|
 
 |
|
REVIEW ARTICLE |
|
|
|
| Year : 2011 | Volume
: 17
| Issue : 3 | Page : 126-131 |
| |
Neural tube defects between folate metabolism and genetics
Helmi Y Alfarra, Sabreen R Alfarra, Mai F Sadiq
Department of Biological Sciences, Yarmouk University, Irbid, Jordan,
| Date of Web Publication | 20-Jan-2012 |
Correspondence Address:
Helmi Y Alfarra
508 -1094 Wellington Street, Halifax, Nova Scotia, Canada, B3H 2Z9
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/0971-6866.92082

 Abstract Abstract | | |
Neural tube defects (NTDs) are the second most common severely disabling human congenital defects. Worldwide, NTDs incidence is approximately one per 1000 live births and varies between 0.78 and 12 per 1000 births in general populations. NTDs causation involves multiple genes, nutritional and environmental factors. Research in the next stage should include bigger populations and bigger studies that would be suitable to detect significant links and conclusions with relatively minor risk factors; analysis of multiple candidate genes to detect potential gene-gene interactions; detailed analysis of patient samples stratified by phenotype.
Keywords: Folic acid, MTRR, MTR, MTHFR, NTDs
How to cite this article:
Alfarra HY, Alfarra SR, Sadiq MF. Neural tube defects between folate metabolism and genetics. Indian J Hum Genet 2011;17:126-31 |
How to cite this URL:
Alfarra HY, Alfarra SR, Sadiq MF. Neural tube defects between folate metabolism and genetics. Indian J Hum Genet [serial online] 2011 [cited 2016 May 13];17:126-31. Available from: http://www.ijhg.com/text.asp?2011/17/3/126/92082 |
 Introduction Introduction | |  |
The neural tube is the embryonic precursor of the brain and the spinal cord. Building a neural tube is an extremely complex phenomenon where cells need to change in shape, migrate and differentiate to form a hollow tube from a flat sheet of thickened epithelial cells (the neural plate). The normal closure of the neural plate occurs very early in human pregnancy from day 21 until day 28 following conception or one week after the expected menstruation. [1] Abnormal closure of the neural plate results in neural tube defects (NTDs). NTDs are very complex birth defects that involve the interactions of multiple systems such as the central nervous system, the urological system and the musculoskeletal system. NTDs seem to be related to defects in the folate-methionine metabolic pathways since preconception of vitamin B12 supplementation with folic acid proved to substantially reduce the risk for NTD affected pregnancies and many different investigations showed alteration in folate status in the mothers of NTDs affected children. In these mothers, folate absorption, transport, and metabolism are the focus of intense research to clarify the mechanisms underlying these observations, yet the bases of this defect remain unknown. Further studies involved examining the different polymorphisms of genes related to folate metabolism. [2],[3] NTDs are the second most common severely disabling human congenital defects. Worldwide, NTDs incidence is approximately one per 1000 live births and varies between 0.78 and 12 per 1000 births in general populations. [4],[5],[6] In Jordan, three studies were performed during the years 1991 to 2003, showed that the average incidence of NTDs in the Jordanian population is about 3.8 per thousand. [7],[8],[9] The correlation between the birth of NTD affected children and the maternal polymorphisms of two genes is related to the folate metabolic pathway. Methylenetetrahydrofolate-dehydrogenase (MTHFD1) 1958 (G>A) and methionine synthase polymorphisms MTR 2756 (A>G) and MTR 2758(C>G) in the Jordanian population have been examined.
 Development of the neural tube (neurulation) Development of the neural tube (neurulation) | |  |
Neurulation is a fundamental embryonic process that leads to the development of the neural tube, which is the precursor of the brain and spinal cord. Neurulation occurs through two distinct phases: primary neurulation (weeks 3-4) that leads to the formation of the brain and most of the spinal cord till the upper sacral level, followed by secondary neurulation (weeks 5-6) that creates the lowest portion of the spinal cord including most of the sacral and all the coccygeal regions. [10],[11]
 Primary neurulation Primary neurulation | |  |
This process involves formation of the neural plate, shaping of the neural plate, bending and fusion of the neural plate at the midline. [12] Shaping of the neural plate involves conversion of the neural plate into an elongated structure that is broad at the cranial and narrow at the spinal regions. In this complex process, cells elongate mediolaterally and produce polarized cellular protrusions that enable them to move directionally and to intercalate with other neighboring cells. This change in shape and movement results in convergence toward the midline and extension of the tissue along the anteroposterior axis.
Bending of the neural plate implicates formation of the neural folds at the lateral extremes of the neural plate and the subsequent elevation and convergence of these folds toward the dorsal midline [Figure 1]. [12] 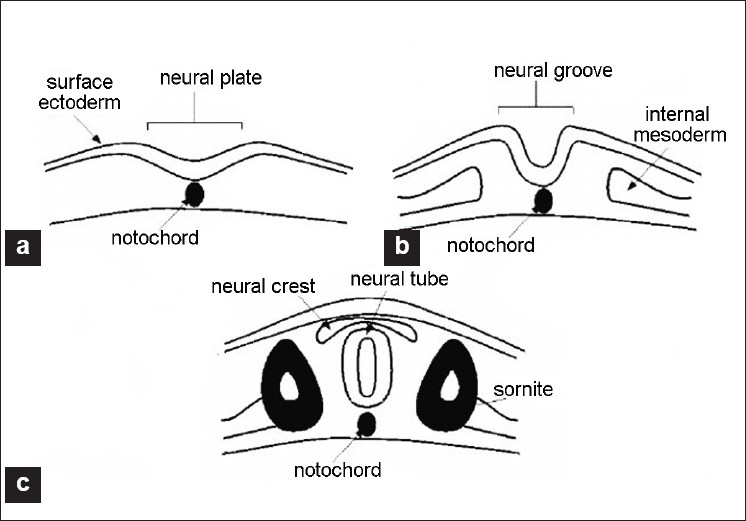 | Figure 1: Scheme of the embryo's transverse cross sections during neurulation process. A = neural plate stage, B = neural groove stage, C = neural tube stage from (12).
Click here to view |
 Secondary neurulation Secondary neurulation | |  |
Secondary neurulation begins after completion of the primary neurulation. During this process, the neural tube is produced by the tail bud, a mass of stem cells representing the remnant of the primitive streak that are located at the caudal end of the embryo. These stem cells undergo proliferation and condensation followed by cavitation and fusion with the central canal of the neural tube that is formed by primary neurulation. [13],[14] Failure of secondary neurulation leads to the rare closed forms of NTDs where the developing neural tube fails to separate from other tissues of the tail bud. [14]
 Folate metabolism Folate metabolism | |  |
Folate is a critical nutrient in maintaining normal cell growth and division and therefore it is important for human development. [15],[16] After uptake of folate in the enterocytes, intracellular polyglutamate synthesis occurs, followed by reconversion into monoglutamates that are reduced to biologically active tetrahydrofolate. [16] After methylation, the folates enter the portal circulation as 5-methyltetrahydrofolate. The majority of this folate is taken up by the liver, which plays a central role in folate homeostasis. [16] The cellular uptake is mediated via specific folate receptors. Plasma 5-methyltetrahydrofolate (30-40%) is bound to albumin, α2 macroglobulin, transferrin, and folate-binding protein. [15] In the cell, 5- methyltetrahydrofolate serves as a methyl donor and as a source of tetrahydrofolate. Tetrahydrofolate acts as an acceptor of one-carbon units, producing a variety of other folates, which, in turn, are specific coenzymes in intracellular reactions. [16] One of these is 5, 10- methylenetetrahydrofolate that is reduced by the enzyme 5, 10- methylenetetrahydrofolate reductase to 5-methyltetrahydrofolate. 5-Methyltetrahydrofolate carries the methyl group required for conversion of homocysteine to methionine (remethylation pathway of homocysteine). This methyl group is initially transferred to cob (I)alamin, to prevent methylcobalamin that is demethylated by homocysteine to form methionine by the cobalamin-dependent enzyme methionine synthase. [15] To maintain the enzyme activity, a reductive methylation by methionine synthase reductase is required. [16] Folate transport and metabolism are suggested to be under genetic control. [17]
 Folic acid and genetic maintenance Folic acid and genetic maintenance | |  |
Folic acid and its derivatives are important in several reactions in the single carbon transfer, which include the biosynthesis of purines, thymidines and the remethylation of homocystine to methionine. Normal folic acid and vitamin B12 metabolism were reported to be essential for normal development of the neural tube. [Figure 2] shows the main steps of homocysteine and folate metabolism pathway. [18] Folic acid plays an important role in DNA metabolism; where it is required for the synthesis of dTMP from dUMP and the maintenance of DNA methylation. Under conditions of folic acid deficiency, dUMPs accumulate in the cell and get a better chance to be incorporated into the DNA instead of thymine. [19] There are good evidences suggesting that excessive incorporation of uracil in DNA not only leads to point mutations but may also lead to the generation of single- and double-stranded DNA damage, chromosome breakage, fragmentation and micronucleus formation. [20],[21] Folic acid and vitamin B12 are required for the synthesis of methionine and the common methyl donor S-adenosylmethionine (SAM), are required for the maintenance of methylation patterns in DNA that determine gene expression and DNA conformation. [22] 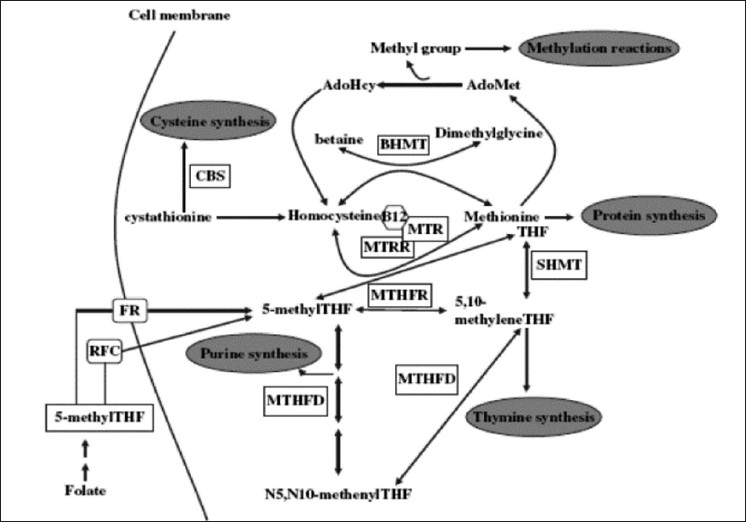 | Figure 2: Simple overview of folate and homocysteine metabolic cycles. AdoHcy, S-adenosylhomocysteine; Ado-Met, S-adenosylmethionine; BHMT, betaine-homocysteine methyltransferase; CBS, cystathionine b-synthase; FR, folate receptor; MTHFD, methylenetetrahydrofolate dehydrogenase; MTHFR, methylenetetrahydrofolate reductase; MS, methionine synthase; MSR, methionine synthase reductase; RFC, reduced folate carrier; SHMT, serine hydroxymethyltransferase; THF, tetrahydrofolate (39).
Click here to view |
When the concentration of vitamin B12 and methionine is low, SAM synthesis will be insufficient leading to the minimization of methylene tetrahydrofolate reductase (MTHFR) activity on the irreversible conversion of 5, 10-methylene tetrahydrofolate to 5- methyltetrahydrofolate, thus favoring an increase of uracil incorporation into the DNA. Deficiencies in folic acid and vitamin B12 therefore can lead to: (1) an elevated DNA damage rate and altered methylation of DNA, both are important risk factors in cancer [20],[21],[22],[23] and (2) an increased level in homocysteine status, an important risk factor for cardiovascular disease. [24],[25] The consequences of folic acid and vitamin B12 deficiencies may also play an important role in developmental and neurological abnormalities. [20],[21]
 Folate, homocysteine and neural tube defects Folate, homocysteine and neural tube defects | |  |
It was reported that folate and folate derivatives are specifically linked to NTD in human since women who had pregnancies associated with fetal malformations had a higher incidence of aberrant folate metabolism [25] and a key role of folate in preventing NTD was suggested. [26] Maternal folic acid levels studies in the first trimester of pregnancy in mothers with NTD offspring tended to be lower than in the controls. Disorder of homocysteine metabolism was suggested to be the basis for NTDs [27] and was confirmed by the fact that homocysteine value in mothers with spina bifida affected offspring was 75% higher than the control. [28]
 Genetic basis of NTDs Genetic basis of NTDs | |  |
Many familial studies indicated a significant genetic component to NTDs (29). NTDs are associated with known genetic syndromes such as trisomies 21, 13 and 18, Meckel syndrome, anterior sacral meningocele stenosis and with various chromosome rearrangements. [30]
 Candidate genes studied in human NTDs Candidate genes studied in human NTDs | |  |
Accordingly as it is articulated in the previous section, it is clear that folate deficiency is a contributor to the etiology of NTDs, and genes in this metabolic pathway have been the basis for many candidate gene studies. Several potential genes have been derived from folic acid pathway [Figure 2]. [Table 1] summarizes the results of studies on the NTD correlation with different genes in different populations. These genes included the polymorphisms of MTHFD1, MTHFR, MTR and others, including what population was studied.
 Conclusions and Recommendations Conclusions and Recommendations | |  |
The etiology of NTD is poorly understood, but it is now suggested that there is a complex interplay between environmental and genetic factors. [31] Knowledge of the association between NTD and various genetic markers related to development may help increase our understanding of the genetics of pathogenesis of NTD. [38]
It is not easy to identify and determine the genetic risk factors of the NTDs because of the multiplicity of genes that participate in neurulation, and the importance of gene-environment interactions. Related researches of common genetic polymorphism especially that are enclosed in the folate one-carbon metabolism, indicate risk factors such as MTHFR, but no particular folate-related gene has yet been occupied as a major determinant of possibility for NTDs. Studies in a large-scale will be necessary to provide satisfactory statistical power to credibly test whether such polymorphisms are truly NTD susceptibility factors. [40] It will be more imperative too, if multiple genes (folate-related and others) were evaluated in the same persons in order to detect possible compounding belongings of combinations of risk alleles that, individually, might not be statistically significant. [17]
 References References | |  |
| 1. | Brouns MR, Straaten HW. Models of neural tube defects. Drug Discov Today 2005;2:285-90. 
|
| 2. | Asindi A, Al-Shehri A. Neural tube defects in the Asir region of Saudi Arabia. Ann Saudi Med 2001;21:26-9. 
[PUBMED]  |
| 3. | Relton CL, Wilding CS, Pearce MS, Laffling AJ, Jonas PA, Lynch SA, et al. Gene-gene interaction in folate related genes and risk of neural tube defects in a UK population. J Med Genet 2003;41:256-60. 
|
| 4. | Zhu H, Wicker NJ, Shaw GM, Lammer EJ, Hendricks K, Suarez L, et al. Homocysteine remethylation enzyme polymorphisms and increased risks for neural tube defects. Mole Genet Metab 2002;78:216-21. 
|
| 5. | World Health Organization, 2006. Prevention of neural tube defects. Available from: http://www.who.int/making-pregnancy_safer/publications/en/. [Retrieved on 2008 Aug 30]. 
|
| 6. | Rampersaud E, Bassuk AG, Enterline DS, George TM, Siegel DG, Melvin EC, et al. Whole genomewide link age screen for neural tube defects reveals regions of interest on chromosome 7 and 10. J Med Genet 2007;42:940-6. 
|
| 7. | Daoud A, Al-kaysi F, El-Shanti H, Batieha A, Obeidat A, Al-Sheyyab M. Neural tube defects in northern Jordan. Saudi Med J 1996;17:78-81. 
|
| 8. | Aqrabawi H. Incidence of Neural tube defects among neonates at King Hussein Medical Center, Jordan. Eastern Mediterranean Health J 2005;11:819-23. 
|
| 9. | Masri A. Neural tube defects in Jordan: A hospital based study. J Pediatr Neurol 2006;4:245-9. 
|
| 10. | Padmanabhan R. Etiology, pathogenesis and prevention of neural tube defects. Congenital Anomalies 2006;46:55-67. 
|
| 11. | Rossi A, Biancheri R, Cama A, Piatelli G, Ravegnani M, Tortori-Donati P. Imaging in spine and spinal cord malformation. Eur J Radiol 2004;50:177-200. 
|
| 12. | Gos M, Szpecht-Potocka A. Genetic basis of neural tube defects: Irregulatory genes for the neurulation process. J Appl Genet 2002;43:343-50. 
|
| 13. | Catala M. Genetic control of caudal development. Clin Genet 2002;61:86-96. 
|
| 14. | Copp A, Greene N, Murdoch J. The genetic basis of neurolation. Nat Rev Genet 2003;4:784-93. 
|
| 15. | Lucock M. Folic acid: Nutritional biochemistry, molecular biology, and role in disease processes. Mol Genet Metab 2000;71:121-38. 
|
| 16. | Fowler B. The folate cycle and disease in humans. Kidney Int 2001;59:S221-9. 
|
| 17. | Boyles LA, Hammoch P, Speer CM. Candidate gene analysis in human neural tube defects. Am J Med Genet Part C 2005;153C:9-23. 
|
| 18. | Yi P, Melnyk S, Pogribna M, Pogribny IP, Hine RJ, James SJ. Increase in plasma homocysteine associated with parallel increases in plasma S-adenosylhomocysteine and lymphocyte DNA hypomethylation. J Biol Chem 2000;275:29,318-29,323. 
|
| 19. | Eto I, Krumdieck CL. Role of vitamin B12 and folate in carcinogenesis. In Essential Nutrients in Carcinogenesis. In: Poirier LA, Newberne PM, Pariza MW, editors. New York: Academic Press; 1986. p. 313-30. 
|
| 20. | Blount BC, Ames BN. DNA damage in folate deficiency. Bailleres Clin Haematol 1995;8:461-78. 
|
| 21. | Blount BC, Mack MM, Wehr CM, MacGregor JT, Hiatt RA, Wang G, et al. Folate deficiency causes uracil misincorporation into human DNA and chromosome breakage: Implications for cancer and neuronal damage. Proc Natl Acad Sci USA 1997;94:3290-5. 
|
| 22. | Zingg JM, Jones PA. Genetic and epigenetic aspects of DNA methylation on genome expression, evolution, mutation and carcinogenesis. Carcinogenesis 1997;18:869-82. 
|
| 23. | Lindahl T, Wood RD. Quality control by DNA repair. Science 1999;286:1897-905. 
|
| 24. | Pancharuniti N, Lewis CA, Sauberlich HE, Perkins LL, Go RC, Alvarez JO, et al. Plasma homocysteine, folate and vitamin B-12 concentrations and risk for early-onset coronary artery disease. Am J Clin Nutr 1994;59:940-8. 
|
| 25. | Hibbard BM, Smithells RW. Folic acid metabolism and human embryopathy. Lancet 1965;1:1254. 
|
| 26. | Hibbard BM. The role of folic acid in pregnancy with particular reference to anaemia, abruption, and abortion. J Obstet Gynaecol Br Commonwlth 1964;71:529-42. 
|
| 27. | Steegers-Theunissen RP, Boers GH, Trijbels FJ, Eskes TK. Neural-tube defects and derangement of homocysteine metabolism. N Engl J Med 1991;324:199-200. 
|
| 28. | Van der Put NM, Thomas CM, Eskes TK, Trijbels FJ, Steegers-Theunissen RP, Mariman EC, et al. Altered folate and vitamin B12 metabolism in families with spina bifida offspring. Q J Med 1997a;90:505-10. 
|
| 29. | Elwood J, Little J, Elwood J. Epidemiology and control of neural tube defects. Oxford: Oxford University Press; 1992. 
|
| 30. | Detrait ER, George TM, Etchevers HC, Gilbert JR, Vekemans M, Speer MC. Human neural tube defects: Developmental biology, epidemiology, and genetics. Neurotoxicol Teratol 2005;27:515-24. 
|
| 31. | Hol FA, van der Put NM, Geurds MP, Heil SG, Trijbels FJ, Hamel BC, et al. Molecular genetic analysis of the gene encoding the trifunctional enzyme MTHFD1 (mthylenetetrahydrofolatecyclohdrolase, formyltetrahydrofolate synthase) in patients with neural tube defects. Clin Genet 1998;53:119-25. 
|
| 32. | Brody LC, Conley M, Cox C, Kirke PN, McKeever MP, Mills JL, et al. A polymorphism, R653Q, in the trifunctional enzyme methylenetetrahydrofolate -dehydrogenase methenyltetrahydrofolate cyclohydrolase/formyltetrahydrofolate synthetase is a maternal genetic risk factor for neural tube defects. Am Soc Hum Genet 2002;71:1207-15. 
|
| 33. | Johanning GL, Wenstrom KD, Tamura T. Changes in frequencies of heterozygous thermolabile 5, 10-methylenetetrahydrofolate reductase gene in fetuses with neural tube defects. J Med Genet 2002;39:366-7. 
|
| 34. | Brody LC, Baker PJ, Chines PS, Musick A, Molloy AM, Swanson DA, et al. Methionine synthase: High-resolution mapping of the human gene and evaluation as a candidate locus for neural tube defects. Mol Genet Metab 1999;67:324-33. 
|
| 35. | Christensen B, Arbour L, Tran P, Leclerc D, Sabbaghian N, Platt R, et al. Enetic polymorphisms in methylenetetrahydrofolate reductase and methionine synthase, folate levels in red blood cells, and risk of neural tube defects. Am J Med Genet 1999;84:151-7. 
|
| 36. | Gueant-Rodriguez RM, Rendeli C, Namour B, Venuti L, Romano A, Anello G, et al. Transcobalamin and methionine synthase reductase mutated polymorphisms aggravate the risk of neural tube defects in humans. Neurosci Lett 2003;344:189-92. 
|
| 37. | Greene ND, Stanier P, Copp AJ. Genetics of human neural tube defects. Hum Mole Genet 2009;18:R113-29. 
|
| 38. | Al Farra HY. Methionine synthase polymorphisms (MTR 2756 A>G and MTR 2758 C>G) frequencies and distribution in the Jordanian population and their correlation with neural tube defects in the population of the northern part of Jordan. Indian J Hum Genet 2010;16:72-7. 
|
| 39. | Kibar Z, Capra V, Gros P. Toward understanding the genetic basis of neural tube defects. Clin Genet 2007;71:295-310. 
|
| 40. | Franke B, Vermeulen SH, Steegers-Theunissen RP, Coenen MJ, Schijvenaars MM, Scheffer H, et al. An association study of 45 folate-related genes in spina bifida: Involvement of cubilin (CUBN) and tRNA aspartic acid methyltransferase 1 (TRDMT1). Birth Defects Res A Clin Mol Teratol 2009;85:216-26. 
|
[Figure 1], [Figure 2]
[Table 1]
|






