|
 
 |
|
ORIGINAL ARTICLE |
|
|
|
| Year : 2012 | Volume
: 18
| Issue : 1 | Page : 75-82 |
| |
Prenatal sonographic evaluation and postnatal outcome of renal anomalies
Manisha Kumar1, Usha Gupta1, Seema Thakur2, Shilpi Aggrawal3, Jyoti Meena1, Sumedha Sharma1, Shubha S Trivedi1
1 Department of Obstetrics and Gynecology, Lady Hardinge Medical College, New Delhi, India
2 Department of Genetics, Fortis La Femme Hospital, India
3 Department of Pathology, Lady Hardinge Medical College, New Delhi, India
| Date of Web Publication | 26-May-2012 |
Correspondence Address:
Manisha Kumar
Department of Obstetrics and Gynecology, Lady Hardinge Medical College and SSK Hospital, New Delhi
India
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0971-6866.96656

 Abstract Abstract | | |
Objective: To determine the prognosis of antenatally detected renal anomalies by sonographic evaluation.
Materials and Methods: This was a follow-up study of all antenatally detected renal anomalies from January 2008 to Dec 2009 referred to fetal medicine clinic. Prenatal evaluation was done and cases were divided into four groups depending upon their prenatal sonographic findings. Post natal follow-up was done up to one year in cases of live babies. Autopsy was carried out in still born fetus after consent.
Results: The renal anomaly was detected in 55 cases, which were fully followed. The prognosis was said to be poor for group I cases with gross extra renal anomaly along with the renal anomaly, and for group II in which there was organic renal pathology with loss of renal function suggested by non-visualization of bladder and almost absent liquor. Prognosis was guarded and depended upon the gestational age of presentation in group III, which had obstructive uropathy; prognosis was good in group IV cases, which were mild, unilateral or which presented late.
Conclusion: Prenatal sonographic evaluation gives reasonably accurate picture of the prognosis and can be very helpful in counseling the parents regarding prognosis and help in deciding the timing and route of delivery.
Keywords: Postnatal outcome, prenatal diagnosis, prognosis, renal anomaly
How to cite this article:
Kumar M, Gupta U, Thakur S, Aggrawal S, Meena J, Sharma S, Trivedi SS. Prenatal sonographic evaluation and postnatal outcome of renal anomalies. Indian J Hum Genet 2012;18:75-82 |
How to cite this URL:
Kumar M, Gupta U, Thakur S, Aggrawal S, Meena J, Sharma S, Trivedi SS. Prenatal sonographic evaluation and postnatal outcome of renal anomalies. Indian J Hum Genet [serial online] 2012 [cited 2016 Jun 1];18:75-82. Available from: http://www.ijhg.com/text.asp?2012/18/1/75/96656 |
 Introduction Introduction | |  |
Ultrasonography has become a standard part of prenatal care. Around one percent of the scan will reveal fetal anomaly. Whenever such an anomaly is diagnosed it is the duty of the caregiver to provide accurate information about the findings as quickly as possible.
Urinary tract abnormalities account for 15-20% of all congenital anomalies. [1],[2] Although prenatal diagnosis of urinary tract anomalies is relatively easy (detection rate of 89%) based on sonographic images corresponding to dilated urinary tract, using the sonographic finding to provide prognostic counseling to the couple is a difficult task. Counseling regarding prognosis becomes a dilemma for obstetricians and pediatric nephrologists and urologists more so as many anomalies may be manifested late in the second trimester. Data on antenatal diagnosis and post-natal follow-up is important for assessing prognosis and hence counseling of parents.
There are many published studies evaluating the use of fetal urinary metabolites in prospectively predicting postnatal renal function; however, a recently published systematic review evaluating the diagnostic ability of fetal urinary analytes to predict outcome concluded that there was insufficient evidence to commend such investigation. [3] There is conflicting data on ultrasound finding in predicting outcome. Previous papers have reported that early gestational age at diagnosis by USG, renal parencymal cystic appearance and echogenicity, and severe oligohydramnios are associated with good predictive accuracy. [4],[5] However no consensus exists on most specific ultrasound parameter or combination of features that prospectively predict postnatal renal function. This may be because of heterogeneity of previous studies or may be due to retrospective study design of previous studies.
The objective of the study was to do prenatal sonographic evaluation regarding renal function impairment after diagnosis and to provide prognostic counseling accordingly. Postnatal correlation was done in all cases in order to see the accuracy of prognostic counseling. The outcome of the study was to provide better counseling for women and families dealing with prenatally diagnosed renal anomalies.
 Material and Methods Material and Methods | |  |
It was a prospective study. All patients with prenatally detected renal malformation by ultrasound referred to the fetal medicine OPD for first 2 years of the 3-year study period (Jan 2008 - Dec 2010) were included. After diagnosis women underwent targeted scanning for appropriate counseling regarding prognosis, ultrasound was done especially with respect to rule out other congenital malformations, to see the renal involvement whether unilateral or bilateral, the amount of liquor, bladder visualization and cortical differentiation. A follow-up scan was done to observe the evolution of the anomaly. Fetal echocardiography was also done. Relevant maternal investigations were done.
In women with gestation less than 20 weeks having gross renal anomaly in fetus, termination was offered. In gestation more than 20 weeks, pediatric surgery referral was taken. Counseling by geneticist was done, depending upon the prenatal evaluation findings. All the cases were divided into 4 groups. The fetuses with suspected major extra renal malformations along with renal malformation were grouped as Group I. In cases with bilateral renal malformation, we looked for sonographic findings suggesting functioning kidneys by seeing the amount of liquor and visualization of bladder, if the cases had oligohydramnios and non-visualization of bladder showing poorly functioning kidney, they were grouped as group II. Group III constituted those fetuses with bilateral renal malformation, oligohydramnios but bladder seen with or without presence of corticomedullary differentiation. In group IV were fetuses with unilateral or mild bilateral renal affection, shown by corticomedullary differentiation present, with slightly decreased or normal liquor, bladder was visualized. Termination was offered in group I and group II women between 21 and 24 weeks having lethal syndromic etiology as the prognosis was poor. Rest cases were followed at regular intervals (USG every 2-3 weekly) to detect the course of the disease.
Postnatal follow-up was done to see the accuracy of the prenatal evaluation. The cases in which there was stillbirth or termination of pregnancy, fetal autopsy was done according to the routinely followed protocol. All post-mortem examinations were carried out with written consent. This included a photograph, X-ray of fetus (AP and lateral), external and internal examination including histopathological examination of the kidneys and other viscera. The chromosomal analysis was done whenever fetal sample was available and the parents gave consent. All live born babies underwent ultrasound within 3-5 days of birth and renal function tests were done. The babies were followed up after 1 month, 6 months and one year, 2 years after delivery; minimum period of follow-up was one year.
 Results Results | |  |
Out of 24,160 deliveries, there were 422 cases (1.8%) with gross congenital anomaly registered in the study period; there were 63 cases with renal anomaly (14.9%). There were 8 cases, which were lost to follow-up and total 55 cases were fully followed up. Diagnosis was done at less than 20 weeks (mean 19 weeks) in 9 cases (16.4%), Termination of pregnancy was offered in them as the anomaly was severe. Fetal autopsy was done after termination of pregnancy in 8 cases, and diagnosis was confirmed in all of them [Table 1].
There were 46 cases in which diagnosis was done after 20 weeks (83.6%), after targeted scan women were divided into groups according to the findings on prenatal evaluation. The women in group I (11 cases) had suspected gross extra renal malformations; the mean gestational age was 31weeks. They were counseled regarding poor prognosis in view of the findings. Termination was offered in 4 cases, which had suspected lethal syndromic etiology and who presented before 24 weeks [Figure 1] and [Figure 2]. There were 3 live births, all of them died within hours to 2 days after delivery. Autopsy was done in 9 cases. Lower segment cesarean section (LSCS) was done in 3 cases for maternal indication only (one case each of placenta previa, previous 2 LSCS and transverse lie) [Table 2].  | Figure 1: Ultrasound showing large cyst in abdomen. Autopsy picture showing with large abdomen with thinned out abdominal wall. Internal examination showed it to be bladder. Baby had urethral atresia (Case 13)
Click here to view |
 | Figure 2: Ultrasound picture of limb body wall defect with enlarged cystic kidney. Autopsy picture confirming the same (Case 19)
Click here to view |
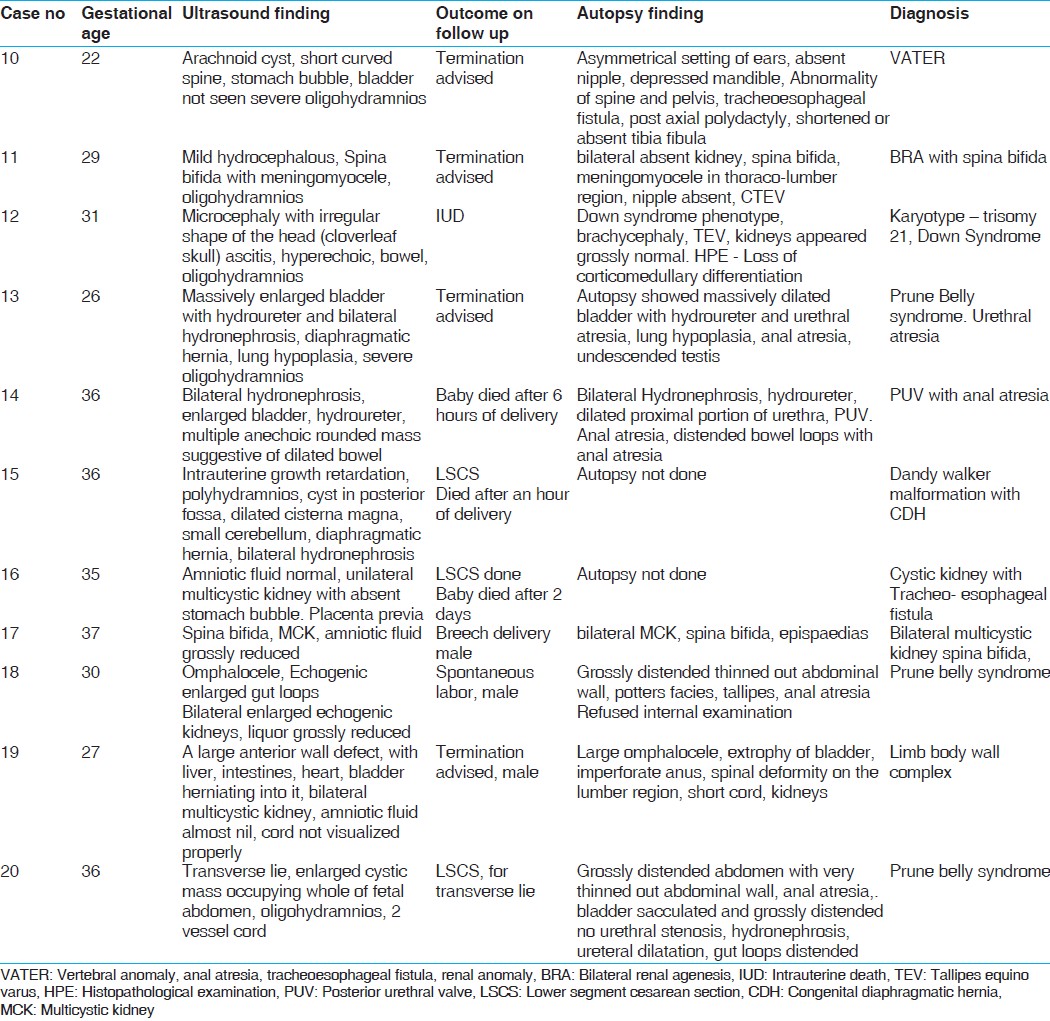 | Table 2: Fetus of more than 20 weeks gestation with gross extra renal anomaly
Click here to view |
The women who belonged to group II were also counseled that the prognosis was poor as the renal function seemed to be impaired as bladder was not seen and liquor was reduced. There were 13 cases in this group, mainly cases with bilateral cystic kidneys; mean gestational age was 27 weeks. There were 5 live births, but all of them died within days of delivery, one survived till 3 months and then succumbed to renal failure [Table 3]. LSCS was done in one case for fetal distress (case no 27). The baby later died after 2 days due to respiratory distress and renal failure. Autopsy was done in 6 cases. Histopathology confirmed multicystic kidney in 5 and autosomal recessive polycystic kidney disease (ARPKD) in one fetus. In one patient with positive family history (case 21), the ultrasound finding of bright echogenic kidney was diagnosed on histopathology as multicystic kidney, showing the possibility of familial multicystic kidney disease [Figure 3]. 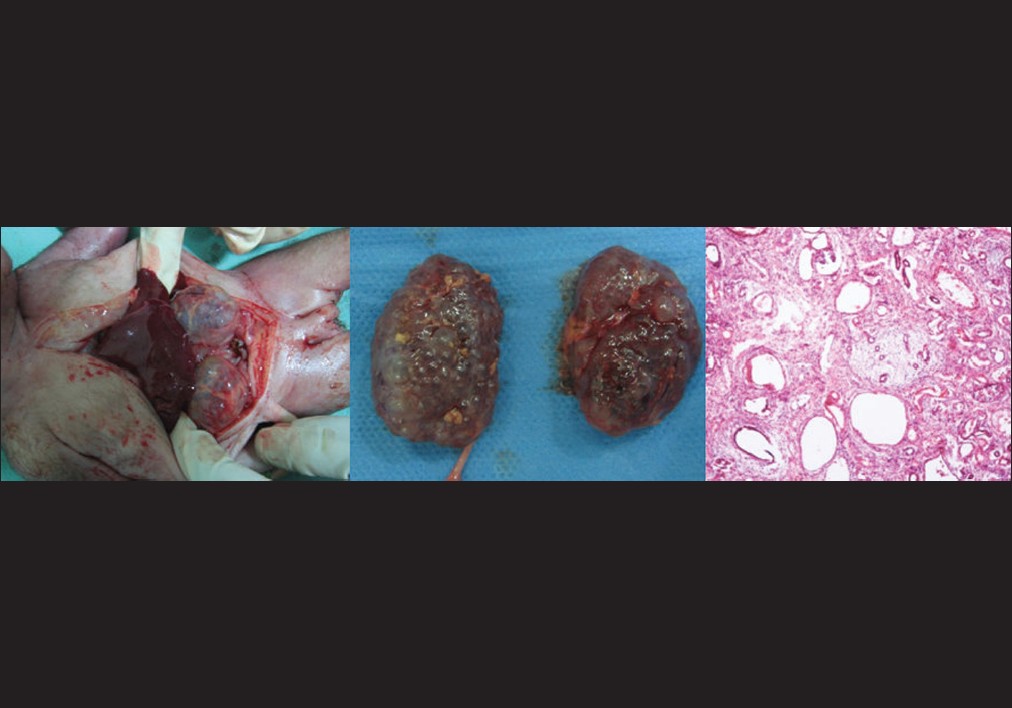 | Figure 3: Case 21, with positive family history and bilateral echogenic kidneys on USG, autopsy showing cysts of varying sizes on autopsy, histopathology confirmed it to be multicystic kidney
Click here to view |
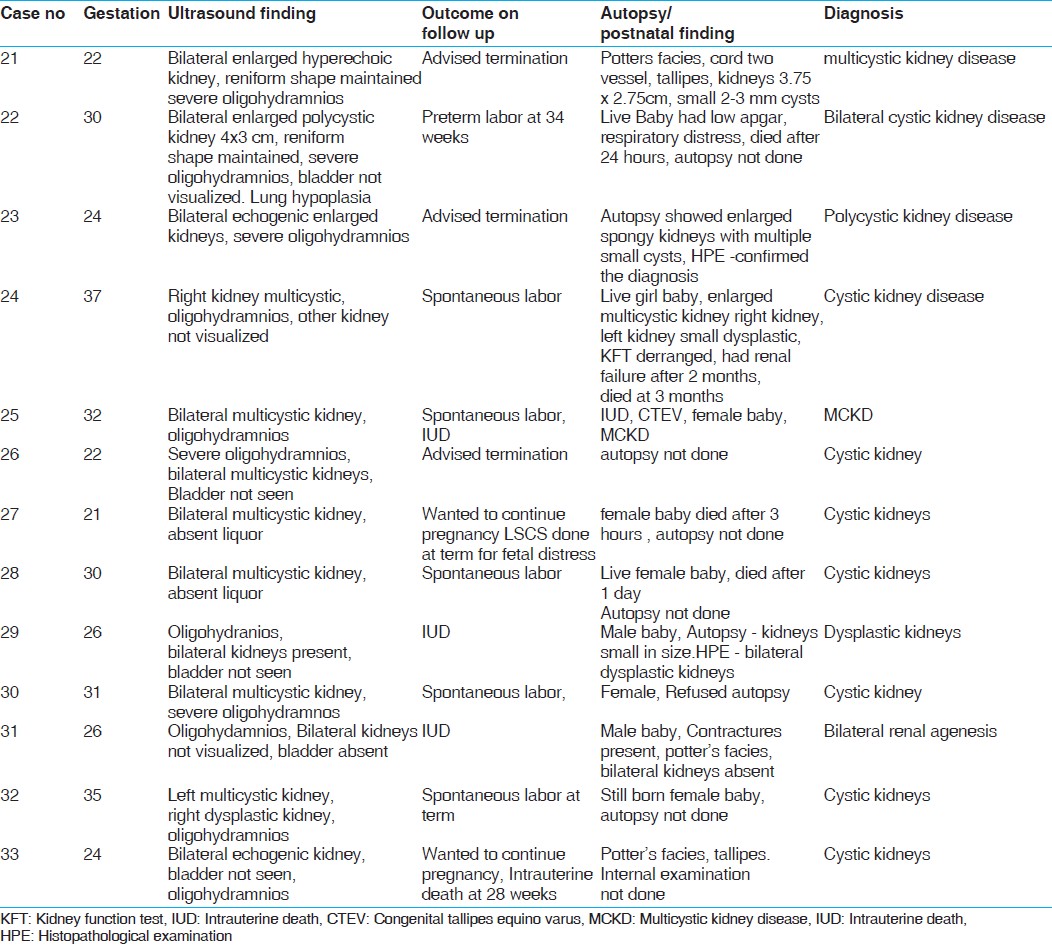 | Table 3: Fetus of more than 20 weeks gestation with oligohydramnios and bladder not visualized
Click here to view |
In women of group III (9 cases), there was mainly lower urinary tract obstruction [Table 4], in this group prognosis chiefly depended upon the gestational age of diagnosis, renal cortical appearance, and degree of oligohydramnios. The mean gestational age was 31 weeks, 5 cases survived after delivery, 2 had vesicouretral reflux, 3 underwent surgery, and one baby had deteriorating renal function. The diagnosis was after 32 weeks and renal cortical appearance was preserved in all cases that survived. LSCS was done in one case for fetal indication. Autopsy was done in all 4 cases which were stillborn [Figure 4]. There was posterior urethral valve in 3 cases and urethral atresia in one case. | Figure 4: Ultrasound picture of bilateral hydronephrosis with enlarged bladder and typical keyhole sign. autopsy confirming the finding (Case 24)
Click here to view |
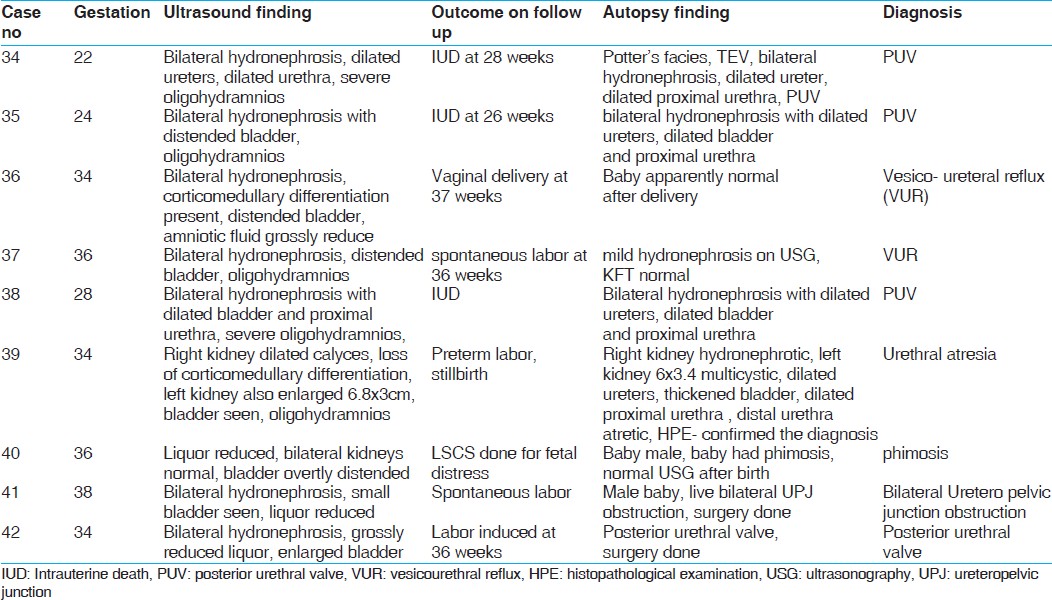 | Table 4: Fetus of more than 20 weeks gestation with bilateral renal involvement, oligohydramnios and bladder visualized
Click here to view |
Group IV consisted of total 13 cases, they had unilateral (7 cases) or bilateral affection (6 cases) with mild oligohydramnios or normal liquor, and bladder was seen in all cases [Table 5]. They were counseled that the prognosis was good and follow-up was required, the mean gestational age of presentation was 34 weeks. All of them were delivered live; LSCS was done for fetal indication in 2 of them. Kidney function test in all but one were normal although the ultrasound after delivery showed mild hydronephrosis persisting in 5 of them; 2 babies underwent surgery. 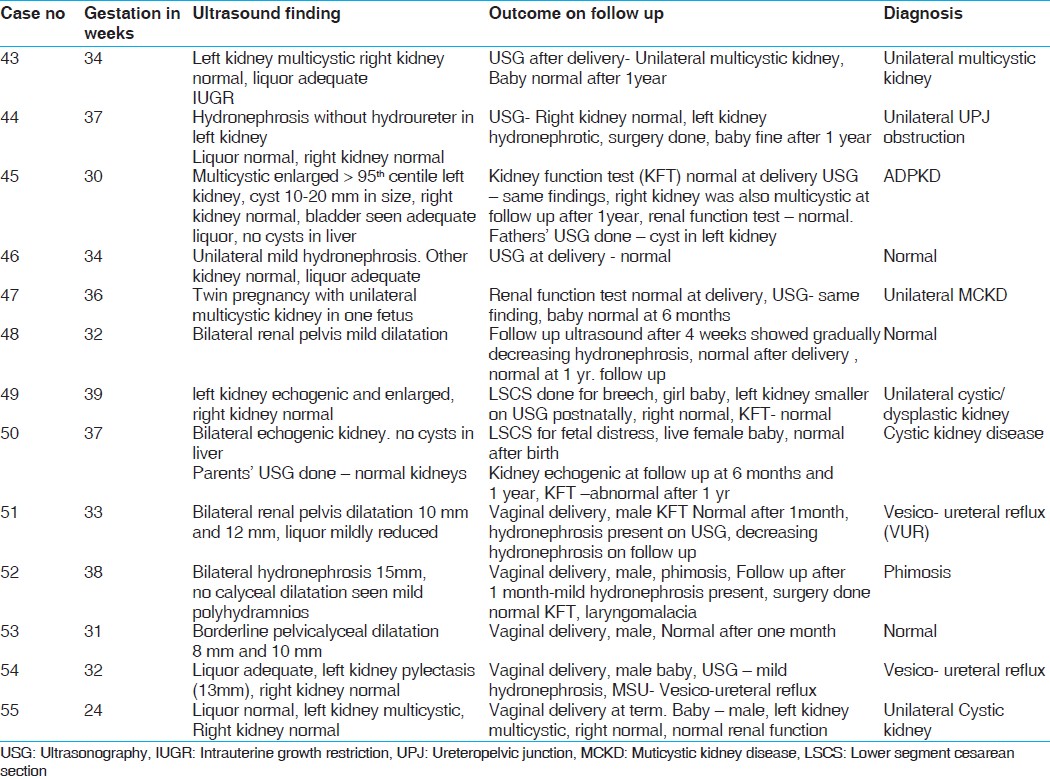 | Table 5: Fetus with unilateral or bilateral renal involvement, normal or slightly reduced liquor with normal bladder
Click here to view |
Autopsy was done in 27 cases out of total 29 stillbirths. There was extra renal anomaly present in 15 cases (27.3%). Chromosomal analysis was done in 10 cases and this was abnormal in 3 cases; in all 3 cases there were extra renal malformation as well. Out of the total 55 cases, 17 survived (32.1%), surgery was done postnatally in 5 cases.
 Discussion Discussion | |  |
Renal malformations are detected in 0.2-2% of all newborns. [6] The fetal kidneys and adrenal glands can be visualized by transabdominal ultrasound between the 12-15 th week of gestation. Medulla and cortex can be differentiated well by the 20-25 th week of gestation. [7] Ultrasound is a very effective diagnostic modality for identifying fetal urinary tract anomalies. But once the abnormality is diagnosed it is equally important to delineate the prognosis of malformation.
Our criteria for determining the prognosis of the malformation was based on evaluation of sonographic findings suggesting functioning kidneys to find out the severity of the disease. The cases in group I with associated extra renal malformation had poor prognosis for survival. LSCS in this group was only performed for maternal indications (3 cases). Detection of any renal malformation should warrant a detailed examination of the fetus for other structural anomalies. Associated anomaly in our study was 27.3%, other studies have reported the incidence of up to 50 %. [8] Chromosomal studies on amniotic fluid should be offered in cases with renal malformation; the incidence of chromosomal abnormality in our study was 5.5%, and the incidence in other studies has reported to be 8-12%. [9],[10] The incidence of chromosomal abnormality was low in our study population as many parents did not opt for the test.
The cases in which there were structural abnormality in kidneys coupled with loss of function, apparent in terms of non-visualization of bladder and absent or severely decreased liquor, the prognosis was believed to be poor and on follow-up none of the babies survived. Severe oligohydramnios and non-visualization of urinary bladder is associated with poor renal function. Fetal autopsy after termination of pregnancy is important to arrive at a definitive diagnosis. It may be difficult to detect bilateral renal agenesis on USG due to severe oligohydramnios and fetal autopsy is necessary to confirm renal agenesis and also any other associated malformation. This will help in counseling for next pregnancy. In cases where there was lower urinary tract obstruction but the kidneys were functioning, prognosis depended upon the gestational age at presentation. Almost all who survived presented after 34 weeks; it helped in timing of delivery, with induction done at 37 weeks to salvage the kidneys if possible. Ultrasound diagnosis when made early helps in the timing of delivery and also the route of delivery and early treatment. [9]
We did not attempt prenatal bladder drainage but the recent review on effectiveness of antenatal intervention for treatment of congenital lower urinary tract obstruction done by Morris et al., concluded that although bladder drainage improves survival but it may confer a high residual risk of poor postnatal renal function. [11] In group IV, the cases were mild, renal function was preserved, as shown by appearance of normal liquor and normal bladder. The antenatal screening in these cases helps in follow-up and helps in early detection of anomaly. Though many believe that the detection of mild dilatation have no therapeutic clinical significance and causes undue anxiety in many cases, in such situation they may be counseled and reassured that they may expect a healthy child with possibly minor problems without consequences for life and renal function. [9]
Some authors suggest that the risk of surgery is minimal when the dilatation is less than 10 mm in late pregnancy. [12],[13] Thomas et al., suggested that prenatal dilatation is not a sensitive indicator of pathology but increasing dilatation is associated with morbidity and mortality. [14]
Our prognostication was reasonably accurate in terms of preparing the couple and the physicians dealing with the case to the outcome of the anomaly. The criteria was simple and not too complicated so it was easy for the obstetrician dealing with the case to interpret them and counsel accordingly. The categorization helped them to take decision regarding route of delivery especially in severe cases, in timing of delivery particularly in cases which were gradually worsening and in post natal follow-up of mild cases.
Although we followed the babies postnatally for one year, prolonged follow-up of these cases would have been more useful and would have given even better estimate of renal function.
 Conclusion Conclusion | |  |
Renal malformations are commonly detected on antenatal ultrasound. Prognosis varies upon the type of malformation and associated malformations. The antenatal sonographic evaluation and counseling helps in delineating the prognosis and thus helping the couple to make reproductive decision. Pregnancy can be terminated in cases of lethal abnormality, if diagnosed early. The authors report no conflict of interest.
 References References | |  |
| 1. | Grandjean H, Larroque D, Levi S; The Eurofetus study group. The performance of routine ultrasonographic screening of pregnancies in Eurofetus study. Am J Obstet Gynecol 1999;181:446-54. 
|
| 2. | Levi S. Mass screening for fetal malformations: The Eurofetus study. Ultrasound Obstet Gynacol 2003;22:555-8. 
|
| 3. | Morris RK, Quinlan- Jones E, Kilby MD, Khan KS. Systematic review of accuracy of fetal urine analysis to predict poor postnatal renal function in cases of congenital urinary tract obstruction. Prenat Diagn 2007;27:900-11. 
|
| 4. | Robyr R, Benachi A, Ikha-Dahmane E, Martinovich J, Dumez Y, Ville Y. Correlation between ultrasound and anatomical findings in foetuses with lower urinary tract obstruction in the first half of pregnancy. Ultrasound Obstet Gynacol 2005;25:478-82. 
|
| 5. | Oliveira EA, Diniz JS, Cabral AC, Pereira AK, Leite HV, Colosimo EA, et al. Predictive factors of fetal urethral obstruction: A multivariate analysis. Fetal Diagn Ther 2000;15:180-6. 
[PUBMED] |
| 6. | Riccipetitoni G, Chierici R, Tamisari L, De Castro R, Manfredi S, Veroni G, et al. Postnatal ultrasound screening of urinary malformations. Urology 1992;148:604-5. 
|
| 7. | Rouse GA, Kaminsky CK, Saaty HP, Grube GL, Fritzsche PJ. Concepts in sonographic diagnosis of fetal renal disease. Radiographics 1988;8:119-32. 
[PUBMED] [FULLTEXT] |
| 8. | Isaken CV, Eik-Nes SH, Blaas HG, Torp SH. Fetuses and infants with congenital urinary system anomalies: Correlation between prenatal ultrasound and Postmortem findings. Ultrasound Obstet Gynecol 2000;15:177-85. 
|
| 9. | Damen-Elias HA, De Jong TP, Stigter RH, Visser GH, Stoutenbeek PH. Congenital renal tract anomalies: Outcome and follow up of 402 cases detected antenatally between 1986 and 2001. Ultrasound Obstet Gynecol 2005;25:134-43. 
[PUBMED] [FULLTEXT] |
| 10. | Nicolaides KH. Screening for chromosomal defects. Ultrasound Obstet Gynecol 2003;15:177-85. 
|
| 11. | Morris RK, Malin GL, Khan KS, Kilby MD. Antenatal ultrasound to predict postnatal renal function in congenital lower urinary tract obstruction: Systematic review to test accuracy. BJOG 2009;116:1290-9. 
[PUBMED] [FULLTEXT] |
| 12. | Sairam S, Al-Habib A, Sasson S, Thilaganathan B. Natural history of fetal hydronephrosis diagnosed on mid-trimester ultrasound. Ultrasound Obstet Gynecol 2001;17:191-6. 
[PUBMED] [FULLTEXT] |
| 13. | Dremsek PA, Gindl K, Voitl P, Strobl R, Hafner E, Geissler W, et al. Renal pyelectasis in fetuses and neonates: Diagnostic value of renal pelvis diameter in pre and postnatal sonographic screening. AJR Am J Roentgenol 1997;168:1017-9. 
[PUBMED] [FULLTEXT] |
| 14. | Thomas DF. Prenatal diagnosis: Does it alter outcome? Prenat Diagn 2001;21:1004-11. 
[PUBMED] [FULLTEXT] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
|






