|
 
 |
|
LETTER TO THE EDITOR |
|
|
|
| Year : 2012 | Volume
: 18
| Issue : 3 | Page : 380-382 |
| |
Chronic pancreatitis: A new pathophysiology
Shweta Singh1, Ravindra Kumar1, Gourdas Choudhuri2, Sarita Agarwal1
1 Department of Genetics, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
2 Department of Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
| Date of Web Publication | 4-Mar-2013 |
Correspondence Address:
Sarita Agarwal
Department of Genetics, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow - 226 014, Uttar Pradesh
India
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0971-6866.108056

How to cite this article:
Singh S, Kumar R, Choudhuri G, Agarwal S. Chronic pancreatitis: A new pathophysiology. Indian J Hum Genet 2012;18:380-2 |
Sir,
The pathological hallmarks of chronic pancreatits are inflamation, gandular atrophy, ductal changes and fibrosis. Alcohol is the most common etiology of chronic pancreatitis, but it is likely that mutiple genetic and environmental cofactors interact to produce expression of disease in a given individual. [1] Here, we describe a case of alcoholic chronic pancreatitis with hemoglobinopathy. The proband visited the Gastroenterology OPD with a complaint of severe pain in the abdomen and obstipation.The proband had a history of alcohol intake of approx 150 mL per week since 20 years of age. Radiographic image [Figure 1]a showed heterogeneously enhancing pancreas in the region of the head, body and tail, with multiple hypodense necrotic areas in the pancreatic parenchyma. He had sepsis, which responded slowly to meropenem. He had no respiratory failure or renal faliure. He was clinically diagnosed as a case of alcoholic chronic pancreatitis. Lipid profile values of the proband were as follows: Triglyceride = 114 mg/dL, total cholesterol = 100 mg/dL, HDL cholesterol = 27 mg/dL, LDL cholesterol = 50 mg/dL and VLDL cholesterol = 23 mg/dL. Liver function tests showed Serum Aspartate transaminase = 30 U/L, Serum alanine transaminase = 25 U/L and Alkaline phosphatase = 97 U/L, and the Serum amylase level were found to be 577 U/L.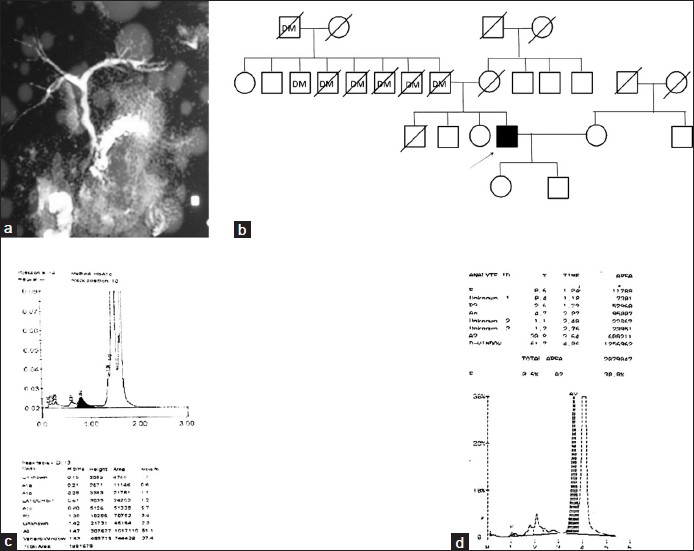 | Figure 1: (a) Contrast enhanced computed tomography image of proband showing necrosis in pancreas, (b) Pedigree of family showing family history of diabetes mellitius type II, (c) HbA1c chromatogram of proband showing abnormal pattern, (d) HPLC chromatogram of proband showing presence of HbE and HbD
Click here to view |
Because his family had a history of DM type II [Figure 1]b, the proband was also evaluated for the same. Fasting serum glucose levels were found to be normal (77 mg/dL), but we found abnormal values of HbA1c that did not correlate with the glucose levels [Figure 1]c. The patient was referred to the Department of Genetics for evaluation of hemoglobin variant analysis as Little et al.[2] showed that HbE and HbD interfere with the measurement of HbA1c. The hematological investigations of the proband revealed Hb = 4.9 g/dL, MCV = 70.2 fl, MCH = 24.1 pg and MCHC = 34.3% with 0.5% reticulocytosis. Analysis on CE-HPLC (Bio-rad Hb variant) revealed the presence of HbE and HbD [Figure 1]d. We further confirmed the presence of HbE and HbD by ARMS-PCR as described by Agarwal et al. [3] This is the first report in the literature that indicates the presence of these two variants together.
Because the patient was diagnosed as a case of chronic pancreatitis, molecular analysis was performed for common SPINK1 gene [4] and CFTR gene [5] mutations using PCR. The patient was found to be compound heterozygous for SPINK1 gene mutation (N34S and IVS3 + 2(T-C)) and heterozygous for CFTR gene [G551D/N]. A family study was conducted and both offspring were found as trait for HbE. His daughter also carried the G551D mutation in heterozygous state. Both his brother and his wife were found to be normal on hemoglobin variant analysis. There was no family history of pancreatitis.
The most likely mechanism of alcohol-induced chronic pancreatitis is the oxidative damage of acinar cells of pancreas, [1] and, in this present case, the oxidative stress is further increased by the presence of two abnormal Hb variants. The HbE and HbD variants with low oxgen affinity produce the condition of hypoxia in tissue. Hypoxia can decrease the ability of cells to detoxify free radicals, subsequently increasing tissue damage and functional impairment. Ahmed et al.[6] also showed a case of pancreatitis with sickle cell disease.
N34S mutation of SPINK1 was associated with various types of pancreatitis, and has been hypothesized as a disease-modifying factor due to its presence in normal individuals, with a prevalence of 1-2%. [7] Moreover, there is no clear phenotypic difference between individuals who are homozygous and those who are heterozygous for the N34S mutation. IVS3+2T-C mutation affects the consensus splicing donor site at intron 3 resulting in skipping of whole exon 3. Thus, IVS3+2T-C mutation results in functional loss of SPINK1 and disturbs the protease/antiprotease balance within the pancreas leading to the development of the pancreatitis. [8]
Although it is well known that chronic pancreatitis is predisposed by heterozygosity for CFTR mutations, little is known about the combination of CFTR mutations with SPINK1 mutations. To date, only a few cases have demonstrated that pancreatitis is caused by simultaneous CFTR and SPINK1 mutations. No information concerning clinical features of these patients is available. [9]
This is the first report that shows the clinical features of chronic pancreatits with HbE and HbD.
In conclusion, pancreatitis is a multifactorial disease and N34S/IVS3+2T-C and G551D/N, together with HbE and HbD, act as a modifier in the disease development.
 Acknowledgment Acknowledgment | |  |
The authors would like to thank the Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS), Lucknow, India, for providing them with the infrastructural facilities. SS is thankful to DST, New Delhi, for her fellowship.
 References References | |  |
| 1. | Chaudhary P, Gupta P. Pathophysiology of alcoholic pancreatitis: An overview. World J Gastroenterol 2006;12:7421-7. 
|
| 2. | Little RR, Rohlfing CL, Hanson S, Connolly S, Higgins T, Weykamp CW, et al. Effects of hemoglobin (Hb) E and HbD traits on measurements of glycated Hb (HbA1c) by 23 Methods. Clin Chem 2008;54:1277-82. 
[PUBMED] |
| 3. | Agarwal S, Pradhan M, Gupta UR, Sarwai S, Agarwal SS. Geographic and ethnic distribution of beta-thalassaemia mutations in Uttar Pradesh. Hemoglobin 2000;24:89-97. 
[PUBMED] |
| 4. | Plendl H, Siebert R, Steinemann D, Grote W. High frequency of the N34S mutation in the SPINK1 gene in chronic pancreatitis detected by a new PCR-RFLP assay. Am J Med Genet 2001;100:252-3. 
[PUBMED] |
| 5. | Ferrie RM, Schwarz MJ, Robertson NH, Vaudin S, Super M, Malone G, et al. Development, multiplexing and application of ARMS tests for common mutations in the CFTR gene. Am J Hum Genet 1992;51:251-62. 
[PUBMED] |
| 6. | Ahmed S, Siddiqui AK, Siddiqui RK, Kimpo M, Russo L, Mattana J. Acute pancreatitis during sickle cell vaso-occlusive painful crisis. Am J Hematol 2003;73:190-3. 
[PUBMED] |
| 7. | Witt H, Luck W, Hennies HC, Classen M, Kage A, Lass U, et al. Mutations in the gene encoding the serine protease inhibitor, Kazal type 1 are associated with chronic pancreatitis. Nat Genet 2000;25:213-6. 
[PUBMED] |
| 8. | Ota Y, Masamune A, Inui K, Kume K, Shimosegawa T, Kikuyama M. Phenotypic variability of the homozygous IVS3+2T>C mutation in the serine protease inhibitor Kazal type 1 (SPINK1) gene in patients with chronic pancreatitis. Tohoku J Exp Med 2010;221:197-201. 
[PUBMED] |
| 9. | Ellis I. Genetic counseling for hereditary pancreatitis the role of molecular genetics testing for the cationic trypsinogen gene, cystic fibrosis and serine protease inhibitor Kazal type 1. Gastroenterol Clin N Am 2004;33:839-54. 
|
[Figure 1]
|






