluence (yellow arrow) with the ventral urethra. (b) Feminizing genitoplasty (black arrow). Soft tissue interposition (white arrow) in between the repaired vagina and urethra. Inset showing postoperative anatomy
Click here to view |
 Discussion Discussion | |  |
There is no embryological theory that explains all UD abnormalities.[3],[4],[5] Currently, widely accepted theory proposed by Patten et al. suggested an abnormal relationship between the lateral anlagen of the genital tubercle and the ventral end of the cloacal membrane.[2]
Indications for surgery include annoying symptoms such as a double stream (most common), urinary incontinence, ambiguous genitalia, perineal sinuses, urinary obstruction or infection, and associated genitourinary anomalies.
The preoperative evaluation requires a variety of radiological investigations and endoscopic procedures to define the anatomy. These include voiding cystourethrogram (VCUG), RGU, intravenous urography, sonourethrography, magnetic resonance imaging, and cystogenitoscopy. VCUG and RGU should be carried out in lateral projections for visualization of the size, shape, and position of the two channels.
Patients with UD can be asymptomatic and in such situation a conservative approach is acceptable. The range of management includes observation to trivial intervention like meatotomy/urethral dilatation to complex urethral reconstruction in severe cases.
Most duplication occurs in the sagittal plane one on top of the other. Less commonly, openings may lie collaterally (side by side) in the frontal plane. It is imperative to be aware of anatomy, continent status, and caliber of both the urethras during the preoperative evaluation. Usually the ventral urethra is continent and good caliber compared to the dorsal urethra; similar findings were present in the index case.
During surgical planning, the facts to be considered are continent urethra should be preserved, good caliber urethra should be used for reconstruction purpose, and excision of accessory urethra should be accomplished. The genital reconstruction depends on the severity of virilization.
In our case, the child presented with incontinence over continence with ambiguous genitalia. Hence, we had started investigations on two lines: Ectopic ureter and disorder of sex development. After cystogenitoscopy and contrast study, diagnosis was confirmed and anatomy of both urethras was well delineated. The incontinence was might be pseudo-incontinence because of the vaginal voiding, i.e. child might have been passing urine into the vagina during micturition and probably led to postvoid vaginal dribbling. The roomy vagina was also suggestive of the possibility for such type of pathology. We had planned to preserve ventral urethra as it was a continent and well developed. Moreover, well-developed part of the dorsal urethra had been used for urethral reconstruction to achieve adequate length. The occurrence of urethrovaginal fistula in the postoperative period was might be because of inadequate soft tissue interposition or overlapping suture line or due to vascularity-related issues. As urethrovaginal fistula was distal to the bladder neck area, the eventual continence status was not compromised.
 Conclusion Conclusion | |  |
UD is a rare cause for ambiguous genitalia in female and requires a high degree of clinical suspicion to diagnose the condition. The optimum management must be individualized and requires thorough investigations to delineate anatomy, which is crucial for surgical planning with the aim to provide excellent functional and cosmetic outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Effmann EL, Lebowitz RL, Colodny AH. Duplication of the urethra. Radiology 1976;119:179-85.  |
| 2. | Bhadury S, Parashari UC, Singh R, Kohli N. MRI in congenital duplication of urethra. Indian J Radiol Imaging 2009;19:232-4.  [ PUBMED]  |
| 3. | Casselman J, Williams DI. Duplication of the urethra. Acta Urol Belg 1966;34:535-41.  |
| 4. | Das S, Brosman SA. Duplication of the male urethra. J Urol 1977;117:452-4.  |
| 5. | Rice PE, Holder TM, Ashcraft KW. Congenital posterior urethral perineal fistula: A case report. J Urol 1978;119:416-7.  |
[Figure 1], [Figure 2]
|