|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2016 | Volume
: 11
| Issue : 4 | Page : 113-118 |
|
Prevalence of diabetes mellitus in a tertiary health institution in Gombe Metropolis, Nigeria
Mela Danjin1, Nafisa Umar Usman1, Danladi Adamu2
1 Department of Anatomy and Physiology, College of Nursing and Midwifery, Gombe, Gombe State, Nigeria
2 Department of Community Health Nursing, College of Nursing and Midwifery, Gombe, Gombe State, Nigeria
| Date of Web Publication | 16-Mar-2017 |
Correspondence Address:
Mela Danjin
Department of Anatomy and Physiology, College of Nursing and Midwifery, Gombe, Gombe State
Nigeria
  | Check |
DOI: 10.4103/1858-5000.202357 
Aim: This study was aimed at determining the prevalence of diabetes mellitus (DM) among adult patients attending Specialist Hospital Gombe, Northern Nigeria. Materials and Methods: A 5-year (2010–2014) retrospective descriptive survey of cases of DM was conducted, using hospital record retrieved from the Record Department of Specialist Hospital Gombe. Diagnosed adult cases of DM were carefully identified and sorted from the general outpatient department morbidity register. Relevant data were then harvested on a specially designed data collection template. Results: A total of 40,083 medical cases were counted, out of which 2069 cases of DM were identified. This implies an overall prevalence rate of 5.16%. However, the yearly prevalence of the disease revealed as high as 12.55% in the year 2012 and a least value of 1.22% in the year 2010. Age-specific case count of the disease was found to be highest (1288; 62.25%) within the uppermost age range of 65–75, while the lowest age range of 25–34 was least affected (33, 1.60%). Overall, more females (1491; 72.06%) suffered from the disease than males (578, 27.94%). The sex difference was found to be significant (χ2 = 449.15521,P= 0.000). Furthermore, the case burden of the disease was found to be significantly (χ2 = 39.02524,P= 0.000) highest among individuals living in urban areas, 663 (80.38%) than those living in rural areas, 406 (19.62%). Conclusion: The disproportionately high case burdens of DM among females, urban dwellers, and the aged are useful information for the design of targeted diabetes prevention programs by government and other stakeholders. Keywords: Adult patients, diabetes, prevalence, retrospective
How to cite this article:
Danjin M, Usman NU, Adamu D. Prevalence of diabetes mellitus in a tertiary health institution in Gombe Metropolis, Nigeria. Sudan Med Monit 2016;11:113-8 |
| Introduction | |  |
The term “diabetes” or “to pass through” was first used in 230 BC by the Greek Apollonius of Memphis. The term “mellitus” or “from honey” was added by Briton John Rolle in the late 1700s to separate the condition from diabetes insipidus, which is also associated with frequent urination.[1] Diabetes mellitus (DM) often simply referred to as diabetes is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin or because the cells do not respond to the insulin that is produced.[2] This high blood sugar produces classical symptoms of polyuria (frequency urination), polydipsia (increase thirst), and polyphagia (increased hunger).
DM is one of the most common chronic diseases in nearly all countries and continues to increase in numbers and significance as changing lifestyles lead to reduced physical activity and increased obesity. Estimates of the current and future burden of diabetes are important to allocate community and health resources and to emphasize the role of lifestyle and encourage measures to counteract trends for increasing prevalence. The world prevalence of diabetes among adults (aged 20–79 years) was 6.4%, affecting 285 million adults, in 2010, and will increase to 7.7% and 439 million adults by 2030. Between 2010 and 2030, there will be a 69% increase in numbers of adults with diabetes in developing countries and a 20% increase in developed countries.[3]
Currently, around 20 million people in Africa have diabetes – a prevalence of 4.9% – but over the next two decades, the number of people with diabetes is expected to more than double, threatening many of the development gains Africa has achieved.[4] Based on the 2013 International Diabetes Federation (IDF) global diabetes scorecard, raw national diabetes prevalence for Nigeria was estimated at 4.99%. The national figure of some other African countries includes 3.58% for Kenya, 3.93% for Guinea, 3.35% for Ghana, and 1.55% for The Gambia. Ethiopia has 4.36%, DR Congo 5.37%, Republic of Congo 5.48%, and Cameroun 4.88%. Others include Rwanda 4.38%, South Africa 8.27%, Senegal 3.24%, Tanzania 7.80%, Zambia 3.16%, and Zimbabwe with the highest (8.83%). The average score for Europe was put at 8.50% with Turkey having the highest score of 14.58% and lowest (2.64%) recorded by Armenia. The USA had an average score of 10.90%.[4]
DM is often associated with a high disease burden in developing countries such as Nigeria. In the early nineties, not much was known about DM in Nigeria, and traditionally, people related DM to “curses” or “hexes” and diagnosis was made based on blood or urinary tests for glucose. A systematic review by Ogbera and Ekpebegh concluded that the current prevalence of DM in Nigeria is not known, but guestimates may likely be in the region of 8%–10%.[5] Studies from different parts of Nigeria revealed varying prevalence or incidence figures irrespective of geographical locations. In Port Harcourt, Nwafor and Owhoji reported DM prevalence of as high as 23.4% among the high socioeconomic group and 16% among the low socioeconomic group.[6] From Abeokuta, Southwestern Nigeria, an overall prevalence rate of 14.8% was reported.[7] When segregated by age group, an increasing trend from 2.9% in the age group of 18–27 years to a peak of 21.1% in the age group of 48–57 years was observed. Omorogiuwa et al. in a survey carried out on a university community, Ekpoma, Edo State, Southern Nigeria, reported an overall prevalence of as high as 9.8%.[8] In Umudike, Abia State, Southeastern Nigeria, in a study among adult Nigerians 18 years and above, a prevalence rate of 3.0% with higher rates reported among females (3.6%) than males (2.3%) was published.[9] In another study among adults aged 18 years and above residing in five rural communities in Edo State, an overall crude prevalence of 4.6% with sex differences (males 1.9%, females 5.8%, P = 0.012) was reported.[10] Overall prevalence of as high as 10.5% with male and female rates of 9.6% and 11.2%, respectively, was reported in Uyo, South-southern Nigeria.[11]
In Northern Nigeria, prevalence and incidence surveys also indicate varying figures. A 5-year (2001–2005) retrospective study of hospital records in Katsina showed more males (201 [71.53%]) suffered from the disease than females (80 [28.47%]).[12] The study also revealed a steep rising age group trend, from the lowest proportion (0.71%) among 21–30 years range to the highest (39.86%) among 61–70 years age group. However, the yearly trend was remarkably irregular with an initial sharp rise from 15.65% in 2001 to 25.27% in 2002 and thereafter came down to 14.23% in 2005. More urban (82.56%) than rural (17.44%) dwellers were affected by the disease. Another prevalence study in Dakace village, a semi-urban community near Zaria in Northern Nigeria, reported 2.0% overall diabetes prevalence.[13] In small size prevalence survey among rural Fulanis in Sokoto, Northern Nigeria, very low prevalence rate (0.8%) was reported although the same study yielded very high impaired fasting glycemia and impaired glucose tolerance rates of 6.9% and 8%, respectively.[14] In the 1990s, Bakari et al. reported very low (1.6%) DM prevalence in some suburban communities in Kaduna State.[15]
| Materials and Methods | |  |
Study setting
This survey was conducted at the State Specialist Hospital domiciled within Gombe Metropolis which is the state capital of Gombe State in Northern Nigeria. The metropolis lies between latitude 110 81 N and 110 241 N, longitude 110 021 E and 110 181 E. The temperature averages 30°C with an annual rainfall of 52 cm. The hospital is the only state government-owned tertiary health facility that is meant to cater for referral cases from other secondary (general hospitals) and primary health facilities scattered over the 11 local governments of the state. Hence, to a large extent, the hospital patient demographics may be a fair reflection of the entire state. Some of the specialist units or departments include general outpatient department which serves as a filter where all cases are first seen, pediatrics department, a standard laboratory, eye clinic, dental clinic, obstetrics and gynecology department, health records department, etc. Based on the Nigerian National Population Commission Census 2006 figures projected to 2014, Gombe State has an estimated total population of about 3 million (3,028,459) at an annual growth rate of 3.2% (http://www.population.gov.ng/pop_figure.pdf).[16] The metropolis has a projected population of 344, 804 inhabitants. Two major seasons are experienced in Gombe; rainy season (April to October) and dry season (November to March).
Study design
A retrospective descriptive survey of DM was conducted in Specialist Hospital Gombe where the records in the health record department of the hospital were retrieved, reviewed, and analyzed with the aim of determining overall prevalence of the disease as well as characterizing trends and patterns of its distribution based on some selected demographics of the patients.
Target population
Inclusion criteria
To be included in the survey, a case record must be that of an adult patient seen in the outpatient department of Specialist Hospital Gombe with medical diagnosis of DM within the period of 2010–2014 and must be within the age range of 25–74 years (well over 90% of all DM cases retrieved). The record of all other medical cases seen within the same period qualified for the overall all-cases count. Although this study could not segregate DM cases by type, extent data from other African countries and Nigeria reveal that about 90% of cases are type 2 DM (T2DM) while T1DM ranges between 5.7% and 10.0% with the remaining 0.0% to 4.3% being gestational DM.[17],[18],[19]
Exclusion criteria
A case record will be excluded especially if patient was seen before the year 2010 or after the year 2014. Only very few diagnosed DM cases fell outside the age range of 25 and 75 years. For the general, all-cases count cases outside the study period (2010–2014) were excluded from the study.
Data collection
The relevant hospital records of all medical cases including DM in the State Specialist Hospital Gombe, from 2010 to 2014, were carefully sorted with the aim of investigating the prevalence of the DM in Gombe. A total of 40,083 medical cases were counted, out of which 2069 cases of DM were identified. The key variables of which data were collected include number of all medical cases seen, number of cases of DM seen, age range, sex, place of residence, month, and year.
A structured pro forma with columns under the aforementioned key variable headings was designed and used for the data collection on all identified diagnosed DM cases.
Data analysis
The raw data were entered on Microsoft Excel spreadsheet for preliminary analysis. Thereafter, it was exported to Epi Info 7 (CDC, Atlanta, GA, USA, 2011) for further analysis. Data were presented as frequency tables, bar charts, and graphs. Associations were tested using Chi-square within 95% confidence interval (CI).
Ethical consideration
Ethical clearance for this work was obtained from the Research and Ethics Committee (REECOM) of College of Nursing and Midwifery Gombe, while consent of relevant authorities of the hospital was properly secured.
| Results | |  |
The results of this study showed a total number of all medical cases seen in the hospital within the study period (2010–2014) as 40,083, out of which 2069 were cases of DM [Table 1]. This represented an overall DM prevalence of 5.16%. The yearly trend of DM prevalence is also shown in [Table 1], 2010 (1.22%; 76/6212), 2011 (3.96%; 226/5704), 2012 (12.55%; 1219/9710), 2013 (3.33%; 431/12944), and 2014 (2.12; 117/5513). [Table 2] depicts DM cases seen within the study period according to age group as 25–34 (33; 1.60%), 35–44 (127; 6.14%), 45–54 (162; 7.83%), 55–64 (459; 22.18%), and 65–75 (1288; 62.25%). The increases in the disease burden with age were significant (χ2 = 24.5502, P = 0.000). In [Table 3], sex distribution of DM cases within the study period was shown with significant (χ2 = 449.15521, P = 0.000) female majority, male (578; 27.94%) and female (1491; 72.06%). [Figure 1] displays the cumulative monthly trend of the 2069 DM cases identified within the 5-year study period (2010–2014). The lowest case count (54) was in March, while the three peaks were recorded in the months of July (141), October (428), and December (560). [Table 4] shows DM case burden according to place of residence, in which 80.38% (1663/2069) of the patients domiciled in urban areas while the remaining 19.62% (406/2069) resided in rural areas. This variation was quite significant with χ2 = 39.02524, P = 0.000.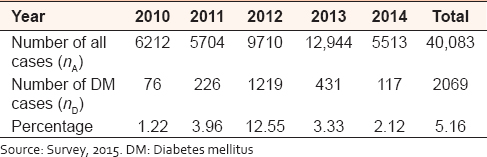 | Table 1: Yearly count of all cases versus case count and prevalence of diabetes mellitus in Specialist Hospital Gombe (2010-2014)
Click here to view |
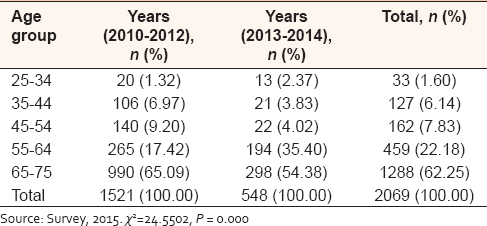 | Table 2: Diabetes mellitus cases by age group in Specialist Hospital Gombe (2010-2014)
Click here to view |
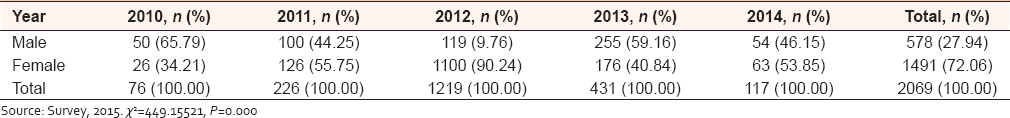 | Table 3: Yearly distribution of diabetes mellitus cases by sex in Specialist Hospital Gombe (2010-2014)
Click here to view |
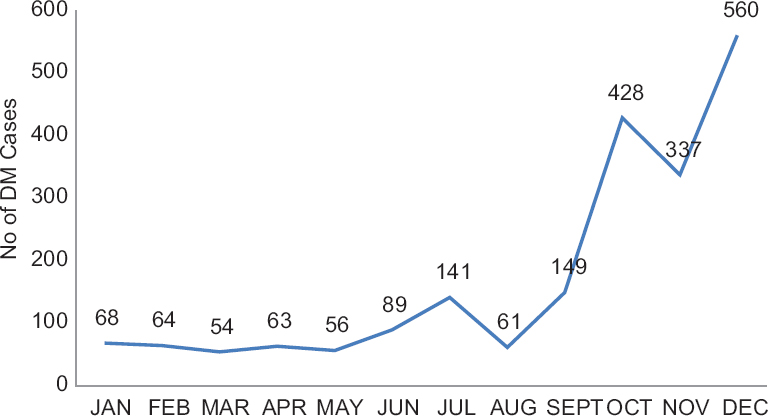 | Figure 1: Cumulative monthly trend of diabetes mellitus case count in Specialist Hospital Gombe (2010–2014). Survey, 2015
Click here to view |
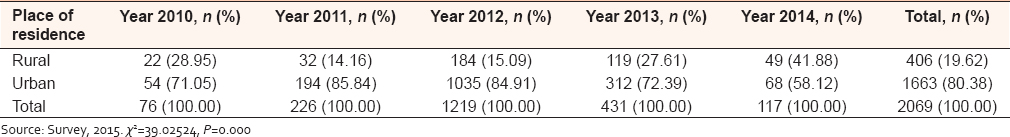 | Table 4: Diabetes mellitus occurrence by residence in Specialist Hospital Gombe (2010-2014)
Click here to view |
| Discussion | |  |
Overall and yearly prevalence of diabetes mellitus
With a computed overall DM prevalence of 5.16% and a census population figure of Gombe state (3,028,459) cited in the study setting, we can say that there is an estimated population of 156,269 people in Gombe State that are suffering from the disease [Table 1]. This rate appears to be on the high side compared to the Nigerian national prevalence rate of 4.99% according to the IDF.[4] When determined according to individual years covered in this study, there was a steep rise from an initial lowest rate of 1.22% in the year 2010–3.96% in 2011. This rising trend continued to a peak of 12.55% in the year 2012. Thereafter, it nosedived to 3.33% in the year 2013 and finally to 2.12% in the year 2014. This picture contrasts with findings at global, regional, and national levels where both developed and developing countries are experiencing an almost linear rising trend in the prevalence of diabetes, cardiovascular diseases, and other noncommunicable diseases.[3],[4],[5],[20] However, on the prevalence of diabetes in Nigeria, Oputa and Chinyere state in a review that, “the diabetes prevalence of 4.9% has more than doubled when compared with the 2.2% prevalence of the Professor Akinkugbe-led National Survey Report of 1997.”[21] Hence, the fluctuating trend observed in this study needs to be further substantiated by other more rigorous studies in the study area.
Age pattern of diabetes mellitus occurrence
When stratified by age group, this study established a consistently rising pattern of DM burden with age, in which the oldest age group (65–75) was responsible for 62.25% of cases, while the lowest age rung (25–34) accounted for the smallest percentage (1.60%) of DM cases. The association between age and DM occurrence was found to be quite significant (χ2 = 24.5502, P = 0.000). This concurs with findings of other studies from different parts of the world and within Nigeria.[18] In a study on type 2 diabetes and its correlates among adults in Bangladesh, respondents within the age group of 55–59 years had higher odds of having diabetes (odds ratios = 2.37, 95% CI: 1.76–3.21) than the age group of 35–39 years.[22] In a study in Uyo, Southern Nigeria, subjects in the highest age group in the study (46–60) were about twice more likely to have diabetes than all the others in the lower age groups.[11] In another DM prevalence study in Port Harcourt, Southern Nigeria, aging was also found to be associated with type 2 diabetes.[17]
Sex distribution of diabetes mellitus cases
When segregated by sex, this study showed that more females were affected than males in a ratio of 2.58:1 (72.06%/27.94%) [Table 3]. This sex differential was found to be quite significant (χ2 = 449.15521, P = 0.000). This agrees with several other studies that revealed higher female ratio in different proportions. Findings from Port Harcourt by Tamunopriye and Iroro showed 70% females and 30% males with a male-female ratio of 1:2.3.[23] Uloko et al. reported from a multicenter study in Nigeria where out of a total of 531 DM patients, 209 (39.4%) were males and 322 (60.6%) were females.[24] From Enugu, Southern Nigeria, Chukwu et al. reported a higher proportion or cases of DM among females (56.0%) than the males (44.0%).[25] However, there were reports of higher male prevalence even Nigeria. In a hospital-based retrospective survey in Katsina, Northern Nigeria, Suleiman and Abdulkarim recorded more males that suffered from the diseases (201, 71.53%) than females (80, 28.47%).[12] A report from Abeokuta, Southern Nigeria, states that “male subjects had higher prevalence of diabetes (1.85%) than females with 1.19% prevalence.”[7] Omorogiuwa et al. also reported higher male prevalence ratio, “the male/female diabetic ratio were 1.4:1 and 1.3:1 for senior staff and junior staff, respectively,” among university staff in Ekpoma, Southern Nigeria.[8] A sedentary lifestyle of women in this part of the country could be a possible explanation to our findings of a feminine preponderance of DM case burden. Men are adjudged to be more physically active than women and this probably could enhance insulin sensitivity in the men than women. Ekpenyong et al. and Nyenwe et al. found physical inactivity to be significantly associated with the incidence of diabetes in their study.[11],[17] The male preponderance in other studies may not reflect the real situation because the pattern of hospital medical admissions may also need to be examined in such studies. The male bias may therefore be related to cultural, geographic, and socioeconomic factors rather than mere gender-related prevalence of DM.[26]
Monthly trend of diabetes mellitus cases
Cumulative monthly trend of cases within the study period (2010–2014) exhibited an overall rising pattern of DM case occurrence from January to December. Three remarkable peaks were recorded in July (141 cases), October (428 cases), and December (560 cases), while two troughs were observed in August (61 cases) and November (337 cases). October and December peaks were more pronounced, suggesting a seasonal predilection of DM case occurrence toward the end of raining season and the peak of harvest and festive period of the year. This finding has been corroborated by others. A seasonality of type 1 diabetes has been reported in Tanzania, with most cases presenting between August and November.[27] From the University of Benin Teaching Hospital, Benin City, Nigeria, Edo et al. reported peak cases in July and December, with the highest in December.[28] In a 6-year study on “seasonal incidence of DM in Tropical Africa,” the peak months of presentation were August through to November, with the greatest number of patients presenting in September.[29] In a slightly varied scenario, Tamunopriye and Iroro from Port Harcourt reported in their study that, “67% of patients were diagnosed in the rainy season.”[23]
Prevalence of diabetes mellitus by place of residence
This study recorded more urban (1663, 80.38%) than rural (406, 19.62%) cases of DM. The differences were statistically significant (χ2 = 39.02524, P = 0.000). This agrees with majority of findings at various levels. A retrospective hospital-based study in Katsina, Northern Nigeria, also established an overwhelmingly higher case burden in the urban (82.56%) than rural (17.44%) areas.[12] In Lagos, Southwestern Nigeria, Oguoma et al. also reported higher urban (5.4%) than rural (1.8%) prevalence figures of DM.[30] Moreover, the explanation to this discrepancy has consistently been fast changing lifestyle due to the overwhelming influence of westernization cum urbanization in most developing countries. Urbanization tends to decrease physical activity as very little physical activity is required for daily living, whereas rural populations rely on foot walk as transportation means and often have intense agricultural activities as their main occupation.[14]
| Conclusion | |  |
The findings of this study show clearly that the prevalence of DM in the study area is consistent with the national prevalence according to the IDF. However, the yearly trend which exhibited a sharp rise in the year 2012 and a nosedive thereafter might be indicative of some dramatic progress in the control efforts occasioned by massive media and community sensitization programs on appropriate lifestyle modifications. In any case, the disproportionate distribution of the disease burden with obvious bias toward females, urban dwellers, and the aged is the useful information for the design of more targeted prevention programs by government and other stakeholders.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Leonid P. Principles of Diabetes Mellitus. 2 nd ed. New York: Springer; 2009. p. 3.  |
| 2. | Gardener DG, Dolores S. Greenspan's Basic & Clinical Endocrinology. 9 th ed., Ch. 17. New York: McGraw-Hill Medical; 2011. p. 880. ISBN 0-07-162243-8.  |
| 3. | Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4-14.  |
| 4. | International Diabetes Federation. Global diabetes scorecard tracking progress for action. Brussels: International Diabetes Federation; 2014. p. 5-24.  |
| 5. | |
| 6. | Nwafor A, Owhoji A. Prevalence of diabetes mellitus among Nigerians in Port Harcourt correlates with socio-economic status. J Appl Sci Environ Manage 2001;5:75-7.  |
| 7. | Akinjinmi AA, Adeyooye OA, Akingbade OA, Okerentugba PO. Prevalence of diabetes mellitus in Abeokuta, Ogun State, Nigeria. Researcher 2014;6:73-5. Available from: http://www.sciencepub.net/researcher. 10. [Last accessed 2015 Oct 05].  |
| 8. | Omorogiuwa A, Oaikhena GA, Okioya P, Akubueze D, Owobu E, Enahoro I, et al. Diabetes mellitus: Prevalence amongst university staff in Southern Nigeria and attitude towards routine glycemic/glucosuric checkup. Int J Biomed Health Sci 2010;6:25-9.  |
| 9. | Ejike CE, Uka NK, Nwachukwu SO. Diabetes and pre-diabetes in adult Nigerians: Prevalence, and correlations of blood glucose concentrations with measures of obesity. Afr J Biochem Res 2015;9:55-60.  |
| 10. | Isara AR, Okundia PO. The burden of hypertension and diabetes mellitus in rural communities in southern Nigeria. Pan Afr Med J 2015;20:103.  |
| 11. | Ekpenyong CE, Akpan UP, Ibu JO, Nyebuk DE. Gender and age specific prevalence and associated risk factors of type 2 diabetes mellitus in Uyo Metropolis, South Eastern Nigeria. Diabetol Croat 2012;41:17-28.  |
| 12. | Suleiman M, Abdulkarim B. Incidence of diabetes mellitus at the Katsina General Hospital, Katsina State, Nigeria. Appl Sci Rep 2015;11:29-32. Available from: http://www.pscipub.com. [Last accessed on 2015 Oct 06].  |
| 13. | Dahiru T, Jibo A, Hassan AA, Mande AT. Prevalence of diabetes in a semi-urban community in Northern Nigeria. Niger J Med 2008;17:414-6.  |
| 14. | Sabir A, Ohwovoriole A, Isezuo S, Fasanmade O, Abubakar S, Iwuala S. Type 2 diabetes mellitus and its risk factors among the rural Fulanis of Northern Nigeria. Ann Afr Med 2013;12:217-22.  [Full text] [Full text] |
| 15. | Bakari AG, Onyemelukwe GC, Sani BG, Hassan SS, Aliyu TM. Prevalence of diabetes in suburban Northern Nigeria: Results of a public screening survey. Diabetes Int 1999;9:59-60.  |
| 16. | |
| 17. | Nyenwe EA, Odia OJ, Ihekwaba AE, Ojule A, Babatunde S. Type 2 diabetes in adult Nigerians: A study of its prevalence and risk factors in Port Harcourt, Nigeria. Diabetes Res Clin Pract 2003;62:177-85.  |
| 18. | Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: A review of current trends. Oman Med J 2012;27:269-73.  |
| 19. | Hall V, Thomsen RW, Henriksen O, Lohse N. Diabetes in Sub Saharan Africa 1999-2011: Epidemiology and public health implications. A systematic review. BMC Public Health 2011;11:564.  |
| 20. | Jayawardena R, Ranasinghe P, Byrne NM, Soares MJ, Katulanda P, Hills AP Prevalence and trends of the diabetes epidemic in South Asia: A systematic review and meta-analysis. BMC Public Health 2012;12:380.  |
| 21. | Oputa RN, Chinenye S. Diabetes mellitus: A global epidemic with potential solutions. Afr J Diabetes Med 2012;20:33-5.  |
| 22. | Chowdhury MA, Uddin MJ, Khan HM, Haque MR. Type 2 diabetes and its correlates among adults in Bangladesh: A population based study. BMC Public Health 2015;15:1070.  |
| 23. | Tamunopriye J, Iroro Y. The pattern of presentation and trends of childhood diabetes mellitus in Port Harcourt, Southern Nigeria. Br J Med Med Res 2015;5:247-53.  |
| 24. | Uloko AE, Ofoegbu EN, Chinenye S, Fasanmade OA, Fasanmade AA, Ogbera AO, et al. Profile of Nigerians with diabetes mellitus – Diabcare Nigeria study group (2008): Results of a multicenter study. Indian J Endocrinol Metab 2012;16:558-64.  |
| 25. | Chukwu BN, Ezebuiro VO, Samuel ES, Nwachukwu KC. Gender differential in the incidence of diabetes mellitus among the patients in Udi Local Government Area of Enugu State, Nigeria. Mediterr J Soc Sci 2013;4:131-8.  |
| 26. | Abdulkadir J. Malnutrition-related diabetes mellitus in Africa. Int J Diabetes Dev Ctries 1993;13:22-8.  |
| 27. | Mbanya JC, Ramiaya K. Disease and mortality in Sub-Saharan Africa. Diabetes Mellitus. 2 nd ed., Ch. 19. Washington, D.C.: The World Bank; 2006.  |
| 28. | Edo AE, Edo GO, Ezeani IU. Risk factors, ulcer grade and management outcome of diabetic foot ulcers in a Tropical Tertiary Care Hospital. Niger Med J 2013;54:59-63.  [ PUBMED] [Full text] |
| 29. | McLarty DG, Yusafali A, Swai AB. Seasonal incidence of diabetes mellitus in tropical Africa. Diabet Med 1989;6:762-5.  |
| 30. | Oguoma VM, Nwose EU, Skinner TC, Digban KA, Onyia IC, Richards RS, et al. Erratum to: Prevalence of cardiovascular disease risk factors among a Nigerian adult population: Relationship with income level and accessibility to CVD risks screening. BMC Public Health 2015;15:891.  |
[Figure 1]
[Table 1], [Table 2], [Table 3], [Table 4]
|