|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 3
| Issue : 3 | Page : 64-70 |
|
Crossover trial for comparing the biofunctional prosthetic system with conventional procedures
Ken-Ichi Matsuda, Yuko Kurushima, Yoshinobu Maeda, Kaori Enoki, Yusuke Mihara, Kazunori Ikebe
Department of Prosthodontics, Gerodontology and Oral Rehabilitation, Osaka University, Graduate School of Dentistry, Suita, Osaka, Japan
| Date of Web Publication | 29-Sep-2015 |
Correspondence Address:
Dr. Ken-Ichi Matsuda
1-8 Yamadaoka, Suita, Osaka, 565-0871
Japan
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2347-4610.166182

Context: The rapid provision of high.quality complete dentures is an unmet clinical need in some populations. Novel procedures may simplify this service but require validation against existing methods. Aims: The aim of this trial was to evaluate the clinical acceptability of complete dentures fabricated using the biofunctional prosthetic system. (BPS) when compared with conventional methods. Materials and Methods: This study was designed as a crossover trial. The patients wore either a complete denture, which was made using the biofunctional prosthetic system biofunctional prosthetic system complete denture (BPSCD) or a complete denture made with conventional procedures conventional complete denture (CCD) for 3. months before switching to the other dentures. The patients were asked to report their satisfaction levels in an abbreviated version of the Oral Health.Related Quality of Life questionnaire, specifically designed for edentulous patients. (Oral Health Impact Profile for edentulous subjects. [OHIP-EDENT]). Furthermore, the number of adjustments required for each technique to deliver pain.free fitting was noted. Finally, the patients were asked to state which denture gave them superior occlusal feel, comfort, esthetics, and retention and which denture they wished to keep for the long-term. Results: Although the satisfaction score and the OHIP.-EDENT scores showed no significant differences, the majority of patients preferred the BPSCD over the CCD in terms of occlusal feel, comfort, esthetics, and retention. Nine out of 10 patients chose to keep the BPSCD rather than the CCD, with one patient choosing the CCD for purely esthetic reasons. Conclusions: Within the limitation of this study, the BPS produced high.quality complete dentures with satisfactory results and was just as efficient as conventional procedures. Keywords: Biofunctional prosthetic system, complete denture, conventional procedures
How to cite this article:
Matsuda KI, Kurushima Y, Maeda Y, Enoki K, Mihara Y, Ikebe K. Crossover trial for comparing the biofunctional prosthetic system with conventional procedures. Eur J Prosthodont 2015;3:64-70 |
How to cite this URL:
Matsuda KI, Kurushima Y, Maeda Y, Enoki K, Mihara Y, Ikebe K. Crossover trial for comparing the biofunctional prosthetic system with conventional procedures. Eur J Prosthodont [serial online] 2015 [cited 2018 Aug 27];3:64-70. Available from: http://www.eurjprosthodont.org/text.asp?2015/3/3/64/166182 |
| Introduction | |  |
Although the field of implant dentistry has undergone rapid development in recent years, approximately 10% of the world population is still partially or totally edentulous.[1] The proportion of these people who have had implanted treatment is just 1.7%. Despite declining rates of edentulism, there is a clear need for complete denture treatments in edentulous patients in developing and industrialized countries.[1] The delivery of high-quality complete dentures and the development of new fabrication techniques are central to such a service. However, dental schools in many countries have reported difficulties in finding suitable undergraduate teaching cases. As a result, less time has been devoted to the teaching of the fabrication of complete denture prosthodontics and fewer complete denture cases have been treated by new graduates.[1] Thus, the incoming generation of clinicians may not be sufficiently trained to diagnose, plan, and perform the treatment needed by edentulous patients.[1],[2] It has, therefore, been suggested in recent studies to include simplified methods for complete denture construction in the dental curriculum.[3],[4],[5],[6]
A major shortcoming of the suggested simplified methods is the fact that they can only be implemented after some basic clinical training, which will allow the operator to decide whether the outcome of each step is satisfactorily done or not. In order to overcome this problem, some standardized methods for fabricating complete dentures have been introduced, for example, the Biofunctional Prosthetic System (BPS) (Ivoclar Vivadent, Schaan Liechtenstein).[7],[8]
This system includes a comprehensive package of simple, standardized techniques for impression-making, the recording of the maxillomandibular relationship, tooth set-up, and denture fabrication in only four patient visits. Since this method puts a high priority on the patient's own functional morphology and movements during the final impression, border molding, as well as Gothic arch tracing in the closed-mouth position are used instead of the doctor's manual handling as is usually the case in the conventional method. The jaw relationship could be tested at least 2 times during the fabrication process.
The hypothesis of this clinical study was that complete dentures fabricated by dentists with a small amount of training using the biofunctional prosthetic system (Biofunctional Prosthetic System Complete Denture: BPSCD) and those made with conventional procedures (Conventional Complete Denture: CCD) are equally well received by patients.
| Materials and Methods | |  |
A randomized controlled single-blind crossover clinical trial was conducted at the Department of Prosthodontics, Gerodontology, and Oral Rehabilitation at the Osaka University Graduate School of Dentistry, Japan, between November 2010 and April 2012.
Edentulous patients were recruited from the outpatient roster of the Department of Removable Prosthodontics at the Osaka University Dental Clinic.
The inclusion criteria were as follows: (a) Healthy adult patient requiring a new set of complete dentures; (b) complete dentures worn for at least 3 years previously; and (c) the patient is mentally receptive. The exclusion criteria were as follows: (a) Dysfunction disorders of the masticatory system, (b) debilitating systemic disease, or oral mucosal disease, and (c) decline in cognitive function.
After the informed consent process, the patients were stratified by gender and age and then randomly divided into two groups (Group 1 or Group 2) within the stratified blocks of participants. The blocks were generated from a random-number table by a specialist in statistics. Group 1 received BPSCD treatment in the first phase followed by CCD in the second phase, and Group 2 received CCD treatment in the first phase and BPSCD in the second phase [Figure 1]. The treating clinicians were 10 resident dentists in the Department of Prosthodontics (six male/four female; mean age: 24.5, mean clinical experience: 2 years). Each clinician attended to one patient.
A sample size calculation should have been done based on the results of a previous study. However, this was the first study ever to compare the BPS with the conventional procedures. Therefore, we could not anticipate the effect-size, and it was difficult to estimate the sample size correctly. The number of participants was limited due to the difficulty in finding suitable candidates who were willing to receive the two different complete denture treatments and clinicians who were resident dentists. Thus, in this pilot clinical study, the sample size was limited to ten participants.
To maintain the "blind" nature of the trial, patients were not informed about the type of dentures they had received or about the differences between the two types. However, due to the design of this clinical trial, blinding of the treating clinicians and dental technicians was not possible. This study protocol was given ethical approval by the Institutional Review Board of the Osaka University Graduate School of Dentistry (#H22-E25-1: Clinical trial registration ID of Osaka University Dental Hospital), and registered in the UMIN Clinical Trials Registry (UMIN000016650).
For CCD, the participants received treatment according to the conventional method used at the Department of Removable Prosthodontics, Osaka University Dental Clinic. At the first appointment, a preliminary impression was made using a stock impression tray (Abe Impression Tray, Tokyo Shizaisha Co., Tokyo, Japan) and irreversible hydrocolloid impression material (Aroma Fine Plus, GC Co., Tokyo, Japan). At the second appointment, a custom tray (Tray-Resin II, SHOFU Co., Kyoto, Japan) was manually adjusted by molding the border with an impression compound (ISO Functional Compound, GC Co.). In addition, a final impression was taken in hydrophilic vinyl polysiloxane impression material (Examix Fine Injection Type, GC Co.). At the third appointment, the vertical maxillomandibular relationship was determined at approximately 2 mm less at the posterior part than the vertical dimension at rest. The horizontal maxillomandibular relationship was recorded with wax occlusal rims and silicone registration paste (Exabite II, GC Co., Tokyo, Japan). A bilateral balanced occlusion was achieved with semi-anatomical artificial teeth (Verasia SA, SHOFU Co.). A wax try-in was performed at the fourth appointment. Following a successful try-in and adjustment process, the denture base for the CCD was polymerized with cold-curing polymethyl methacrylate denture base resin (ParaXpress, Heraeus-Kulzer Co., Hanau, Germany), and the completed dentures were delivered to the patient at the fifth appointment.
The BPSCD was fabricated according to the manufacturer's instructions. Preliminary impressions were taken with the Accu-Dent System 1 (Ivoclar Vivadent, Schaan, Liechtenstein), which uses two materials of different viscosity. The lower viscosity material (System 1 Syringe Accu-Gel; Ivoclar Vivadent) was injected into the vestibular areas using a syringe, whereas the higher viscosity material (System 1 Tray Accu-Gel; Ivoclar Vivadent) was applied to the tray to support the syringe material. At the same appointment, an approximate maxillomandibular relationship was recorded using a Centric Tray (Ivoclar Vivadent). In the laboratory, the primary casts were then mounted in this approximate maxillomandibular relationship using the Centric Tray, with custom trays fabricated with the help of the Gnathometer M tracing device (Ivoclar Vivadent). At the second appointment, the final impressions and a definitive record of the maxillomandibular relationship were obtained. The final impressions were made with the patient in the "mouth-closed" position using vinyl polysiloxane impression material (Virtual Heavy Body and Virtual Light Body; Ivoclar Vivadent). The vertical maxillomandibular relationship was determined at approximately 2 mm less at the posterior part than the vertical dimension at rest. The horizontal maxillomandibular relationship was determined according to Gothic arch tracing using the Gnathometer M tracing device and fixed with a silicone registration paste (Virtual CAD Bite; Ivoclar Vivadent) [Figure 2]. After mounting the final cast, semi-anatomical artificial teeth (SR Phonares NHC; Ivoclar Vivadent) were placed according to the manufacturer's instructions such that a bilateral balanced occlusion was achieved. The wax try-in was performed at the third appointment. After the try-in, the dentures were polymerized using the Ivocap system (Ivoclar Vivadent). Finally, the patient received the dentures at the fourth appointment. [Table 1] shows each clinical step of the fabrication process of CCD and BPSCD. All the laboratory work of both dentures was produced by one technician affiliated with the dental laboratory of Osaka University Dental Hospital (clinical experience: 10 years).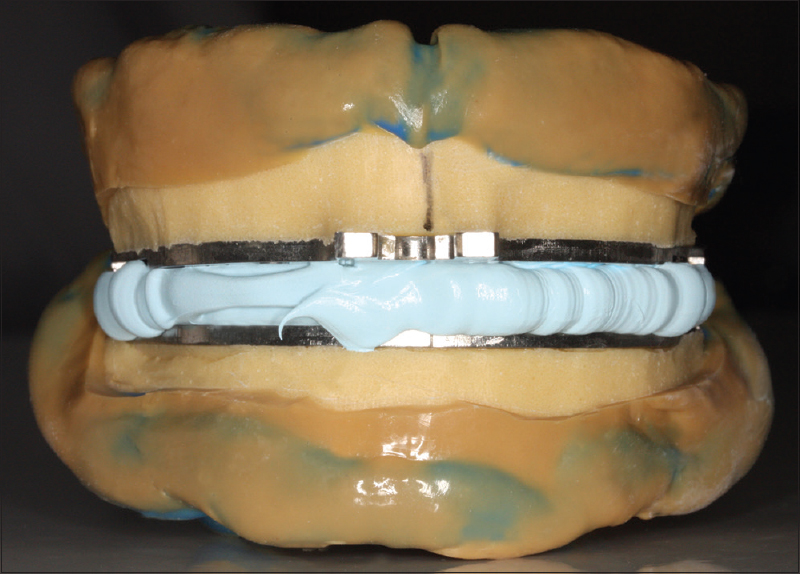 | Figure 2: Final impression and recording of the maxillomandibular relationship
Click here to view |
All the patients attended the follow-up appointments. The clinical outcomes were first assessed after 3 months of comfortably wearing the first set of dentures (calculated from the 1st day on which the patients felt no pain or discomfort with the new dentures). Subsequently, the prostheses were changed and a second evaluation was carried out after a further 3 months.
An evaluation of the patient satisfaction with the dentures was performed with a visual analog scale (VAS) to quantify their satisfaction in response to the question: "How good is this denture?" Assessors marked their opinion on a 100-mm scale between 0 (0 mm = worst) and 100 (100 mm = best).[9]
The oral health-related quality-of-life (OHR-QoL) was measured with the Japanese version of the Oral Health Impact Profile for edentulous subjects (OHIP-EDENT-J), a shortened version of the OHIP and with improved relevance to clinical studies investigating prosthodontic procedures in edentulous patients.[10] The OHIP-EDENT-J features 19 items derived from the English-language OHIP-EDENT. The OHIP-EDENT questionnaire includes seven domains. These domains reflect the hierarchy of increasingly complex and disruptive impacts or problems. The first three domains - functional limitations, physical pain, and psychological discomfort: Include items that impact the individual's experience, whereas items in the disability and handicap domains represent problems that may affect everyday activities and social functions.[11] The response options were "very often (4)," "fairly often (3)," "occasionally (2)," "hardly ever (1)," and "never (0)." The total OHIP-EDENT-J score for each patient was calculated by adding the response codes of all the 19 items.
Most dentures had required some adjustments before they were deemed "pain-free." The number of adjustments required for each denture was counted to give an indication of the accuracy and adequacy of the clinical practice and denture fabrication process. In this study, the visiting frequency for denture adjustment was once a week, the end of the adjustment process was determined when the patient could use the dentures without any pain or a major inconvenience.
Participants were asked to compare four aspects of the two dentures, namely: (1) Occlusal feel, (2) pain, (3) appearance, and (4) retention. The questionnaire comprised four questions:
- Which denture do you feel is better for chewing?
- Which denture produces less pain while eating?
- Which denture do you think looks better?
- Which denture do you think has better retention?
(Options: "1:First denture," "2: Second denture" or "3: There is little difference between the two dentures [no preference]")
After the second evaluation, the participants were asked to decide which denture they would prefer to use in the long-term.
The satisfaction scores, OHIP-EDENT-J scores, and the numbers of adjustments were not normally distributed, as confirmed by the Shapiro-Wilk test. Therefore, differences in these data sets were analyzed using the Wilcoxon signed-rank test. P values of <0.05 were considered to be statistically significant. All the data were analyzed using SPSS version 19.0 statistical software (IBM Co., Tokyo, Japan).
| Results | |  |
Ten edentulous patients (five men/five women) with a mean age of 76.5 years (67–86 years) participated in this clinical trial [Table 2]. All the participants received two types of dentures which were evaluated by each patient. Almost all of the patients were satisfied with both of the new dentures. The OHIP-EDENT-J score for BPSCD (median: 34.5) was slightly but not significantly (P = 0.722) lower than for CCD (median: 35.8) [Figure 3]. Furthermore, [Figure 4] shows the denture satisfaction assessed with VAS. The denture satisfaction for BPSCD (median: 86.5) was slightly lower than the score for CCD (median: 88). However, there was no significant difference between these values (P = 0.262).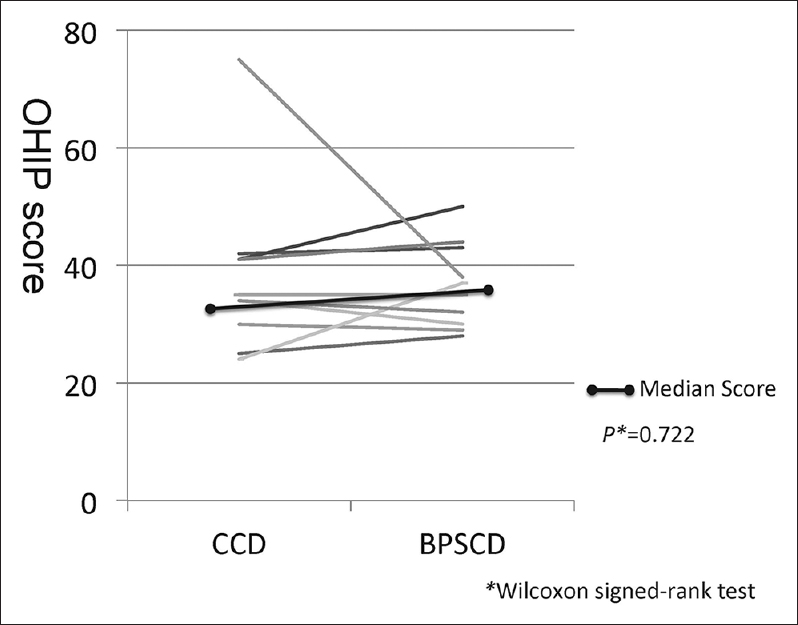 | Figure 3: The Japanese version of the Oral Health Impact Profile for edentulous subjects' score of CCD and BPSCD in each patient, and the median Japanese version of the Oral Health Impact Profile for edentulous subjects score
Click here to view |
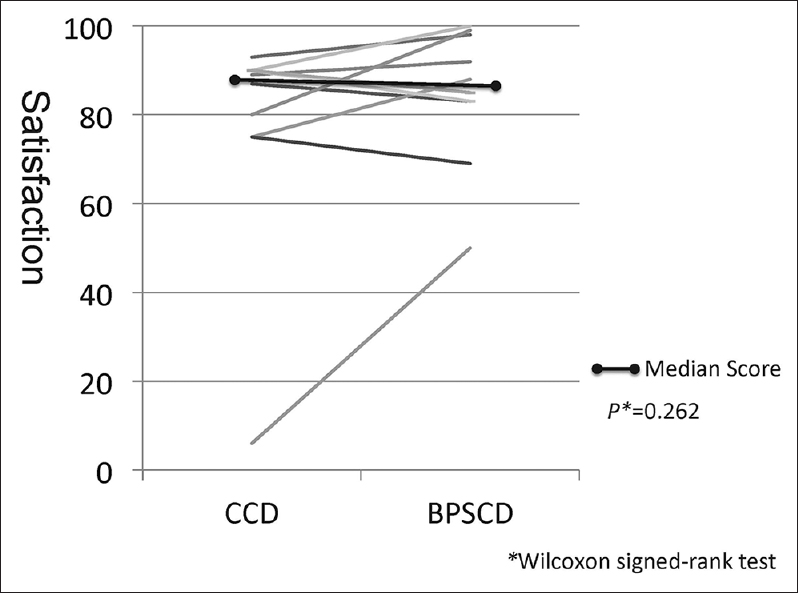 | Figure 4: Satisfaction with CCD and BPSCD of each patient, and the median score
Click here to view |
The median number of denture adjustments for CCD was 4.5 and for BPSCD 3.5. There was a significant difference between the two denture types (P = 0.027) [Figure 5] indicating that BPSCD required fewer adjustments than the CCD.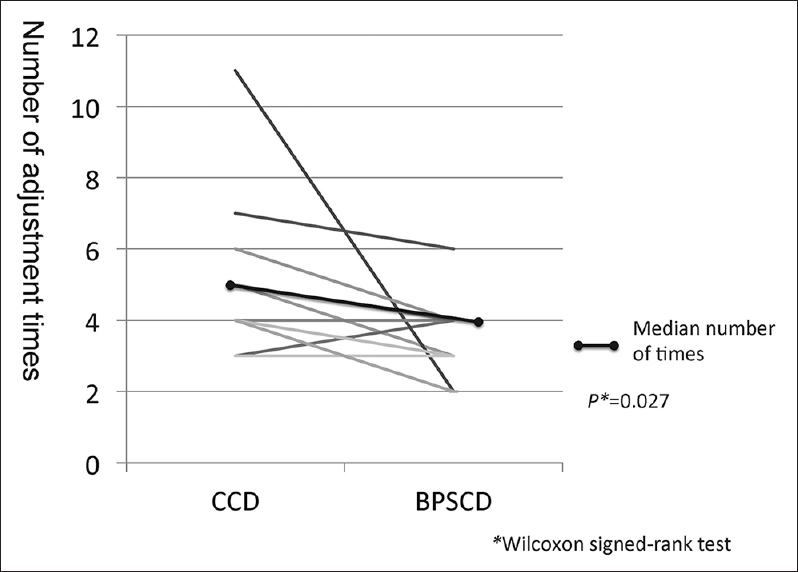 | Figure 5: The number of denture adjustments for CCD and BPSCD, and the median number of adjustments
Click here to view |
[Table 3] shows the results of the questionnaire comparing both dentures types. Almost all the participants considered the BPSCD to be superior or equivalent to CCD in the various aspects evaluated, with only one patient rating the CCD to provide a better occlusion and cause less pain. Although three patients found the CCD to look better, none felt that it had better retention, and ultimately, all but one patient chose the BPSCD as their preferred long-term option.
| Discussion | |  |
Complete dentures can be fabricated by means of various procedures. Since the vast majority of complete dentures, however, is provided by general dental practitioners, usually the simplest clinical and laboratory protocols, which were learned by dental students, are used.
This assumption leads us to the following conclusions: (1) The curriculum of dental students should include the simplest method of fabricating complete dentures and (2) the simplest method of fabricating complete dentures should be given preference over more complex procedures in practice.[3],[4],[5],[6]
Cunha et al. reported that the simplified method for complete denture fabrication is able to restore the masticatory function to a level comparable to that of a conventional protocol, both physiologically and according to the patient's perceptions.[12] However, there is one big problem in their article. The information about the attending dentists is not clear. If the practitioners are prosthodontic specialists, the differences between the two methods should be small. We believe that simplified methods should be easy to use and lead to good clinical results for all dentists. Therefore, in our study, the treating clinicians were young resident dentists (mean clinical experience: 2 years). The simplified method which they used required fewer treatment appointments than conventional techniques due to a reduction of some of the common clinical steps. Furthermore, BPS also required fewer visits for the patients (four appointments, when compared with five for conventional methods) by using unique devices and standardized ideas. It might be the answer to both demands as it is a simple, standardized system for fabricating complete dentures.
In many aspects, we found no statistically significant differences between the two fabrication methods. These results reflected the high levels of satisfaction of the patients with both dentures. This is also applied to the OHR-QoL measures. It has been reported that new dentures improve the patient's QoL.[13],[14] In this study, the OHR-QoL was not significantly greater with BPSCD. In this clinical trial, almost all the patients were satisfied with both of their dentures until the appointment for the evaluations. In other words, they used both dentures without strong pain or inconvenience: The OHR-QoL was therefore correspondingly high. Further, in this study, each evaluation was carried out after 3 months usage of each denture. Due to the long time span between each evaluation, the participants did not actually compare the two dentures. Therefore, the OHR-QoL score did not differ too much among the two dentures, and we did not find any significant difference.
However, in comparing the questionnaires with regard to denture function, including retention, esthetics, and absence of pain, most participants considered BPSCD to be superior or equivalent to CCD and all but one of the participants selected BPSCD for their final choice. The participant who selected CCD did so because she preferred the appearance of the anterior teeth in this set of dentures, despite finding BPSCD to be superior in the occlusal feel, absence of pain, and retention. These results indicate that BPSCD is subjectively superior to CCD.
The significant difference between the numbers of adjustment appointments required for the two dentures indicates that BPSCD requires less "adjustments" than the CCD, and that BPSCDs fit very well immediately after completion. Denture adjustments can be required for various reasons such as residual ridge resorption, the health of the soft tissues covering edentulous areas, the adaptability of patients to complete dentures, the skill of the clinicians and dental laboratory technicians involved in the treatment, the jaw relationship, denture occlusion, and other factors.[15] However, many of these patient-related factors were canceled out by the crossover trial design. Therefore, we believe that the number of adjustments required is a useful indicator for evaluating the overall denture quality.
There were several limitations in the design of this study. We acknowledge the limitations, with the most significant being the limited significant power of only 10 participants. This group is too small to make conclusions for all edentulous patients. Furthermore, it is unclear which clinical step of the fabrication of complete dentures is the most critical.
A multitude of methods for the fabrication of complete dentures has been suggested in the dental literature, with three principal areas (impressions, the maxillomandibular relationship record, and the occlusal scheme) influencing the overall quality of dentures.[5] In our clinical trial, both dentures were given the same occlusal scheme, but due to the fact that the artificial teeth used were different, the teeth arrangement varied. Further differences existed between BPSCD and CCD in terms of making impressions and recording the maxillomandibular relationship. Therefore, several possibilities could explain the apparent superiority of BPSCD. The combination impression approach for preliminary impressions provides high quality primary casts, thus, enabling the final impression to provide a record in the closed position to reproduce the functional figure more accurately than conventional impressions. The BPSCD technique also records multiple maxillomandibular relationships (preliminary record with the centric tray, definitive record with Gothic arch tracing using the Gnathometer M), permitting greater accuracy in recording and replicating the correct maxillomandibular relationship. However, in this study we were unable to determine which of these features had the greatest influence and led to the superiority of BPSCD over CCD. Further research should, thus, be undertaken in order to provide more details.
| Conclusion | |  |
Within the limitations of this study, the hypothesis was confirmed, indicating that with the BPS even dentists with a small amount of clinical training can quickly produce complete dentures and satisfactory results that are comparable to those achieved with conventional procedures.
Acknowledgments
The study protocol was approved by the Institutional Review Board of the Osaka University Graduate School of Dentistry. This research was supported by the research fund of the Department of Prosthodontics, Gerodontology, and Oral Rehabilitation, Osaka University Graduate School of Dentistry.
Financial support and sponsorship
His research was supported by the research fund of Department of Prosthodontics, Gerodontology and Oral Rehabilitation, Osaka University Graduate School of Dentistry.
Conflicts of interest
Kenichi Matsuda and Yoshinobu Maeda are remunerated instructors who have given educational lectures at the request of the Ivoclar Vivadent company.
| References | |  |
| 1. | Carlsson GE, Omar R. The future of complete dentures in oral rehabilitation. A critical review. J Oral Rehabil 2010;37:143-56.  |
| 2. | Douglass CW, Shih A, Ostry L. Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent 2002;87:5-8.  |
| 3. | Owen CP. Guidelines for a minimum acceptable protocol for the construction of complete dentures. Int J Prosthodont 2006;19:467-74.  |
| 4. | Kawai Y, Murakami H, Shariati B, Klemetti E, Blomfield JV, Billette L, et al. Do traditional techniques produce better conventional complete dentures than simplified techniques? J Dent 2005;33:659-68.  |
| 5. | Heydecke G, Vogeler M, Wolkewitz M, Türp JC, Strub JR. Simplified versus comprehensive fabrication of complete dentures: Patient ratings of denture satisfaction from a randomized crossover trial. Quintessence Int 2008;39:107-16.  |
| 6. | Owen CP. Standards of care: Good of evil? Int J Prosthodont 2009;22:328-30.  |
| 7. | Nekora-Azak A, Evlioglu G, Ozdemir-Karatas M, Keskin H. Use of biofunctional prosthetic system following partial maxillary resection: A clinical report. J Oral Rehabil 2005;32:693-5.  |
| 8. | Saini V, Singla R. Biofunctional prosthetic system: A new era complete denture. J Pharm Bioallied Sci 2011;3:170-2.  |
| 9. | Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990;13:227-36.  |
| 10. | Allen F, Locker D. A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. Int J Prosthodont 2002;15:446-50.  |
| 11. | Ikebe K, Hazeyama T, Enoki K, Murai S, Okada T, Kagawa R, et al. Comparison of GOHAI and OHIP-14 measures in relation to objective values of oral function in elderly Japanese. Community Dent Oral Epidemiol 2012;40:406-14.  |
| 12. | Cunha TR, Della Vecchia MP, Regis RR, Ribeiro AB, Muglia VA, Mestriner W Jr, et al. A randomised trial on simplified and conventional methods for complete denture fabrication: Masticatory performance and ability. J Dent 2013;41:133-42.  |
| 13. | Adam RZ, Geerts GA, Lalloo R. The impact of new complete dentures on oral health-related quality of life. SADJ 2007;62:264-6, 268.  |
| 14. | Ellis JS, Pelekis ND, Thomason JM. Conventional rehabilitation of edentulous patients: The impact on oral health-related quality of life and patient satisfaction. J Prosthodont 2007;16:37-42.  |
| 15. | Drago CJ. A retrospective comparison of two definitive impression techniques and their associated postinsertion adjustments in complete denture prosthodontics. J Prosthodont 2003;12:192-7.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
[Table 1], [Table 2], [Table 3]
|