|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 8
| Issue : 3 | Page : 146-152 |
|
Complications and management of hair dye poisoning in Khartoum
AA Elgamel1, NO Ahmed2
1 Forensic Science Institute, Poisons Center, The National Ribat University, Khartoum, Sudan
2 Omdurman Military Hospital, Department of Internal Medicine, Omdurman, Sudan
| Date of Web Publication | 16-May-2014 |
Correspondence Address:
A A Elgamel
Dean of the Forensic Science Institute, Khartoum
Sudan
  | Check |
DOI: 10.4103/1858-5000.132603 
Introduction: Paraphenylenediamine (PPD) is the major cause of intoxication in Sudan with high morbidity and mortality rate among the intoxicated victims. We here PPD poisoning studied in terms of mode of poisoning, case fatality rate, clinical presentation, management and complications. Methodology: This is a retrospective prospective study on 200 patients with hair dye poisoning who presented to Khartoum teaching hospital in the period from June 2008 to December 2008. Results: We reached to results that in the sample of 200 patients studied, (80.5%) were females and (19.5%) males. The ages of these patients ranged between 6 month - 57 years. Most of them were from Khartoum state (98.5%) and most of them were single (74%). About 51% had history of psychological problems. Most of them arrived immediately to the hospital (90%). Oral route is common route of administration of PPD (96%). The main causes of poisoning were suicidal attempts which occurred in (76%), accidental (22.5%) and homicidal (1.5%). The accessibility of dye to those patients was from local market accounts for about (47.9%), home (23.5%), relatives (22%) and other places (7.5%). Types of dye used were Indian (38.5%), Stone (42%) and Began account about (19.5%). PPD was detected in urine in (36%). There was impairment of renal function test using urea in (22%). Creatinine was abnormal in (23%). Serum electrolytes (sodium, potassium, Calcium) were abnormal in (11%).Uric acid was abnormal in (19.5%) and those who developed renal failure were (20.5%). The most common presentations were ingestion of dye (85.5%), tachycardia in (58%), tachypnea in (31.5%), vomiting in (31%), angioneuratic edema in (22.5%), abdominal pain (22%), enlarge tongue (18%), facial edema (14%) and loin pain in (7%) of the cases. The complications were respiratory distress in (22.5%), acute renal failure in (20.5%), cardiac problem in (1%) and liver problem in (0.5%). The medical treatment and emergency tracheostomy tend to decrease the mortality rate to only (3.5%). Relationship too many parameters were discussed. Recommendation: We recommended that may assist in decreasing the number of cases as health education about the danger of Hair dye that should be provided at the level of the community through all methods of mass media. Restriction should be made on the trade of Hair dye with more support analytical equipments in hospitals. Keywords: PPD, lawsonia alba, angionuoratic edema, contact allergy, tracheostomy, intoxication, renal failure, respiratory obstruction, suicidal.
How to cite this article:
Elgamel A A, Ahmed N O. Complications and management of hair dye poisoning in Khartoum. Sudan Med Monit 2013;8:146-52 |
[TAG:2]Introduction[/TAG:2]
A poison is chemical or physical agents that produce adverse effects when enter the human body. [1] Intoxication by hair dye is very common in Sudan and this usually attributed to the active ingredient paraphenylenediamine (PPD). [2]
Some other hair dyes exist where the active ingredient is different from PPD e.g., Naphthylamine, Toluenediamine and other aromatic amine compounds, but hairs dye that is used in Sudan composed of PPD which is synthetic semisolid dark greenish substance. [1]
Mechanism of intoxication either through the Topical route which means absorption through the skin (percutanious absorption) when it is used as a cosmetic to enhance darkening of lawsonia alba (Henna) or blackening of the hair. This can lead to sensitization which may be attributed to some genetic factor, oral ingestion or inhalation. [1]
Cutaneous absorption and ingestion produce sever local reactions and systemic effects. Investigation performed in a cases admitted to hospital had shown significant histopathological and biochemical changes. In the case reported by Suliman et al.,[3] the cardiovascular, respiratory and alimentary systems were normal. However the patient was anuric for 4 days.
A survey of suicide attempts using PPD in the capital Khartoum (Sudan), during the year 1987-1990 revealed that there were a total of 264 cases of suicidal attempts. In (35%) of them PPD was used, about (60%) of the cases were 10-20 years old and (30%) in the age group 21-30 years. The highest mortality rate (22.7%) was reported during year 1987. [4] El-Ansary et al. [5] in their study stated that 24 patients were admitted into Omdurman Hospital within 12 months, 12 patients took PPD intentionally and 8 of them died. Death was mainly due to acute respiratory distress. Over a period of 2 years a series of 18 cases of acute PPD poisoning were reported sporadically to the accident emergency department of Khartoum north hospital (Sudan). Two of the cases were babies about 18 months old. The reason for ingestion of PPD was mainly suicidal about (70%), the remaining was accidental. The mortality rate in this series was (22%). The exact dose taken by each patient was not known, however in severe cases, was estimated to be about 7 g (orally) to traces of PPD in mild cases. [6] Suliman et al.[3] in their study reported a case of 15 years old Sudanese girl attempted suicide by drinking a solution of PPD; they also reported 16 patients who developed toxicity of PPD after accidental, suicidal or homicidal ingestion. 12 of the patients died within 48 h of ingestion of PPD. The substance was identified by laboratory analysis as PPD using gas chromatography mass spectrometry. Lipid peroxidation is suggested to be responsible for tissue damage associated with PPD poisoning. This can be demonstrated histopathologicaly and biochemically by changes in cytoplasmic enzymes. [7]
Death may occur following ingestion or absorption of small amount although the lethal dose reported in the pharmacopeia is 10 g, this is due to the fact that about (4%) of people are usually sensitive to PPD while about (1%) are extremely sensitive. [1] Yagi et al.[6] reported cases of fatality also Charra, [8] Bariema [9] reported case fatality rate of (24%) while Osman [10] reported mortality rate of (20.9%) in Wad madani. However, Hamdouk [11] reported low case mortality rate of (11.8%). Study conducted by Sir Hashim [12] between 1981 and 1989 the case fatality rate was (41%) and highest mortality rate reported.
The usual pattern of intoxication are Suicidal; which constitute about (84%) of cases, Accidental; due to accidental ingestion especially in children which is about (8%) or through the skin absorption while used as cosmetic about (2%), Homicidal or criminal about (6%). [10]
PPD may also been found textile or fur dye dark colored cosmetic, temporary tattoos, photogenic developer, lithography plate, photocopy and printing ink, black rubber oils grease and gasoline. PPD required oxygen to be colored it is this intermittent partially oxidize state that may cause allergy in sensitive individuals.
Reaction cause by the use of hair dye in mild cases usually only involved dermatitis to the upper eyelids and ear, but may completely close the eyelids in more severe cases and allergic contact dermatitis reaction may become wide spread. [10] Teratogenicity was studied by applying four commercially available hair dye formulation containing 1, 2, 3 and (4%) of PPD. Teratogenicity was studied in 20 female rate. Each formulation was applied topically into a shaved site in the dorsoscapular region at dose of 2 ml/kg body weight on days 1, 4, 7.10, 13, 16 and 19 of gestation. Just prior to its use each formulation was mixed with equal volume of (6%) H 2 O 2 . The mothers were killed on day 20 of gestation. No abnormal fetal effect were noted except that in groups treated with formulation containing (2%) PPD there were skeletal change of life fetuses. Reverse mutation induce by PPD in Salmonella More Details typhimurium. [13]
The use of synthetic dye for coloring Hair dates back to 1883, it is an old tradition. Freshly prepared mixture of PPD and hydrogen peroxide (H 2 O 2 ) was used to produce this effect, [14] however it have been used commercially since 1878. PPD in a pure form was not known to be available for home application except for few countries e.g., Sudan, Morocco, Japan, UK and France. PPD produced commercially by reducing 1-amino4-nitrobenzen with iron and hydrochloric acid or iron and ferrous chloride. [15] About 10-100 thousand kg are produced annually in UK. Japan and USA also produce the same amount or more. The purity of the produce compound varies between (99%) and (99.5%). PPD is widely used as a hair dye and most of the hair dye formulation contains variable concentrations of PPD (0.2%, 3.75%). It is used in the industry of tyre cords, photographic developer, photochemical measurement and Varity of antioxidant. [6]
From [Table 1] it is evident that intoxication by hair dye is very common in Sudan and usually associated with active ingredient PPD which constitute significant source of aggregate of morbidity, mortality and health care expenditure. This study was initiated to asses some of the factors that lead to hair dye intoxication, determine symptoms and signs, management, complications, outcome of PPD poisoning and assess the relationship between the type of intoxication in relation with age, gender, route of administration and outcome.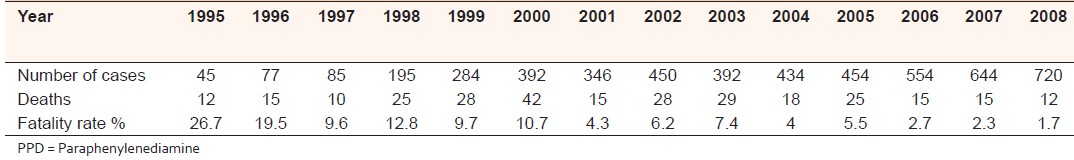 | Table 1: The number of cases intoxicated by PPD admitted in ENT Khartoum teaching hospital, deaths and case fatality rate from 1995 to 2008[2]
Click here to view |
| Materials and Methods | |  |
Study design
Retrospective-prospective descriptive hospital base case study design.
Study area
ENT Khartoum teaching hospital.
study population
People who came to ENT. Khartoum teaching hospital, suffering from PPD intoxication.
Sample size
A study sample consists of 200 patients who admitted to Khartoum teaching hospital due to PPD poisoning.
The data was collected by questionnaire to achieve the objective of the study.
The variables of the study were age, gender, residence, type and accessibility of dye, marital status, psychological problems, route of administration, type of intoxication, symptoms and signs, management and complications.
A sample of 200 patients presented to Khartoum teaching hospital after various form of exposure to PPD in the period from June/2008 to December/2008. The data was presented in the form of simple statistical frequency tables and figures.
Ethical consideration
An official latter was taken to approach the director of ENT Khartoum teaching hospital for permission to conduct the study.
| Results and Discussion | |  |
In the present study, a sample of 200 poisoned patients by PPD (hair dye) was studied. It was found that the peak incidences of PPD poisoning were between 14 and 27 years. This is nearly similar to Hamdouk [11] which reported a peak incidence at 17-27 years. Musa [16] reported the peak incidence between 21 and 30 years. This may be due to stress which increases at this age. (23.5%) of the patients were married. Marriage may add more stress on the individual. The age of all patients ranges in general between 6 month and 57 year.
Furthermore as noted by all previous studies females were found to be more affected by hair dye intoxication. This study found that (80.5%) were females and the (19.5%) were males [Table 2]. This is because females are subjected and exposed to PPD more than men due to cosmetic use of henna to enhance the blacking of hair and also it is used as a skin cosmetic. This is why when males came intoxicated usually it is suicidal (84.6%) while (24.2%) of females had accidental intoxication.
Statistical records showed that the incidence of PPD poisoning in Khartoum State was (77%) in the year 2000. This study showed that (98.5%) of patients came from Khartoum State (distributed as 36.5% from Khartoum province, 48.5% of patients from Omdurman province and 13.5% from Khartoum north province). The remaining (0.5%) came from El Gezira state and (1%) from River Nile. Musa [16] in their study reported (93.6%) of the cases came from Khartoum state (distributed as 61.2% from Khartoum province, 25% of patients from Omdurman province and 13.8% from Khartoum north province), (2.5%) from El Gezira state and (1.8%) from River Nile. The number of patients from Omdurman province increased in the present study.
Marital status in this study showed that most of the patients (74%) were single. This is the same when compared with the study of Musa [16] in which (62%) were single. In this study (89%) of married patients had suicidal attempts and (71.4%) of single were considered in the suicidal attempts group.
In this study, the psychological problems play major effects as predisposing factors for intoxication (about 51%). This is in Comparison to Musa [16] who reported that about (27.7%) of patients had psychological problems. This increase in percentage may be due to deterioration of economic status among Sudanese people and increase stress due to urbanization and complexity of life with problems that were not found in the past. This is supported by finding most of the patients have psychological problems in the intoxication that is suicidal (65.8%) and most of them have problems with their family.
It was found that about (67%) of patients developed the symptoms after minutes to 1 h. This may be due to exposure of the patient to large amounts of the dye, because (76%) of patients were in suicidal attempts.
Although most of the patients were in suicidal attempts but (90%) of them came early after appearance of symptoms. This may be due to serious and severe symptoms that cannot be tolerated by the patient. No previous study was found to compare with it. Only (10%) of the patients came late. The causes were that: The patients refuse to go to hospital with the suicidal tendency (about 5.5%); hospital is far (1%), or the patient start first to self-treatment by use of traditional medication (35%).
In this study about (96%) of the patients were exposed to hair dye through oral ingestion, compared with Musa [16] who also found the oral ingestion rates to (93.1%). This is because most of the patients had suicidal attempts and the suicidal attempt is better done by ingestion which always gives sufficient amount to cause death (>10 g of PPD which is the lethal dose). When correlation was made between the type of intoxication and the route of administration, it was found that all cases of suicidal attempts used the oral route and (17.8%) of accidental poisoning were by topical use.
In this study it was found that about (76%) of patients had suicidal attempts (78.3% were female and 21.7% were male). This is comparable to Musa [16] who reported about (76.1%) as suicidal attempts and accidental poisoning about (22.5%). When compared to Osman, [10] we find that he reported suicidal attempts constituted (84%) of cases, accidental poisoning about (10%) of the poisoned patients, homicidal (6%). Homicidal act is the least cause of poisoning in this study. This is the same as reported by Bariema. [9] A survey of suicidal attempts using PPD in capital Khartoum (Sudan), during the years 1987-1990 revealed that there was a total of 264 cases of suicidal attempts. In (35%) of them the PPD was used and about (60%) of the cases were 10-20 years old while (30%) of them in the age group 21-30 years. [4]
This study showed that accessibility of hair dye to patients is about (47%) from the local market and this is due to the increase sale of Indian type of hair dye in the local markets. Home accessibility is about (23.5%) in this study and most of them are stone type. In comparison the study of Musa, [16] where the source of PPD in (66%) was from home. In the past the Indian dye did not enter the market as in this time.
The type of dye used was the stone type in (42%). This may be due to high suicidal attempt and the concentration of PPD is more in stone form so it is expected to cause death quickly.
This study found that most of the intoxicated patients presented with ingestion of dye (accounted to about 85.5% of all patients). In some of them this was the only complaint (most of them is accidental), also other presenting symptoms included vomiting in about (31%) of all patients (vomiting exacerbate the upper respiratory tract obstruction due to re-exposure of mucous membrane to the toxic substance, which causes irritation and angioneuretic edema), angioneuretic edema in (22.5%), abdominal pain in (22%), woody enlarge tongue in (18%), difficulty in breathing in (18 %) and facial edema in (14 %). This is compared to Bariema [9] study (2002) in which about (42%) presented with wooden tongue, difficulty in breathing in (46%) and facial edema in (28%) of patients. Hamdauk [11] reported that the individual susceptibility to develop facial edema is not related to amount of dye that was taken by the patients. There are lots of other presenting features but not significant.
Presenting features became mild because now the patient comes early after exposure to hair dye because they know to some extent the dangers of it, and due to good transport facilities. Hence, patients come early and serious symptoms do not commonly occur.
Most of the patients (75.5%) stay in ENT hospital for only 1 day. Then the patients were either referred to other units to complete the treatment or discharged after complete recovery.
About (66%) of patients were referred to other units (70.45% of them referred to medicine unit and 8.33% to obstetrics unit, because there are 11 pregnant women in this study which were complicated by three abortions and one preterm labor. (13.64%) were referred to pediatrics because the children were 10% and all of them accidentally ingested the dye. One of them aged 6 months had taken breast milk containing PPD it was due to topical use by mother when she used the dye as cosmetic which was in the breast milk. (7.58%) referred to psychiatrists because there are 10 patients in this study suffering from psychiatric problems), (69%) of those who were referred were treated completely, (8.3%) had complications and (22.7%) refused the referral and went to home immediately after the symptoms subsided but before discharge by the doctor so they were not follow after that. No previous study reported in this aspect.
All investigations were performed: Urine for hair dye was found positive in (36%) of the patients. The study of Musa [16] showed (58%) were +ve. The same happened in other investigations which were requested to complete evaluation of the patient such as ultrasound, chest X-ray, ECG, renal function test, liver function test and complete hemogram serum electrolyte, urine analysis. Some of the patients were investigated for other investigations according to the situation (done to 5.5% of patients, like neck x-ray in patients who had angioneoratic edema because this is the precipitating factor for chest infection, blood film for malaria for patients who have fever.
The treatment as shown in [Figure 1], intravenous fluid in (94.5%), because PPD causes hypersensitivity and anaphylactic shock. Antihistamine was given to (95.5%) of cases and hydrocortisone to (97.5%). This treatment enforces diuresis in PPD intoxicated patients and thus prevents angioneuretic edema and renal failure. They observed that used of steroids with antihistamine and adrenaline prevent edema formation and occurrence of acute renal failure. Furthermore benzyl penicillin was given for about (86.5%) to prevent infection because those patients are susceptible to develop upper respiratory tract infection.
Medical treatment was satisfactory for (43.5%) of patient. This is consistent with Bariema [9] in which (57%) of the intoxicated patients were managed by medical treatment only.
Surgical treatment which was done included: Gastric lavage to wash out the PPD from stomach that ingested by the poisoned. NG tube done to (28.5%) of patients. Tracheostomy for (18%) of patients coming complaining of difficulty in breathing. Dialysis was done for (20%) of cases while Hamdouk [11] reported (65.2%) of patient were managed by dialysis.
In this study respiratory problems accounted for about (22.5%), in (20.5%) of patients the complication was renal failure. Cardiac problems occurred in about (1%), compared with Bariema [9] who reported that (21%) of patients with PPD toxicity died as a result of the same causes as in this study. This matches with that reported in literature which proved that death due to asphyxia dramatically was reduced by emergency tracheostomy. Liver problems occur in (0.5%).
The outcome of this study showed that case fatality rate was (3.5%). Comparably this case fatality rate is less than that reported by Osman [10] which was (33.3%). Hamdouk [11] reported a case fatality rate of (11.9%). Dawoud [17] reported a case fatality rate of (9.5%) this was explained by the success of treatment, which was tried as a method of detoxification and due to early arrival of poisoned patients to the hospital.
The causes of death in this study were respiratory obstruction (71.4% of deaths) and renal failure (28.6% of deaths). In this study, it was found that all deaths were females (seven patients). Three of them at the age 1-10 years, two patients were in the age group 11-20 years, one patient aged 21-30 years and the last one in 41-50 years). Yagi et al.[6] reported that the mortality rate was high among females.
The mortality rate was decreased due to the fact that patients came immediately to hospital and due to improvements in modalities of management.
| Conclusion and Recommendations | |  |
- Hair dye poisoning is a major cause of intoxication in Sudan and the intention to commit suicide is the main cause of PPD poisoning.
- There is relationship between:
- Presence of psychological problems, age, marital status and type of intoxication.
- Type of intoxication with the gender and route of administration.
- Outcome with gender, age and route of administration.
- The most common clinical presentation is ingestion of dye (85.5%) tachycardia (58%), tachypnea (31.5%), vomiting (31.0%), angioneuratic edema (22.5%) and abdominal pain (22.0%).
- Acute renal failure still consider as the major complication (20.5%).
- The medical treatment and emergency tracheostomy improve the outcome of intoxicated patients.
- The common complications of hair dye were respiratory obstruction (22.5%) and acute renal failure (20.5%).
- The common causes of death in hair dye intoxication were respiratory obstruction (71.4%) and renal failure (28.6%).
- Immediate arrival to hospital is the cause of low fatality rate (3.5%). And therefore we recommend the followings:
- Health education about the dangers of hair dye poisoning and complications is important.
- To prohibit availability of hair dye in common places without any restrictions.
- Trades in hair dye without permission from responsible authorities must be discussed within the legislations.
- Organizing field works and seminars about hair dye poisoning on the national level.
- Provision of equipment requirement for intubations in all hospital and health centers on national levels.
- Campaigns of extensive information, public education and collaboration of different health authorities to arise the public awareness of PPD related hazards are urgently needed. Mass media and social workers should help in this program.
- The use of henna mixed with PPD should be discouraged or formulation with concentration less than 6% (allowed concentration according to the European standards can replace the available dye to be mixed with henna.
- The use of PPD freely with pregnancy should be prohibited as there is growing concern that fetus may be seriously affected (more study are required in this field).
- Psychological support to the patients to avoid future events especially suicidal attempt.
- Further studies on hair dye poisoning especially the prevalence in whole country.
| Acknowledgment | |  |
We express our sincere thanks to Ahfad University for women with special regards to Professor Ali Billy.
We highly appreciate the support of statistical Department in ENT unit in Khartoum Hospital, Dr. Abd elrahman Elafshy, Emad and Egbal (in computer work).
| References | |  |
| 1. | Mathiharan K, Pantaik AK. Modis Medical Jurisprudence and Toxicology. 23 edition. Lexis Nexis Butterworth Rakmo Press, New Delhi; 2005. p. 3-12 
|
| 2. | Information unit statistical report, Khartoum Teaching Hospital - ENT department 2008. 
|
| 3. | Suliman SM, Homeida M, Aboud OI. Paraphenylenediamine induced acute tubular necrosis following hair dye ingestion. Hum Toxicol 1983;2:633-5. 
[PUBMED] |
| 4. | Elgamel AA, A/Kareim EI. Prevalence of suicidal and criminal cases caused by PPD in Sudan, forensic medicine (medical negligence and forensic science). Eithar Prints and Press, Khartoum, Sudan; 2006. p. 97-81. 
|
| 5. | El-Ansary EH, Ahmed ME, Clague HW. Systemic toxicity of para-phenylenediamine. Lancet 1983;1:1341. 
[PUBMED] |
| 6. | Yagi H, el Hind AM, Khalil SI. Acute poisoning from hair dye. East Afr Med J 1991;68:404-11. 
|
| 7. | Mathur AK, Gupta BN, Narang S, Singh S, Mathur N, Singh A, et al. Biochemical and histopathological changes following dermal exposure to paraphenylene diamine in guinea pigs. J Appl Toxicol 1990;10:383-6. 
|
| 8. | Charra B. Systemic toxicity of PPD; Work of Sixth Congress of the Arab Society of Nephrology and Renal Transplantation. February 21-24, Marakesh Marroco. 2000. 
|
| 9. | Bariema E. Incidence of tracheostomy compared to conservative management of hair dye poisoning. MD Thesis SMSB. Vol. 3. MD Thesis Sudanese Medical Specialties Board 2002. 
|
| 10. | Osman M. Acute poisoning with hair dye containing PPD, the Gezera experience. J Arab Med Spec 2001; (80-1). 
|
| 11. | Hamdouk M . Acute hair dye systemic toxicity. MD Thesis Shuffled University 2001. 
|
| 12. | Sir Hashim M, Hamza YO, Yahia B, Khogali FM, Sulieman GI. Poisoning from henna dye and para-phenylenediamine mixtures in children in Khartoum. Ann Trop Paediatr 1992;12:3-6. 
|
| 13. | Hsin I. Anti-dotes, medical toxicology, clinical toxicology. J Toxicol 2000;38:21-8. 
|
| 14. | Burentt CM, Corbetl DF. The chemistry and toxicology of hair dye. In: Drill UA, Lazar. Cutaneous Toxicity. New York: Academic Press; 1977. p. 203-21. 
|
| 15. | Thirtle JR. Phenylene diamine and toluene diamine. In: Kirk RE, Othmer DF, editors. Encyclopedia of Chemical Technology. Vol. 15. New York: John Wily and Sons; 1968. p. 216-24. 
|
| 16. | Musa SM. Paraohenylenediamine (Hair dye) poisoning-case study in Ear, Nose and Throat, Khartoum Teaching Hospital, research submitted in partial fulfillment fpr the requirement for the M.B.B.S Ahfad University for Women School of Medicine, Sudan; 2003. 
|
| 17. | Dawoud AS. PPD poisoning at Khartoum teaching hospital and Bahri Renal Center, Case Symposium; 2007. 
|
[Figure 1]
[Table 1], [Table 2]
|