| |


 |
| Year : 2012 | Volume
: 6
| Issue : 4 | Page : 112-115 |
|
|
|
|
|
ORIGINAL ARTICLE Does age or gender of the patient influence the outcome of type II superior labrum anterior and posterior repair?
Daniel Mok1, Emily L Wang2
1 Shoulder and Upper Limb Unit, Epsom & St Helier NHS Trust,Epsom General Hospital, Surrey, UK,
2 New York University School of Medicine, New York, NY 10016, USA,
Correspondence Address:
Daniel Mok
2906 Bank of America Tower, 12 Harcourt Road, Central, Hong Kong
 Source of Support: None, Conflict of Interest: Dr. Mok is a consultant
for Biomet sports medicine. The authors have not received any financial
payments or other benefits for any commercial entity related to the subject
of this article.
DOI: 10.4103/0973-6042.106223

|
|
|
|
| Date of Web Publication | 18-Jan-2013 |
 Abstract Abstract | | |
Aims: To assess whether patients above 50 years of age, particularly female, would benefit from repair of their SLAP tears.
Settings and Design: Review of patients' records followed by telephone interview at a minimum of two years after surgery.
Materials and Methods: Seventy-two consecutive patients who had their SLAP repaired were retrospective reviewed by an independent examiner. Follow up was by telephone interview with pain and functional results measured according to the Oxford Shoulder Questionnaire. The patients were asked whether they would undergo the same operation if they had a similar injury.
Statistical Analysis Used: OKS - One way ANOVA, followed by Tukey HSD multiple comparisons were used to assess the Oxford Shoulder score. Kruskal-Wallis Test was used to assess the final VAS Pain Score. Student's T tests for Oxford scores before and after surgery.
Results: Between 2007-2008, 38 male patients and 34 female patients with an average age of 53 (19-75) years had their SLAP repair. Good to excellent results in Oxford shoulder scores were reported in 94%. 68 0f 72 patients would undergo the same if they had a similar injury. No statistical correlation was found between the patient's age, gender and outcome scores.
Conclusions: Neither the patients' gender nor their age above 50 affected the outcome after surgery.
Keywords: Arthroscopic repair, gender and age risk factors, type II superior labrum anterior and posterior lesions
How to cite this article:
Mok D, Wang EL. Does age or gender of the patient influence the outcome of type II superior labrum anterior and posterior repair?. Int J Shoulder Surg 2012;6:112-5 |
 Introduction Introduction | |  |
Superior labrum anterior and posterior (SLAP) lesions are often seen in shoulder arthroscopy. Kim reported an incidence of 26% in 554 arthroscopic procedures for painful shoulder; [1] 88% of the SLAP lesions were associated with intra-articular surface rotator cuff tear. The majority (74%) were type I and 21% type II according to Snyder's classification. [2] From cadaveric studies, Pfahler concluded that type I lesions were natural labral degeneration occurring with advancing age and could be left untreated. [3] In type II lesions where the biceps anchor is detached, Snyder recommended repair with suture anchor. [4] Brockmeier and Kim reported similar excellent results in patients under the age of 50. [5],[6] If a SLAP lesion and a rotator cuff tear were both present, Abbot found better clinical results with SLAP debridement and cuff repair. [7] Franceschi found the same with tenotomy and cuff repair rather than repair of the SLAP. [8] For isolated type II SLAP lesions, Boileau reported significantly better results after tenodesis than suture anchor repair. [9] The aim of our study was to assess whether older patients, particularly female, would benefit from repair of their degenerate SLAP tear.
 Materials and Methods Materials and Methods | |  |
Patients who had arthroscopic repair of their SLAP lesions with a minimum of a two-year follow-up were reviewed retrospectively. To qualify for a diagnosis of SLAP lesions at arthroscopy, they were to have all the following three symptoms: (1) Instability of the anchoring point of the biceps upon probing with displacement from the glenoid margin, (2) fraying of the free labral edge, and (3) exposure of bare bone without articular cartilage at the glenoid neck [Figure 1]. They were excluded if they had a history of dislocation, were aged over 75, or if the bicep tendon itself had an intrasubstance tear of more than 25%. Coexisting pathology, if present, was treated at the same time. In 2007-2008, 72 consecutive patients who underwent SLAP repair by the senior author satisfied the above criteria. The SLAP lesion was repaired with a 3.5 mm lacto (biodegradable) screw (Biomet) with one suture, introduced at the 12 o'clock position through the rotator interval, followed by a simple sliding knot tied posterior to the biceps tendon. The records of the patient were reviewed by an independent examiner for the following characteristics: Age, sex, arm dominance, sporting activity, a history of trauma, and the interval from injury to surgery. Their arthroscopic findings such as extent of SLAP lesion and concomitant pathology were also collected. Follow-up was conducted through a telephone interview with pain and functional results measured according to the Oxford Shoulder Questionnaire. The patients were asked when they returned to work, to play, and whether they would undergo the same operation if they had a similar injury.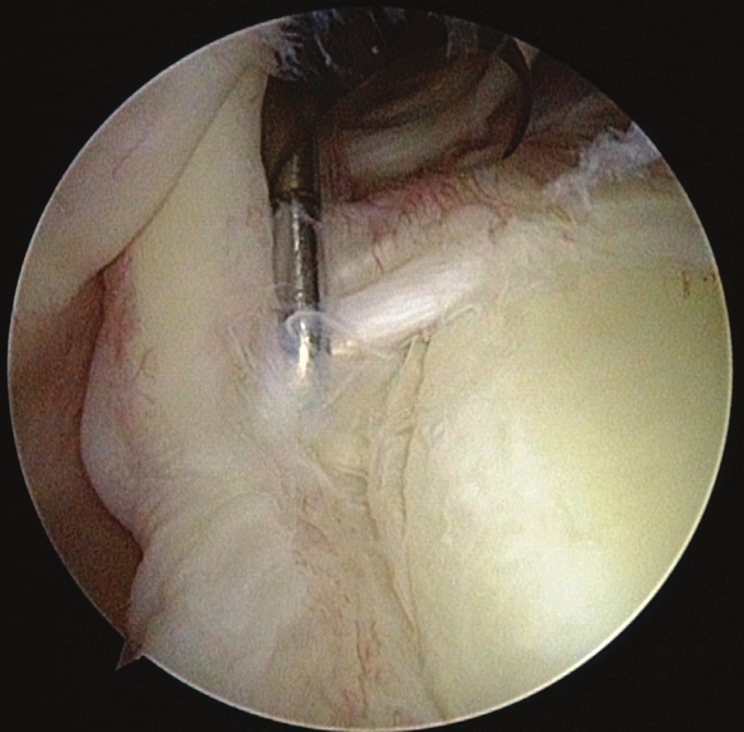 | Figure 1: Superior labrum anterior and posterior lesion with unstable biceps anchor point which could be pulled away from the glenoid margin; note fraying of the labrum
Click here to view |
For statistical analysis, one-way analysis of variance (ANOVA) of the Oxford Shoulder Score (OSS), followed by Tukey honestly significant difference (HSD) multiple comparisons were used to assess the Oxford Shoulder Score. Kruskal-Wallis test was used to assess the final visual analog scale (VAS) pain score. Paired student t-test was used for analysis of pre and postoperative Oxford score.
 Results Results | |  |
There were 38 male patients and 34 female patients with an average age of 53 (range 19-75) years. Twenty-eight patients were aged 60 or over. They had an average follow-up of 26 (24-36) months. The dominant shoulder was involved in 31 patients. Twenty-eight patients participated regularly in sport; 13 played overhead sports and four enjoyed gym workout. The rest were into golf, rugby, and mountain biking. Twenty-one had a recent history of injury to their shoulder on presentation. Thirteen had a history of a fall; four attributed it to lifting heavy weight; in the others, the pain was of gradual onset. Of the clinical signs, 16 patients had a positive O'Brien's test compared with 56 patients who had a positive biceps load test.
At arthroscopy, 45 patients had isolated SLAP tears and 27 had coexisting rotator cuff tears. Nine patients had arthroscopic evidence of degenerative changes affecting the humeral head with two affecting the glenoid surface as well. Buford complexes were noted in three. Subacromial decompression was performed in all except three patients, aged 19, 32, and 72. Seventeen patients required more than one anchor repair to their labral injuries.
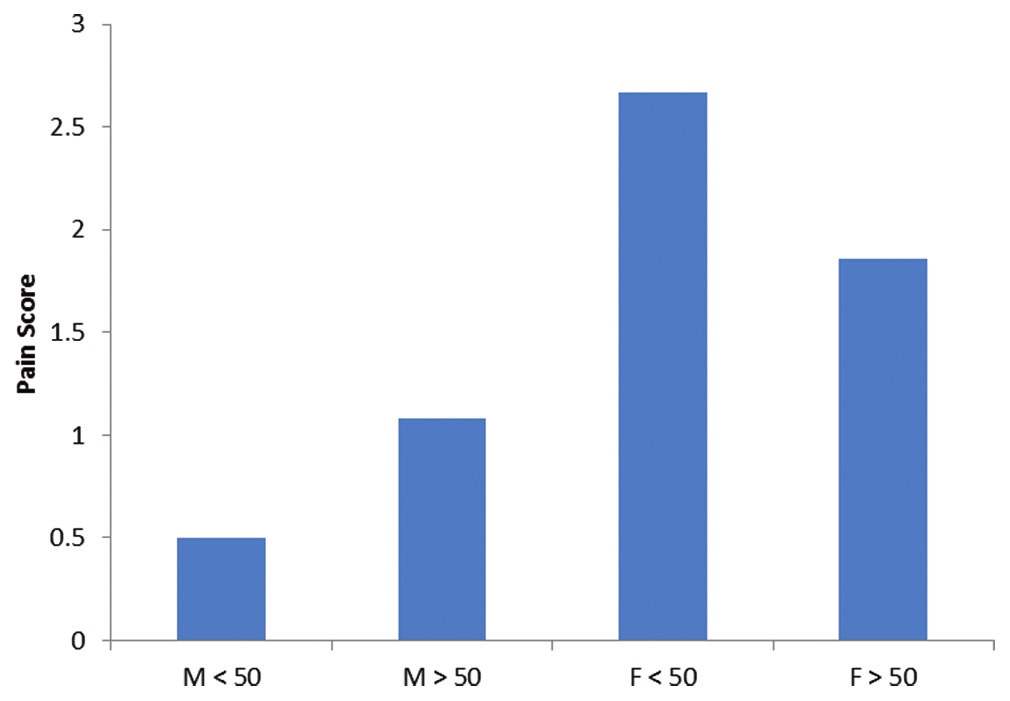
The average Oxford score before surgery was 28 compared with 14.2 after surgery. Results were significantly better after surgery ( P < 0.001). In the final outcome according to the Oxford score, 58 (81%) patients were excellent, 10 (13%) were good, two (3%) were fair, and two (3%) were poor. Statistical analysis revealed there was no significant association between age and gender of the patient and the Oxford Shoulder Score [Figure 2]. None of the four patients with fair and poor Oxford scores had degenerative arthritis in the glenohumeral joint, poor-quality labrum, or coexisting rotator cuff tear. They were all female. Of the 11 patients who had a final pain score of 5 and above, nine were female. There was, however, no association between female patients and the final VAS pain scores [Figure 3]. Patient satisfaction was 95%, with 68 of the 72 respondents reporting that they would have gone through with the operation again. Also, 97% of the patients returned to work and 85% returned to sports. Three of 13 patients who played overhead sports did not return to their sport. There were no patient characteristics that were significant predictors of the fair and poor scores.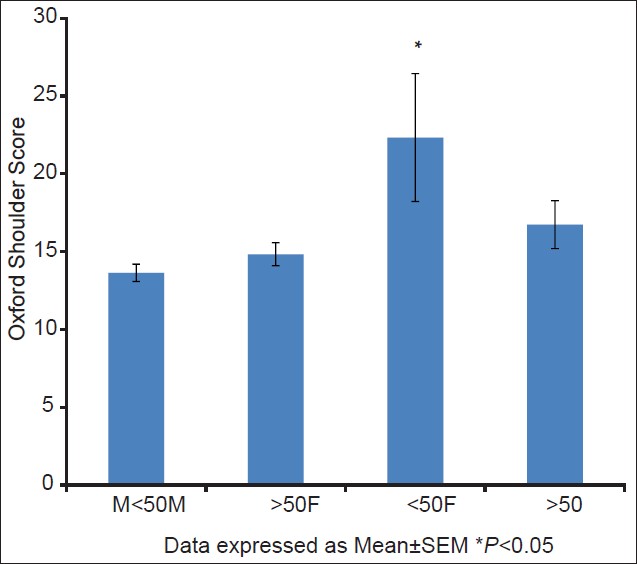 | Figure 2: Statistical analysis of age and gender versus oxford shoulder score
Click here to view |
 | Figure 3: Statistical analysis of age and gender versus final pain score
Click here to view |
 Discussion Discussion | |  |
Arthroscopic definition of a type II SLAP lesion is not absolute. [10] There are 14% anatomical variations which exist at the anchoring point of the biceps. [11] The presence of sublabral recess (2.64%), sublabral foramen (7.67%), and Buford complex (2.64%) could have contributed to the development of type II SLAP. [12] Repair of abnormalities around these anatomical variants may not improve symptoms of the patient. It may even cause pain and limitation of movement. Snyder set a very useful arthroscopic indication for SLAP repair. [13] In our practice, surgical repair is offered to patients with loose bicep anchor point on probing with displacement away from the glenoid margin. Bare bone has to be exposed in the superior glenoid neck where the biceps tendon was formerly attached [Figure 3]. Biceps tendon must not be torn by more than 25%; otherwise, a tenotomy or a tenodesis would be required. We used a single anchor with a simple suture sliding knot tied posterior to the tendon. Additional anchors were used if the tear was extensive. Simple suture anchor repair was found biomechanically to be as effective as single anchor with mattress repair, or two anchors with simple suture tied anterior and posterior to the biceps tendon. [14],[15] In a review of the failure of SLAP repair by Weber, biodegradable and metallic anchors raised concerns of articular cartilage erosion, and he recommended caution with their use. [16] Poly-L/D-lactic acid (PLDLA) biodegradable anchors have recently been reported to be associated with failure of repair. In a 10-year study of 438 patients treated for their SLAP lesions, Park found revision repair in 4.3%. Revision was performed in 24% of poly-96L/4D-lactic acid (ConMed Linvatec) and 4% of poly-70L/30D-lactic acid (Arthrex) anchors. [17] We used a 3.5 mm LactoSorb anchor which is a copolymer of 82% L-lactic acid and 18% glycolic acid (Biomet). In our study, we did not have to revise any of our SLAP repair secondary to failure of anchor fixation.
We found biceps load test more sensitive than O'Brien's test in detecting SLAP lesions. This may be because 60 of our 72 patients were aged over 40. Kim showed that the majority of SLAP lesions coexisted with other intra-articular pathology. [1] Patients younger than 40 were often found to have Bankart lesions and those over 40 had rotator cuff tears or degenerative changes in the joint; the O'Brien's test which was designed to detect isolated SLAP lesions in young athletes was less sensitive as pain from the rotator cuff tear was likely to dominate. We believe biceps load test is likely to be more useful than O'Brien's test for the detection of SLAPs for patients over the age of 40.
Repair of SLAPs lesions were often not offered to patients over 50 years of age. They are deemed to be a natural degenerative phenomenon and should be left untreated. [3] Nevertheless, lifestyle change means men over 50 will spend time in the gym working out with weights. Likewise, ladies may have yoga and Pilates lessons which involve repetitive movements of their arms above the shoulder level. There has often been controversy as to the best treatment for painful SLAP lesions presenting in this age group. Several authors have reported good results in patients over 40 after their SLAP repair. [18],[19] Others found better results after tenotomy with or without tenodesis than SLAP lesions after suture anchor repair. [8],[9] Problem with biceps tenotomy is that it results in a muscle belly bulge in the lower arm, the Popeye sign, in 70% of the shoulders. [20] This cosmetic deformity may not be acceptable for those who work out to keep their bodies in shape. Boileau did not find this deformity an issue with his patients. [9],[21] Another complaint after tenotomy was discomfort of muscle fatigue in the lower arm after resisted elbow flexion. Kelly reported this in 38% of 54 patients. [19] Tenodesis reduced the risk of the Popeye sign and could restore elbow strength to 90% of the contralateral side. [22] In laboratory tests, 40% of the tenotomized specimens failed under physiological loading compared with none in the tenodesed specimens. [23] After tenodesis, Boileau reported that 13 of 15 patients were able to return to their previous level of participation in sports. This compared with only 2 of 10 patients after SLAP repair ( P = 0.01). [9] In a recent literature review of 517 patients with painful biceps tendons treated with either tenodesis or tenotomy, Hsu could not recommend any one procedure over the next. He found that after tenodesis, 25% of the patients still developed a Popeye sign. [24]
In a Canadian study of 279 patients with rotator cuff-related problems treated arthroscopically, female patients had significantly more emotional difficulties. [25] Female patients had significantly lower outcome scores after treatment, compared with male patients, particularly those under the age of 55. In our study, patients who did not have good or excellent results were female, under the age of 55. However, statistical analysis of the Oxford Shoulder Score and the VAS pain score independently did not show significant difference between male or female patients above or below the age of 50. We therefore could not support the hypothesis that female patients could have a worse outcome after their SLAP repair.
A limitation to our study was the small sample size used for assessing gender and age as risk factors for the outcome after surgery. Though one surgeon did the operation with a standardized technique, concomitant pathology may have been the source of pain rather than SLAP lesions. We excluded patients with a history of dislocation on the assumption that these patients often had an additional Bankart lesion and would require repair. This exclusion left us 60 patients who were aged 40 and above. In this age group, SLAP lesions and rotator cuff tears were commonly found together. [1] Repair of the SLAP lesion may not be the only beneficial treatment for the patient. We used Oxford Shoulder Score as subjective outcome measure as our interviews with patients were conducted by telephone. This scoring system is an accepted assessment tool after shoulder surgery. [26] Despite the above limitations, the study showed the benefit of SLAP repair irrespective of the age or gender of the patient.
 Conclusion Conclusion | |  |
After repair of their type II SLAP lesions, 94% of patients had a good to excellent result. Satisfaction of patients was 95%. Neither age nor gender had influenced the outcome. We recommend repair of symptomatic SLAP tears when present at arthroscopy.
The assistance of Ms Maggie Shen in providing the statistical analysis is appreciated.
 References References | |  |
| 1. | Kim TK, Queale WS, Cosgarea AJ, McFarland EG. Clinical features of the different types of SLAP lesions: An analysis of one hundred and thirty-nine cases. J Bone Joint Surg Am 2003;85-A: 66-71. 
[PUBMED] |
| 2. | Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Am J Sports Med 1990;6:274-9. 
[PUBMED] |
| 3. | Pfahler M, Haraida S, Schulz C, Anetzberger H, Refior HJ, Bauer GS, et al. Age-related changes of the glenoid labrum in normal shoulders. J Shoulder Elbow Surg 2003;12:40-52. 
[PUBMED] |
| 4. | Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg 1995;4:243-8. 
[PUBMED] |
| 5. | Brockmeier SF, Voos JE, Williams RJ, Altchek DW, Cordasco FA, Allen AA. Outcomes After Arthroscopic Repair of Type-II SLAP Lesions. J Bone Joint Surg Am 2009;91:1595-603. 
|
| 6. | Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am 2002;84:981-5. 
[PUBMED] |
| 7. | Abbot AE, Li X, Busconi BD. Arthroscopic treatment of concomitant superior labral anterior posterior (SLAP) lesions and rotator cuff tears in patients over the age of 45 years. Am J Sports Med 2009;37:1358-62. 
[PUBMED] |
| 8. | Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. No advantages in repairing a type II superior labrum anterior and posterior (SLAP) lesion when associated with rotator cuff repair in patients over age 50: A randomized controlled trial. Am J Sports Med 2008;36:247-53. 
[PUBMED] |
| 9. | Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: Biceps tenodesis as an alternative to reinsertion. Am J Sports Med 2009;37:929-36. 
[PUBMED] |
| 10. | Nam EK, Snyder SJ. The diagnosis and treatment of superior labrum anterior and posterior (SLAP) lesions. Am J Sports Med 2003;31:798-810. 
[PUBMED] |
| 11. | Kanatli U, Ozturk B, Bolukbasi S. Anatomical variations of the anterosuperior labrum: Prevalence and association with type II superior labrum anterior-posterior (SLAP) lesions. J Shoulder Elbow Surg 2010;19:1199-203. 
|
| 12. | Bents RT, Skeete KD. The correlation of the Buford complex and SLAP lesions. J Shoulder Elbow Surg 2005;14:565-9. 
[PUBMED] |
| 13. | Burns JP, Bahk M, Snyder SJ. Superior labral tears: Repair versus biceps tenodesis. J Shoulder Elbow Surg 2011;20:52-8. 
[PUBMED] |
| 14. | Yoo JC, Ahn JH, Lee SH, Lim HC, Choi KW, Bae TS, et al. A biomechanical comparison of repair techniques in posterior type II superior labral anterior and posterior (SLAP) lesions. J Shoulder Elbow Surg 2008;17:144-9. 
[PUBMED] |
| 15. | Baldini T, Snyder RL, Peacher G, Bach J, McCarty E. Strength of single- versus double-anchor repair of type II SLAP lesions: A cadaveric study. Arthroscopy 2009;25:1257-60. 
[PUBMED] |
| 16. | Weber SC. Surgical management of the failed SLAP repair. Sports Med Arthrosc 2010;18:162-6. 
[PUBMED] |
| 17. | Park MJ, Hsu JE, Harper C, Sennett BJ, Huffman GR. Poly-L/D-Lactic acid anchors are associated with reoperation and failure of SLAP repairs. Arthroscopy 2011;27:1335-40. 
[PUBMED] |
| 18. | Kanatli U, Ozturk BY, Bolukbasi S. Arthroscopic repair of type II superior labrum anterior posterior (SLAP) lesions in patients over the age of 45 years: A prospective study. Arch Orthop Trauma Surg 2011;131:1107-13. 
[PUBMED] |
| 19. | Alpert JM, Wuez TH, O'Donnell TF, Caroll KM, Bruckner NN, Gill TJ. The effect of age on the outcomes of arthroscopic repair of typeII superior labral anterior and posterior lesions. Am J Sports Med 2010;38:2299-303. 
|
| 20. | Kelly AM, Drakos MC, Fealy S, Taylor SA, O'Brien SJ. Arthroscopic release of the long head of the biceps tendon. Am J Sports Med 2005;33:208-13. 
[PUBMED] |
| 21. | Boileau P, Baque F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am 2007;89:747-57. 
|
| 22. | Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: A new technique using bioabsorbable interference screw fixation. Arthroscopy 2002;18:1002-12. 
[PUBMED] |
| 23. | Wolf RS, Zheng N, Weichel D. Long head biceps tenotomy versus tenodesis: A cadaveric biomechanical analysis. Arthroscopy 2005;21:182-5. 
[PUBMED] |
| 24. | Hsu AR, Ghodadra NS, Provencher MT, Lewis PB, Bernard BR. Biceps tenotomy versus tenodesis: A review of clinical outcomes and in biomechanical results. J Shoulder Elbow Surg 2011;20:326-32. 
|
| 25. | Razmjou H, Holtby R, Myhr T. Gender differences in quality of life and extent of rotator cuff pathology. Arthroscopy 2006;22:57-62. 
[PUBMED] |
| 26. | Desai AS, Dramis A, Hearnden AJ. Critical appraisal of subjective outcome measures used in the assessment of shoulder disability. Ann R Coll Surg Engl 2010;92:9-13. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3]
|
