|
 
 |
| CASE REPORT |
|
| Year : 2014 | Volume
: 2
| Issue : 2 | Page : 74-77 |
|
Absence of the musculocutaneous nerve in the right upper extremity: An unusual anatomical variation with potential clinical relevance
Gabriel Godson Akunna, Ogugua Augustine Egwu, Joseph A Nwafor, Obinna Uchewa
Department of Anatomy, Federal University, Ndufu Alike Ikwo, Ebonyi, Nigeria
| Date of Web Publication | 23-Mar-2015 |
Correspondence Address:
Ogugua Augustine Egwu
Department of Anatomy, Faculty of Basic Medical Sciences, Federal University Ndufu Alike Ikwo, Ebonyi
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2315-7992.153821

Neural variations of the brachium constitute a significant anatomical and clinical entity. Variations in median and musculocutaneous nerves are common, whereas the absence of the musculocutaneous nerve (McN) is very rare. The present report is on the absence of the McN observed in the right upper extremity of a middle-aged Nigerian male cadaver during routine educational dissection in the Department of Anatomy, Ebonyi State University, Nigeria. We observed three separate branches from the median nerve innervating the coracobrachialis muscle, biceps brachii, and brachialis muscles. The muscles that are usually innervated by the McN were innervated by the median nerve in this case. Also, the longest and more distal of these branches (branch to brachialis muscles) pass between the biceps and the brachialis muscle. In the cubital fossa, it lies at the lateral margin of the biceps tendon where it continues as the lateral cutaneous nerve of the forearm. The presence of this anomaly should be considered during surgical interventions and clinical investigations of the arm as this may help plan a surgical procedure in the region of axilla and the arm, traumatology of the shoulder joint, and plastic and reconstructive repair. Keywords: Brachial plexus, median nerve, musculocutaneous nerve (McN), variations
How to cite this article:
Akunna GG, Egwu OA, Nwafor JA, Uchewa O. Absence of the musculocutaneous nerve in the right upper extremity: An unusual anatomical variation with potential clinical relevance. Ann Bioanthropol 2014;2:74-7 |
How to cite this URL:
Akunna GG, Egwu OA, Nwafor JA, Uchewa O. Absence of the musculocutaneous nerve in the right upper extremity: An unusual anatomical variation with potential clinical relevance. Ann Bioanthropol [serial online] 2014 [cited 2018 Sep 6];2:74-7. Available from: http://www.bioanthrojournal.org/text.asp?2014/2/2/74/153821 |
| Introduction | |  |
Variations of the brachial plexus and its terminal branches are common and have been severally documented. [1],[2],[3],[4],[5],[6],[7] They are found in around 13% of dissections on cadavers. Nerves of the brachial plexus are formed by the anterior primary rami of spinal nerves C5, C6, C7, C8, and T1, which may be joined by branches from the fourth cervical (C4) and second thoracic (T2) nerves. The fifth and sixth cervical roots (C5 and C6) join to form the upper trunk. The seventh cervical root continues as the middle trunk. The eighth cervical and the first thoracic (C8 and T1) roots bond to form the lower trunk. Each of these trunks divides into ventral and dorsal divisions. Ventral division of the lower trunk continues distally to form the medial cord. Dorsal divisions of the upper, middle, and lower trunk join to form the posterior cord. Ventral divisions of the upper and middle trunks join to form the lateral cord.
The median nerve, formed by the union of the terminal branch of the lateral (C5, C6, and C7) and medial (C8 and T1) cords of the brachial plexus, laterally enters the arm to the brachial artery. Near the insertion of coracobrachialis, it crosses in front of the artery (rarely behind) descending medially to it to the cubital fossa where it is posterior to the bicipital aponeurosis and anterior to the brachialis, separated by the latter from the elbow joint. It then descends to the forearm between the two heads of the pronator teres muscle. The median nerve does not give motor branches in the arm; however, it gives off vascular branches to the brachial artery and supplies articular branches to the elbow joint.
The musculocutaneous nerve (McN) is the nerve of the flexor/anterior compartment of the arm. It is the continuation of the lateral cord of the brachial plexus. It gives a branch to the shoulder joint and then pierces the coracobrachialis muscle and descends laterally between the biceps and the brachialis muscles and supplies all the muscles in the anterior (flexor) compartment of the arm. In the cubital fossa, it lies at the lateral margin of the biceps tendon where it continues as the lateral cutaneous nerve of the forearm.
The McN has frequent variations. It may run behind the coracobrachialis muscle or adhere to the median nerve for some distance and pass behind the biceps brachii muscle; some fibers of the median nerve may run in the McN; less frequently the median nerve sends a branch to the McN. [8],[9],[10] The presence of a communicating branch arising from the McN and joining the median nerve is more common than the presence of a communicating branch arising from the median nerve joining the McN.
The present report deals with a rare variation/absence of the McN.
| Case report | |  |
During an educational gross anatomy dissection of the right upper extremity of a middle-aged Nigerian male cadaver in the Department of Anatomy, Ebonyi State University, we observed an absence of the McN. This occurred after a routine dissection of 20 upper extremities in the gross anatomy laboratory. It was noted that the lateral cord, instead of giving rise to the McN, continued in its route as the lateral root of the median nerve even after sending fibers that initially appeared as the lateral root of the median nerve [Figure 1], [Figure 2], [Figure 3], [Figure 4] and [Figure 5]. However, three muscular branches were seen emerging from the "large" median nerve to the coracobrachialis muscle, biceps muscle, and the brachialis muscle.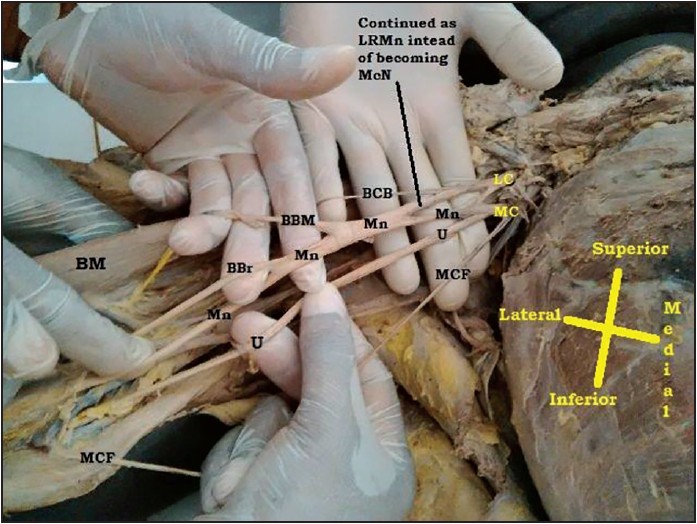 | Figure 1: Indicating the absence of musculocutaneous nerve. LC = Lateral cord, MC = Medial cord, Mn = Median nerve, U = Ulnar, BCB = Muscular branch to coracobrachialis, McF = Medial cutaneous nerve of forearm, BBM = Muscular branch to biceps brachii muscle, BBr = Branch for brachialis, BM = Biceps brachii muscle, LRMn = Lateral root of median nerve, MRMn = Medial root of median nerve, McN = Musculocutaneous nerve
Click here to view |
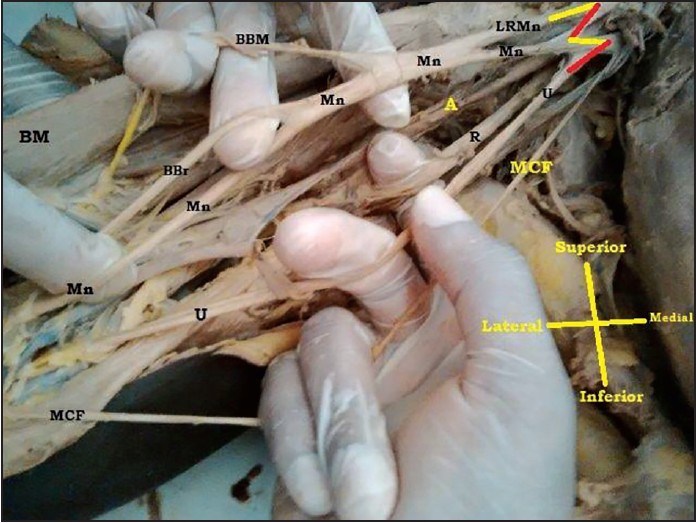 | Figure 2: Indicating the absence of musculocutaneous nerve. LC = Lateral cord, MC = Medial cord, Mn = Median nerve, U = Ulnar nerve, BCB = Muscular branch to coracobrachialis, R = Radial nerve, MCF = Medial cutaneous nerve of forearm, BBM = Muscular branch to biceps brachii muscle, A = Axillary nerve, BBr = Branch to brachialis, BM = Biceps brachii muscle, LRMn = Lateral root of median nerve
Click here to view |
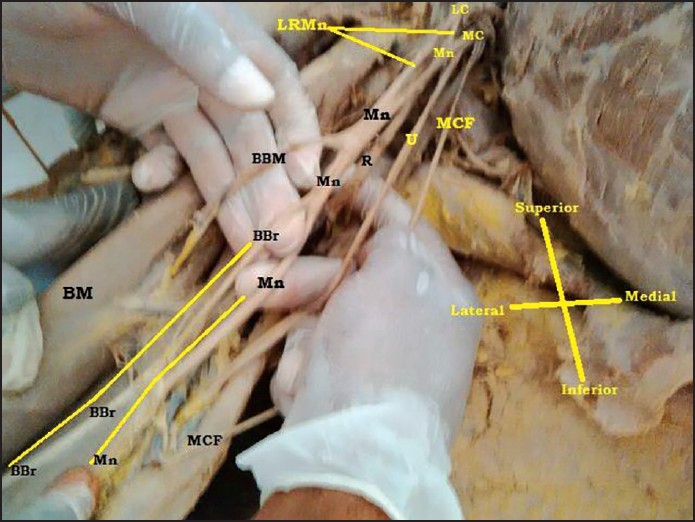 | Figure 3: Indicating the absence of musculocutaneous nerve. LC = Lateral cord, MC = Medial cord, Mn = Median nerve, U = Ulnar nerve, BCB = Muscular branch to coracobrachialis, R = Radial nerve, MCF = Medial cutaneous nerve of forearm, BBM = Muscular branch to biceps brachii muscle, A = Axillary nerve, BBr = Branch to Brachialis, BM = Biceps brachii muscle, LRMn = Lateral root of median nerve, MRMn = Medial root of median nerve
Click here to view |
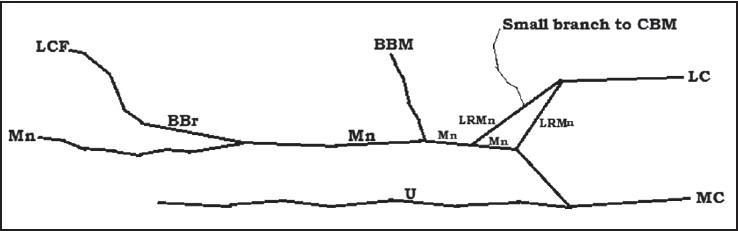 | Figure 4: Showing illustrations of our case. LC = Lateral cord, MC = Medial cord, Mn = Median nerve, U = Ulnar nerve, CBM = Muscular branch to coracobrachialis, R = Radial nerve, MCF = Medial cutaneous nerve of forearm, BBM = Muscular branch to biceps brachii muscle, BBr = Branch to brachialis, BM = Biceps brachii muscle, LRMn = Lateral root of median nerve
Click here to view |
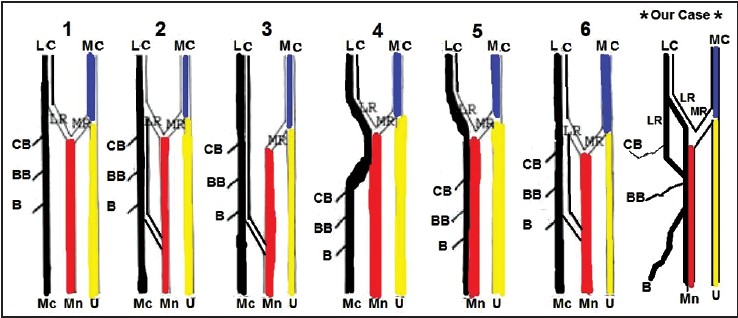 | Figure 5: Showing illustrations of six types of the musculocutaneous and the median nerves (I-VI) and our case (*). LC = Lateral cord, MC = Medial cord, MC = Musculocutaneous nerve, Mn = Median nerve, U = ulnar nerve, CB = Coracobrachialis muscle, BB = Biceps brachii muscle, B = Brachialis muscle, LR = Lateral root of median nerve, MR = Medial root of median nerve
Click here to view |
The most superior of the branches was to the coracobrachialis muscle. It was a small and short branch. Although it was small and fragile, we were able to preserve it during the dissection [Figure 1], [Figure 2], [Figure 3], [Figure 4] and [Figure 5].
The second and third branches (branches to the biceps and the brachialis muscles, respectively) from the median nerve were longer and larger. The branch to the brachialis muscle was the most distal and the longest. In the cubital fossa, this longer branch lies at the lateral margin of the biceps tendon where it continues as the lateral cutaneous nerve of the forearm [Figure 3].
| Discussion | |  |
The divisions and the route of the McN are of clinical significance. A more precise knowledge found in classical anatomical texts is paramount for clinical investigation and surgical treatment of peripheral nerve injury. [11],[12] The McN is usually the continuation of the lateral cord of the brachial plexus (C5, C6, and C7). It gives a branch to the shoulder joint and then pierces the coracobrachialis muscle (sometimes behind) and descends laterally between the biceps and the brachialis muscles, and supplies all the muscles in the anterior (flexor) compartment of the arm. In the cubital fossa, the McN lies at the lateral margin of the biceps tendon and continues as the lateral cutaneous nerve of the forearm after piercing the fascia just superior to the elbow.
In typical textbooks, the McN originates from the lateral cord of the brachial plexus and pierces the coracobrachialis muscle. However, there are several reports documenting variation in the communication between the McN and the median nerve. These communications have been considered as remnants from the phylogenic or comparative anatomical viewpoint. [4],[5]
In some cases, the McN originates from the posterior cord instead of the lateral cord. [6]
Occasionally, the lateral cord, without giving off the lateral root of the median nerve, passed through the coracobrachialis muscle and innervated the coracobrachialis, biceps brachii, and brachialis muscles. [7]
In some cases, some of the fibers of the medial root of the median nerve unite with the lateral root of the median nerve and form the median nerve; the remaining medial root fibers run in the McN and then leave it after an expanse, joining the main trunk of the median nerve. In some cases, the lateral root of the median nerve runs in the McN instead of forming the median nerve with the lateral root. It leaves the McN after a distance to join the main trunk of the median nerve. [13],[14]
Sometimes the fibers of the McN unite with the lateral root of the median nerve instead of going its way into the coracobrachialis. After some distance, the McN arises from the median nerve. [6],[15]
The most recurring variation is the presence of a communicating branch that separates from the McN and goes distally to join the median nerve. [16],[17]
In some rare cases (as has been reported here), the McN is absent. The fibers of the McN run within the median nerve through its course without piercing the coracobrachialis. In 1997, Nakatani et al. [18] reported three cases of the McN not perforating the coracobrachialis muscle. In our case, three muscular branches from the resultant median nerve were seen supplying the coracobrachialis, biceps, and brachialis muscles. According to Kerr, [19] Watanabe et al., [20] and Le Minor [7] incidence of this variation ranges from 1.7%, 1.4%, and 0.3% to 2%. [5]
Another finding in our case was that the cutaneous innervation of the lateral part of the forearm came from the continuation of the branch to the brachialis from the median nerve. This is in accordance with the reports of Aydin et al. [21] and Mane and Pandhare. [22]
The absence of the McN should be kept in mind since injury to the median nerve in both the axilla or the arm (bullet and blade wounds) is likely to cause unexpected paresis or paralysis of the flexor musculature of the elbow and loss of cutaneous sensation of the lateral surface of the forearm. [3],[21]
| Conclusion | |  |
The abovementioned case of McN absence and the innervations of flexors of arm by the median nerve should be considered when assessing tumors in the axilla. In this case, care must be taken to dissect cranially than normally as this may affect the median nerve and its branches resulting in dysfunction of the flexor musculature of the elbow, weakness of forearm flexion, and supination.
It must be added that this absence could explain why patients with thoracic outlet syndrome and median nerve infection experience weakness during flexion of their arms.
| Acknowledgement | |  |
The authors acknowledge the contributions of 2012/2013 batch of undergraduate anatomy students of the Federal University Ndufu Alike Ikwo, Ebony State, Nigeria and the dissection hall technicians of the Anatomy Department of the Ebonyi State University, Ebonyi State, Nigeria.
| References | |  |
| 1. | Miller RA. Comparative studies upon the morphology and distribution of the brachial plexus. Am J Anat 1934;54:143-75.  |
| 2. | Bergman RA, Thompson SA, Afifi AK, Saadeh FA. Compendium of Human Anatomic Variation. Munich: Urban & Schwarzeberg; 1988. p. 139-43.  |
| 3. | Gümüsburun E, Adigüzel E. A variation of the brachial plexus characterized by the absence of the musculocutaneous nerve: A case report. Surg Radiol Anat 2000;22:63-5.  |
| 4. | Iwamoto S, Kimura K, Takahashi Y, Konishi M. Some aspects of the communicating branch between the musculocutaneous and median nerves in man. Okajimas Folia Anat Jpn 1990;67:47-52.  |
| 5. | Kocabiyik N, Yalcin B, Yazar F, Ozan H. An accessory branch of musculocutaneous nerve joining median nerve. Neuroanatomy 2005;4:13-5.  |
| 6. | Buch C. On the variation in the method of innervation of the biceps muscle of the arm with special reference to branches from the musculocutaneous nerve and the median nerve. Anat Anz 1964;114:131-40.  |
| 7. | Le Minor JM. A rare variation of the median and musculocutaneous nerves in man. Arch Anat Histol Embryol 1990;73:33-42.  |
| 8. | Moore KL, Dalley AF. Clinically oriented anatomy. 6 th ed. Philadelphia: Lippincott Williams & Wilkins; 1999. p. 737-8.  |
| 9. | Standring S. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 39 th ed. London: Elsevier, Churchill Livingstone; 2005.  |
| 10. | Feray GU, Gülgün K, Mete E. Anastomotic branch from the median nerve to the musculocutaneous nerve: A case report. Int J Exp Clin Anat 2008;2:63-6.  |
| 11. | Linell EA. The distribution of nerves in the upper limb, with reference to variabilities and their clinical significance. J Anat 1921;55:79-112.  |
| 12. | Pećina M, Bojanić I. Musculocutaneous nerve entrapment in the upper arm. Int Orthop 1993;17:232-4.  |
| 13. | Song WC, Jung HS, Kim HJ, Shin C, Lee BY, Koh KS. A variation of the musculocutaneous nerve absent. Yonsei Med J 2003;44:1110-3.  |
| 14. | Nakatani T, Mizukami S, Tanaka S. Three cases of the musculocutaneous nerve not perforating the coracobrachialis muscle. Kaibogaku Zasshi 1997;72:191-4.  |
| 15. | Kosugi K, Shibata S, Yamashita H. Supernumerary head of biceps brachii and branching pattern of the musculocutaneus nerve in Japanese. Surg Radiol Anat 1992;14:175-85.  |
| 16. | Venieratos D, Anagnostopoulou S. Classification of communications between the musculocutaneous and median nerves. Clin Anat 1988;11:327-31.  |
| 17. | Beheiry EE. Anatomical variations of the median nerve distribution and communication in the arm. Folia Morphol (Warsz) 2004;63:313-8.  |
| 18. | Nakatani T, Mizukami S, Tanaka S. Three cases of the musculocutaneous nerve not perforating the coracobrachialis muscle. Kaibogaku Zasshi 1997;72:191-4.  |
| 19. | Kerr AT. The brachial plexus of nerves in man, the variations in its formation and branches. Am J Anat 1918;23:285-395.  |
| 20. | Watanabe M, Takatsuji K, Sakamoto N, Morita Y, Ito H. Two cases of fusion of the musculocutaneous and median nerves. Kaibogaki Zasshi 1985;60:1-7.  |
| 21. | Aydin ME, Kale A, Edizer M, Kopuz C, Demir MT, Corumlu U. Absence of the musculocutaneous nerve together with unusual innervation of the median nerve. Folia Morphol (Warsz) 2006;65:228-31.  |
| 22. | Mane UW, Pandhare SR. Absence of musculocutaneous nerve along with accessory head of biceps brachii. Int J Recent Trends Sci Technol 2011;1:45-8.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|