| |


 |
| Year : 2011 | Volume
: 5
| Issue : 3 | Page : 81-84 |
|
|
|
|
|
CASE REPORT Isolated supraspinatus muscle atrophy and fatty infiltration associated with recurrent anterior shoulder instability: A case report and review of the literature
Abdulaziz Z Alomar1, Tom Powell2, Mark L Burman3
1 Department of Orthopaedic Surgery, College of Medicine, King Saud University, Riyadh, Saudi Arabia
2 Department of Radiology, McGill University, Montreal, Quebec, Canada
3 Department of Orthopaedic Surgery, McGill University, Montreal, Quebec, Canada
Correspondence Address:
Abdulaziz Z Alomar
Department of Orthopaedic Surgery, College of Medicine, King Saud University, P.O. Box 7805, Riyadh 11472
Saudi Arabia
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.86246

|
|
|
|
| Date of Web Publication | 17-Oct-2011 |
 Abstract Abstract | | |
Supraspinatus muscle atrophy and fatty infiltration are two distinct muscle abnormalities which can be seen after a chronic massive tear or suprascapular neuropathy. Isolated supraspinatus muscle denervation due to suprascapular nerve injury after shoulder dislocation is extremely rare.
We report on a patient who developed isolated supraspinatus muscle atrophy and fatty infiltration after traumatic anterior shoulder instability. Possible explanations and etiologies of this rare condition are discussed in this report.
Keywords: Fatty infiltration, supraspinatus atrophy, suprascapular neuropathy, shoulder instability
How to cite this article:
Alomar AZ, Powell T, Burman ML. Isolated supraspinatus muscle atrophy and fatty infiltration associated with recurrent anterior shoulder instability: A case report and review of the literature. Int J Shoulder Surg 2011;5:81-4 |
How to cite this URL:
Alomar AZ, Powell T, Burman ML. Isolated supraspinatus muscle atrophy and fatty infiltration associated with recurrent anterior shoulder instability: A case report and review of the literature. Int J Shoulder Surg [serial online] 2011 [cited 2016 Apr 25];5:81-4. Available from: http://www.internationalshoulderjournal.org/text.asp?2011/5/3/81/86246 |
 Introduction Introduction | |  |
Muscle atrophy (reduced muscle bulk) is a nonspecific sign, and it may occur as a consequence of muscle disuse, tendon tear, or denervation.
Fatty infiltration (replacement of muscle fibers by fat) is mostly seen in association of chronic, massive rotator cuff tear. However, supraspinatus muscle fatty infiltration can occur in the absence of any intrinsic tendon rupture as a result of suprascapular neuropathy.
Suprascapular nerve (SSN) injury associated with traumatic shoulder dislocation is most likely due to a traction injury to the nerve. [1],[2],[3] The location of SSN injury can be predicted by the pattern of the muscles' involvement. While the infraspinatus muscle is always affected, the supraspinatus muscle will be spared when the injury is at spinoglenoid notch level or distal, whereas both supra- and infraspinatus muscle denervation will occur when the injury is at the level of suprascapular notch or proximal, making the distribution of muscle involvement helpful in localizing the site of injury.
Isolated motor branch injury to supraspinatus muscle is extremely rare. In the literature, only one other case reported of isolated supraspinatus muscle paralysis following an anterior shoulder dislocation. [4]
Diagnosis is based on clinical history, physical examination, appropriate imaging, and electrodiagnostic studies. Traction injuries typically respond well to the non-operative management, whereas mass compression usually responds best to surgical decompression, and the causes of nerve dysfunction should be determined.
 Case Report Case Report | |  |
A 43-year-old female was referred for recurrent left shoulder instability. She sustained her first dislocation eight years ago, which was a traumatic anterior shoulder dislocation and has had an increasing frequency of shoulder dislocation since. She estimates this has happened about 20 times. Over the subsequent years, she has experienced multiple painful subluxation episodes that have occurred with abduction and external rotation of the shoulder. She, therefore, presented for evaluation of her condition. Otherwise, she has an unremarkable past medical history.
On physical examination, the patient had obvious left supraspinatus muscle atrophy. She had a full range of motion of her shoulder and had positive apprehension and positive relocation tests. She had a negative sulcus sign, and a negative O'Brien's sign. Rotator cuff muscles strength were within normal except for the supraspinatus muscle, which showed a significant weakness. Neurological examination of all peripheral nerves was normal, and there was no evidence of generalized ligamentous laxity.
Magnetic resonance imaging (MRI) revealed significant atrophy and diffuse fatty infiltration of the supraspinatus muscle associated with supraspinatus tendinopathy and a shallow Hill-Sachs defect. Because of associated history of instability, an MRI arthrogram was performed, which showed a Bankart lesion that could not be appreciated in the previous plain MRI. The infraspinatus muscle appeared unremarkable, and no structural lesion was apparent in the suprascapular or spinoglenoid notch or along the course of the suprascapular nerve. The rest of examination was normal [Figure 1] and [Figure 2].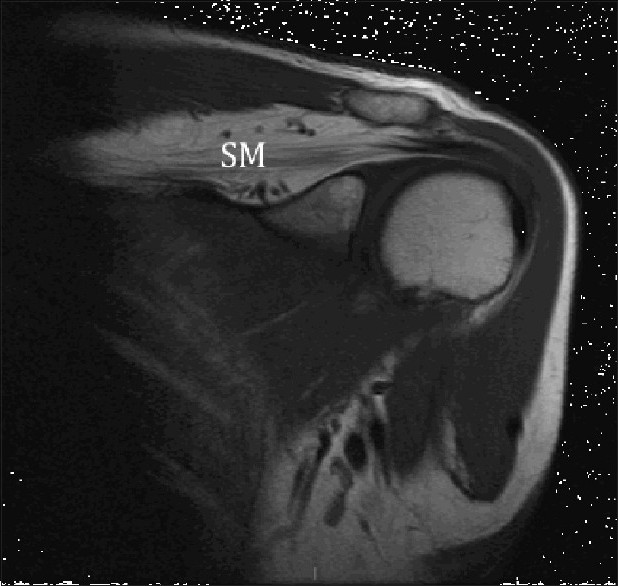 | Figure 1: Magnetic resonance imaging coronal view showing significant atrophy and fatty infiltration of the supraspinatus muscle
Click here to view |
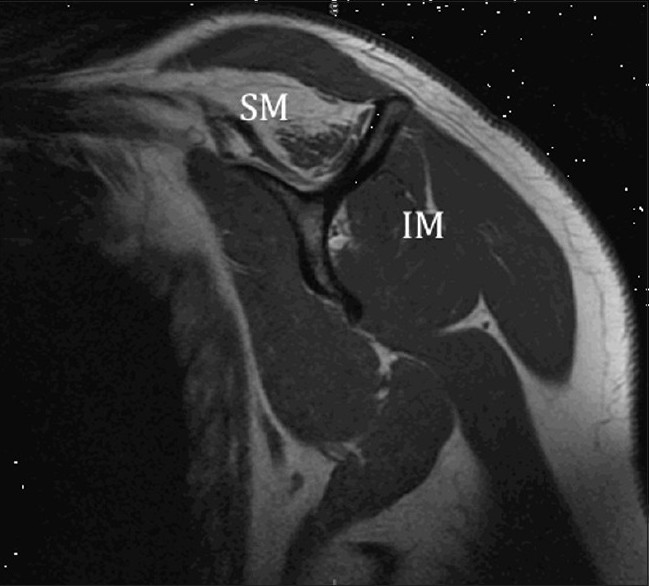 | Figure 2: Magnetic resonance imaging oblique view showing significant fatty infiltration of the supraspinatus muscle; Note the normal appearance of the infraspinatus muscle
Click here to view |
Electromyographic study showed an injury to SSN branch affecting only the supraspinatus muscle. There was no evidence of brachial plexopathy or cervical radiculopathy.
Operative treatment
Non-operative treatment failed to alleviate the patient's shoulder instability; therefore, she underwent arthroscopic Bankart repair. Arthroscopic evaluation of the shoulder joint revealed evidence of a detached anterior labrum with a flap tear of superior labrum [Figure 3] and a small Hill-Sachs lesion. The biceps anchor, supraspinatus tendon and the rest of the rotator cuff appeared normal [Figure 4].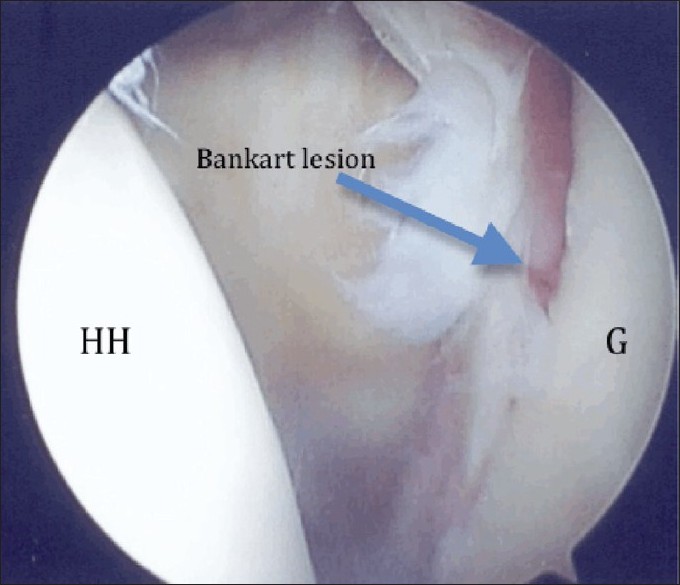 | Figure 3: Arthroscopy of the shoulder showing Bankart lesion of the glenoid (posterior portal view). HH: Humeral head, G: Glenoid
Click here to view |
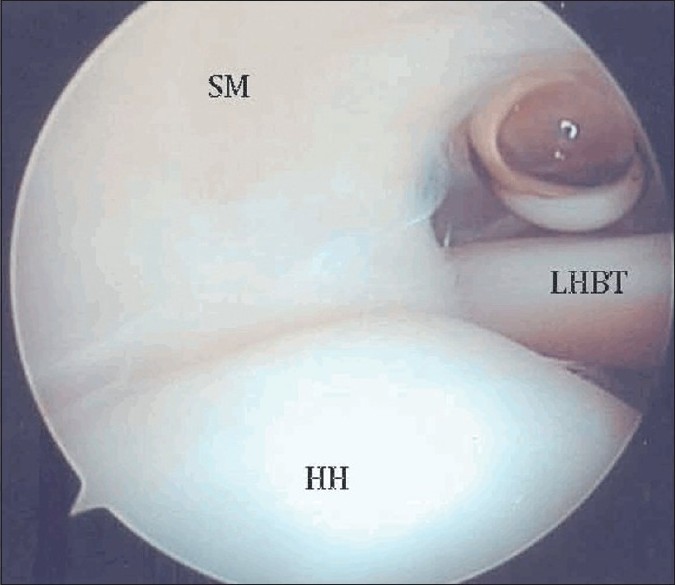 | Figure 4: Arthroscopy of the shoulder showing the normal appearance of the supraspinatus tendon (posterior portal view). HH: Humeral head, SM: Supraspinatus muscle, LHBT: Long head of biceps tendon
Click here to view |
Postoperative follow up
Postoperatively, the patient followed a post-Bankart rehabilitation program. At two-year follow-up, she reported no more instability in her left shoulder. On physical examination, she still has wasting and weakness of her supraspinatus muscle. Overall, she was satisfied with her outcome.
 Discussion Discussion | |  |
The natural history of the rotator cuff fatty infiltration associated with cuff tear is well described and reported in the literature. However, the incidence and the nature history of rotator cuff atrophy and fatty infiltration resulted from traumatic muscle denervation is still unknown and not clear in the literature.
SSN injury associated with shoulder dislocation has been described and documented in the literature. [3],[5] The reported incidence rate of SSN injury in association with anterior shoulder dislocation vary from 14% [3] to 29%. [5] However, because the infraspinatus muscle is used as a reference for SSN injury in EMG study, the true incidence of the isolated supraspinatus muscle denervation and fatty degeneration in the absence of tendon tear remains unknown, and none of these reported cases had described an isolated SSN injury to the supraspinatus muscle only.
In the literature, there is only one other case which reported of isolated nerve injury to the motor branch of SSN following an anterior shoulder dislocation. Weiland et al. [4] reported a 42-year-old female, who sustained isolated supraspinatus muscle denervation after a traumatic shoulder dislocation.
In this reported case, we think the cause of supraspinatus muscle atrophy and fatty infiltration is a traction injury to the terminal motor branches of SSN to the supraspinatus muscle resulting from traumatic anterior shoulder dislocation. The complete sparing of the infraspinatus muscle seen in this patient is an unusual and extremely rare presentation of SSN injury associated with shoulder dislocation. We propose three potential explanations for this rare phenomenon; first, the short tether motor branches to the supraspinatus muscle are more prone to injury as compared to the motor branches to the infraspinatus muscle, which are longer and larger. [6] Second, the infraspinatus muscle had three or four motor branches, where the supraspinatus had only tow motor branches as being shown by a suprascapular nerve anatomy study done by Warner et al. [6] Finally, Lee et al. [7] and Bergman et al. [8] have proposed that the axillary nerve can contribute to the innervation of the infraspinatus muscle. Bergman et al. [8] Indicates that the axillary nerve may give a branch to the long head of triceps and (or) the infraspinatus muscles. Lee [7] reported unusual infraspinatus muscle innervation. The cadaver dissection of the left side of a 65-year-old female Korean showed that the infraspinatus muscle entirely received its innervation from a branch of the axillary nerve, and SSN supply only the supraspinatus muscle.
Associated rotator cuff tear and fatty infiltration had a negative influence on the outcome of SSN injury after shoulder dislocation.
The progression of the fatty infiltration associated with cuff tear can be minimized after a successful repair; however, improvement or reversal of muscle fatty degeneration will be unlikely. [9]
While the fatty degeneration associated with traumatic peripheral nerve injury is likely to be irreversible, the time of onset and progression of the fatty infiltration after traumatic muscle denervation is still unclear yet.
When there is no rotator cuff tear or fatty infiltration, the outcome after SSN injury is favorable and full recovery can be expected. [3],[5]
In this reported case, the patient persists to exhibit some weakness and atrophy of the supraspinatus muscle even after a supervised and considerable preoperative physiotherapy and surgical treatment of her shoulder instability. Probably, this can be explained by the presence of a significant and irreversible fatty infiltration after long standing (eight years) muscle denervation. The favorable overall shoulder's function outcome which had seen with this patient is most likely due to complete preservation of the infraspinatus muscle and surgical stabilization of her shoulder.
Despite significant atrophy and fatty infiltration of the supraspinatus muscle on MRI, no visible changes were apparent arthroscopically. Further preoperative investigations like Computed tomography (CT) scan, MRI, or ultra sound of the rotator cuff will be more helpful to address the presence and the extent of fatty infiltration when supraspinatus muscle atrophy and paralysis persist.
 Conclusion Conclusion | |  |
Persistent supraspinatus muscle atrophy and weakness after traumatic anterior shoulder dislocation should be worked up to rule out associated SSN injury. Further investigations, like MRI, should be done to assess the presence and extent of fatty infiltration, which might affect the overall outcome of the treatment.
It is still largely unknown if the early recognition and surgical treatment of this condition have any role in delaying the progression of atrophy and fatty infiltration of the supraspinatus muscle.
 References References | |  |
| 1. | Gariepy R, Derome A, Laurin CA. Brachial plexus paralysis following shoulder dislocation. Can J Surg 1962;5:418-21. 
|
| 2. | Milton GW. The mechanism of circumflex and other nerve injuries in dislocation of the shoulder, and the possible mechanisms of nerve injuries during reduction of dislocation. Aust NZ Surg 1953;23:25-30. 
|
| 3. | Visser CP, Coene LN, Brand R, Tavy DL. The incidence of nerve injury in anterior dislocation of the shoulder and its influence on functional recovery: A prospective clinical and EMG study. J Bone Joint Surg Br 1999;81:679-85. 
|
| 4. | Weiland DE, MacGillivray JD. Isolated supraspinatus muscle paralysis after shoulder dislocation: A case report. Am J Sports Med 2003;31:462-4. 
|
| 5. | De Laat EA, Visser CP, Coene LN, Pahlplatz PV, Tavy DL. Nerve lesions in primary shoulder dislocations and humeral neck fractures: A prospective clinical and EMG study. J Bone Joint Surg Br 1994;76:381-3. 
|
| 6. | Warner JP, Krushell RJ, Masquelet A, Gerber C. Anatomy and relationships of the suprascapular nerve: Anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tears. J Bone Joint Surg Am 1992;74:36-45. 
|
| 7. | Lee KS. Unusual innervation of the supraspinatus and infraspinatus muscles. Clin Anat 2007;20:970-1. 
|
| 8. | Bergman RA. Compendium of human anatomic variation: Text, atlas, and world literature. Baltimore, Munich: Urban and Schwarzenberg; 1988. 
|
| 9. | Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 2007;35:719-2. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|
