| |


 |
| Year : 2013 | Volume
: 7
| Issue : 1 | Page : 32-36 |
|
|
|
|
|
SURGICAL TECHNIQUE Arthroscopic autograft reconstruction of the inferior glenohumeral ligament: Exploration of technical feasibility in cadaveric shoulder specimens
Samy Bouaicha1, Beat K Moor2
1 Division of Trauma Surgery, University Hospital of Zurich, Zurich, Switzerland
2 Department of Orthopaedics, Balgrist University Hospital, Zurich, Switzerland
Correspondence Address:
Samy Bouaicha
Division of Trauma Surgery, University Hospital of Zurich, Raemistrasse 100, 8091 Zurich
Switzerland
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.109893

|
|
|
|
| Date of Web Publication | 2-Apr-2013 |
 Abstract Abstract | | |
Failure of primary arthroscopic Bankart repair in anterior-inferior glenohumeral instability is low, but in some cases revision surgery is required. Revision procedures show good to excellent results but typically are done open and do not respect the anatomical functionality of the joint capsule. The purpose of this cadaveric study was to explore the feasibility of a completely arthroscopic anatomical reconstruction of the inferior glenohumeral ligament using a hamstring autograft.
Keywords: Arthroscopy, autograft reconstruction, cadaver study, inferior glenohumeral ligament
How to cite this article:
Bouaicha S, Moor BK. Arthroscopic autograft reconstruction of the inferior glenohumeral ligament: Exploration of technical feasibility in cadaveric shoulder specimens. Int J Shoulder Surg 2013;7:32-6 |
 Introduction Introduction | |  |
The inferior glenohumeral ligament (IGHL) complex is the major passive restraint to anterior-inferior dislocation in the abduction and external rotation (ABER) position of the shoulder joint. [1],[2],[3] The traumatic detachment of its anterior band (AB) from the glenoid rim - the Bankart lesion - may cause persistent antero-inferior shoulder instability. [4],[5] In the past decade, arthroscopic repair of the Bankart lesion has become very popular and represents the current state-of-the-art in the treatment of traumatic, unidirectional anterior-inferior shoulder instability. [6],[7],[8],[9] Failure of arthroscopic Bankart repair was reported to be 4-18%. [9],[10],[11],[12] For revision surgery after open or arthroscopic Bankart repair, extra-anatomical bone block procedures such as the Bristow-Latarjet or iliac crest bone graft reconstruction have shown to be successful. [13],[14],[15],[16] Recently, several authors reported good and excellent results with arthroscopic revision Bankart repairs as well. [17],[18],[19] For chronic anterior capsular deficiency, open procedures with autologous iliotibial band or hamstring graft reconstruction have been reported. [20],[21] No data exists for completely arthroscopic autograft reconstruction of the IGHL complex.
The aim of our study was to explore the technical feasibility of an all-arthroscopic, anatomical reconstruction of the anterior and posterior bands (PBs) of the IGHL using a hamstring autograft in two cadaveric shoulder specimens.
 Surgical Procedure Surgical Procedure | |  |
The concept behind anatomical IGHL reconstruction is to recreate a triangular sling with the tendon autograft that prevents anterior-inferior subluxation and dislocation of the humeral head. The sling has two footprints, one located at the anterior glenoid rim attached by two suture anchors between 4 and 3 o'clock on the right shoulder (8 and 9 for left shoulders) at the origin of the AB of the IGHL and the other one attached posteriorly between 8 (4) and 7 (5) o'clock representing the origin of the PB. The sling apex is fixed as a doubled tendon graft within the humeral head and blocked with an interference screw [Figure 1]a. The triangular construct between the glenoid and the humeral head is slack in neutral position of the glenohumeral joint and becomes progressively more tensioned with increasing ABER, forming a triangular restraint in front of the humeral head [Figure 1]b. The two limbs of the reconstructed IGHL hereby adapt to the preexisting inferior capsular pouch, creating reinforcement of the incompetent IGHL complex, similar to the genuine AB and PB.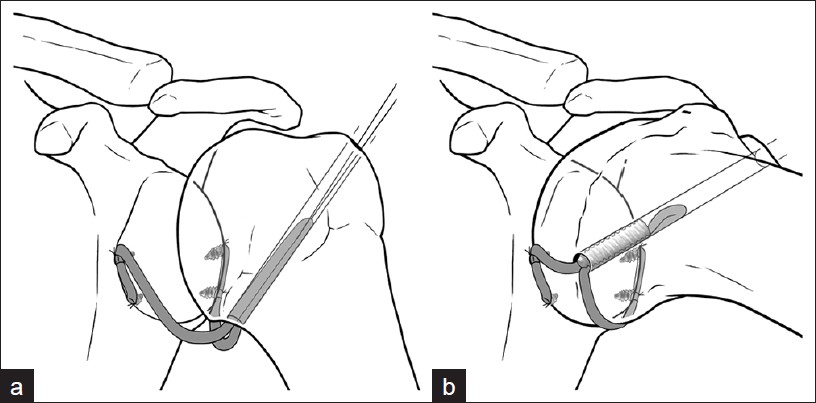 | Figure 1: Schematic illustration of the anatomical reconstruction of the IGHL with a hamstring autograft. (a) (left) Shows the slack graft in the neutral position while (b) (right) shows the tensioned graft in the abduction external rotation (ABER) position forming a triangular restraint in front of the humeral head
Click here to view |
To simulate shoulder arthroscopy, the cadavers were placed in a beach chair-like position. First, harvesting of the ipsilateral hamstring tendons was performed using a standard 7 mm stripper for anterior cruciate ligament (ACL) reconstruction (Karl Storz GmbH and Co KG, Tuttlingen, Germany). In this study, the gracilis tendon was used instead of the semitendinosus, in order to avoid bulky graft in the shoulder joint.
Graft lengths vary but should be a minimum of 20 cm. For diagnostic shoulder arthroscopy, the camera was brought in through the standard posterior portal. Before starting the reconstruction, an anterolateral working portal was established and the antero-inferior capsule-labral complex was detached using an arthroscopic chisel (Karl Storz GmbH and Co KG).
The first step of the reconstruction was placement of four suture anchors (BioPlug® Karl Storz GmbH and Co KG) at the anterior and posterior glenoid rim. Two anchors were inserted at the anatomical origins of the anterior and posterior bands at 3 (9) o'clock and 8 (4) o'clock, respectively. Two other anchors were inserted about 5-10 mm inferior at the anterior glenoid and 5-10 mm superior at the posterior glenoid, allowing "side-to-side" attachment of the tendon ends for better graft-bone healing [Figure 2].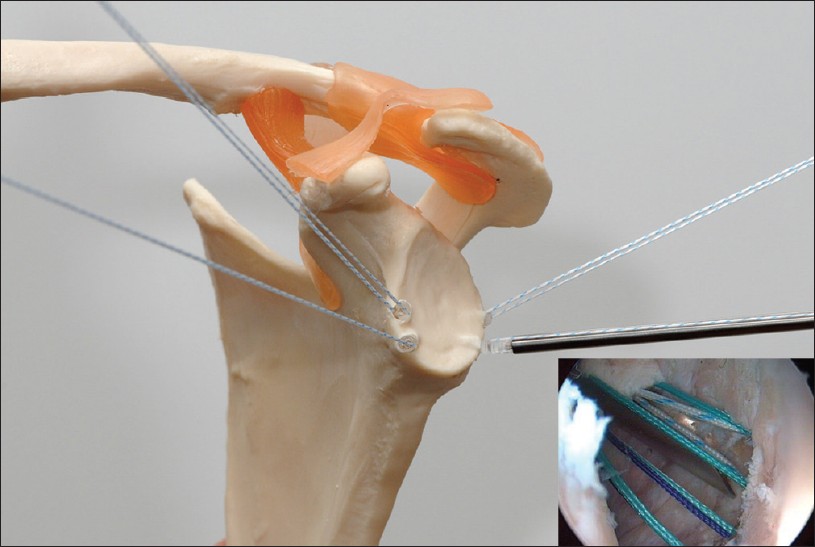 | Figure 2: Position of the four suture anchors. The anterior inferior anchor represents the anatomical origin of the anterior band of the IGHL while the posterior superior anchor marks the origin of the posterior band. The other two anchors should allow a better (side-toside) engraftment of the tendon. The inlet shows the arthroscopic view of the anterior anchors
Click here to view |
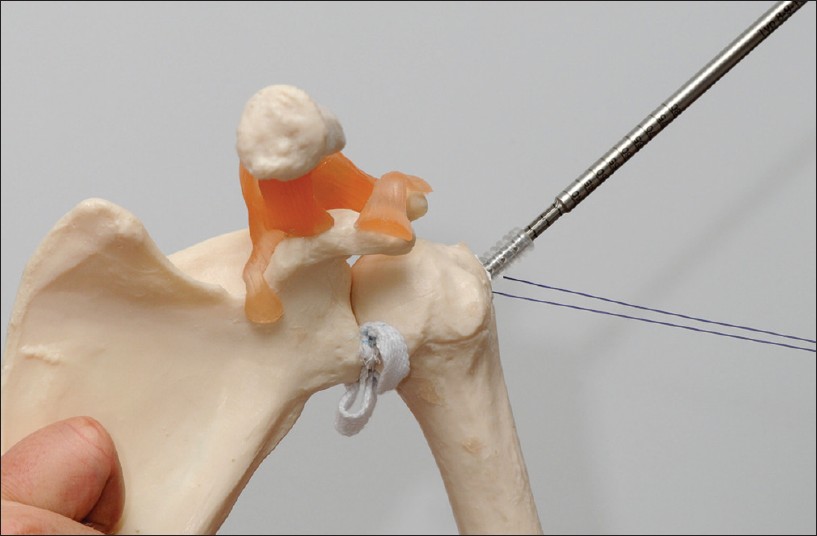
The next step was percutaneous drilling of a 6-8 mm hole (depending on doubled graft diameter) through the greater tuberosity aiming at the center of the anatomical neck just above the inferior capsule using a tibial posterior cruciate ligament (PCL) targeting device (Karl Storz GmbH and Co KG). For that purpose, the targeting device was inserted through the posterior portal and the bullet for the drill bit was placed approximately 1 cm lateral to the palpable lateral edge of the acromion [Figure 3] and [Figure 4].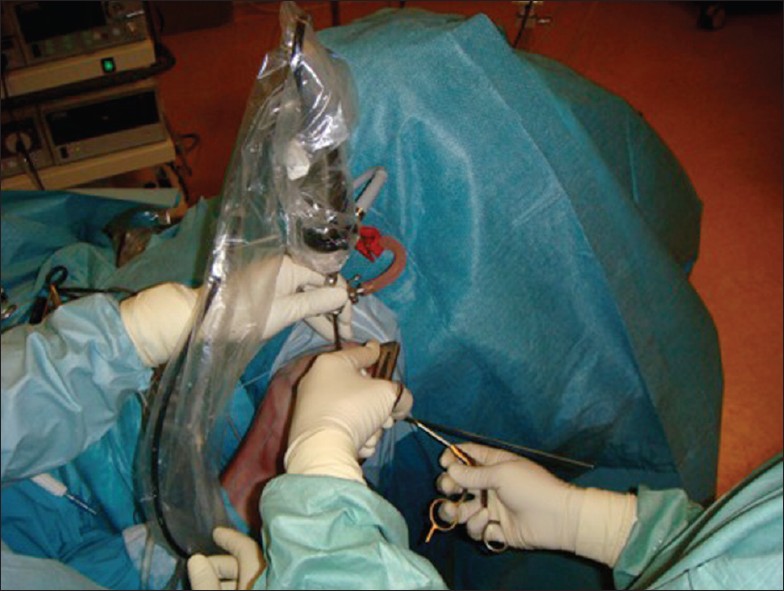 | Figure 3: Positioning of the targeting device: Insertion through the posterior portal, viewing portal is the anterosuperior portal
Click here to view |
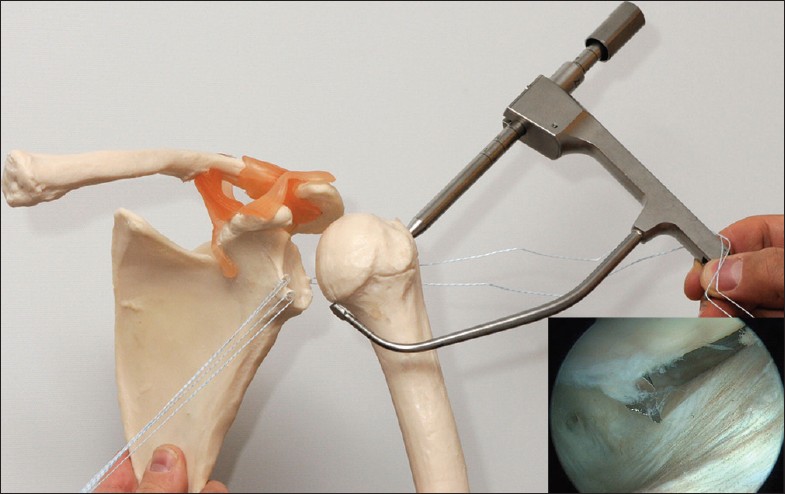 | Figure 4: Transhumeral outside-in drilling with a targeting device. The intraarticular drill hole is placed just above the humeral insertion of the inferior joint capsule in the center of the humeral head. For better illustration, the device is brought in front of the humerus. Inlet: Arthoscopic view of the wire tip
Click here to view |
To attach the graft to its anterior glenoid footprint, one tendon end was prepared with a baseball-type stitch from one limb of the anterior-inferior 4 (8) o'clock suture anchor. Then the graft was pulled into the joint and the first (non-gliding) knot was tied [Figure 5]. Enlarging the anterior footprint (assuming better healing potential to the bone), the graft tail was brought upward along the anterior rim and fixed "side-to-side" with the 3 (9) o'clock anchor (gliding knot).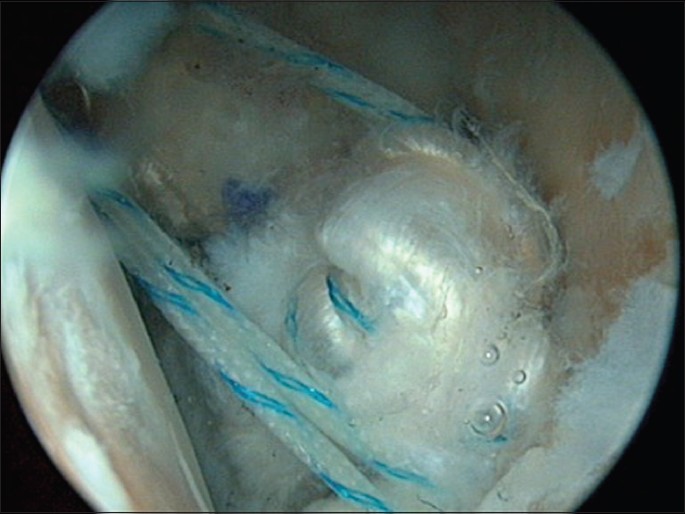 | Figure 5: Arthroscopic view of the anterior graft limb pulled into the joint using one suture limb of the antero-inferior anchor
Click here to view |
Posterior graft fixation was performed similarly after changing the camera to the anterolateral portal. This time "end-to-side" fixation was performed superiorly at the 8 (4) o'clock anchor and "side-to-side" fixation inferiorly at the 7 (5) o'clock anchor. Because of limited viewing with the entire tendon graft in the joint, careful suture management is critical before pulling the posterior graft tail into the joint. Therefore, two additional suture portals were established, one anterolateral and another posterolateral in the same fashion as commonly used in rotator cuff reconstructions. [Figure 6] shows the anteriorly and posteriorly fixed autograft in a shoulder model. As an alternative to advancing the graft through the anterior portal, insertion through the humeral drilling hole could be an option. This, however, was not tested in the present study.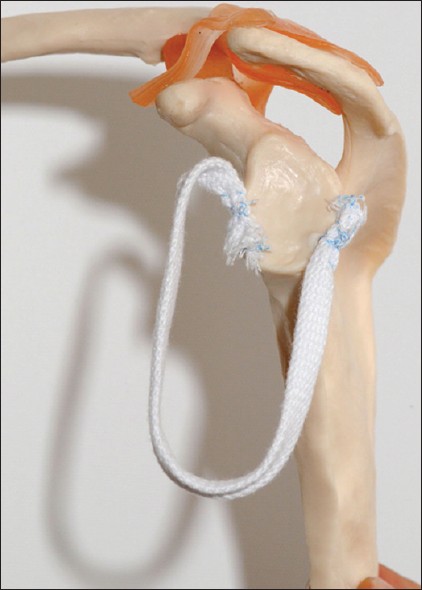 | Figure 6: Overview of the glenoidal attachments of the anterior and posterior tendon limbs
Click here to view |
Finally, the apex of the graft sling was pulled inside-out into the humeral head using an already out-of-joint PDS shuttle suture [Figure 7]. Fixation of the now double-stranded sling apex was achieved with a 7 × 3 mm interference screw (MegaFix® Karl Storz GmbH and Co KG) [Figure 8]. It was essential to fix the sling apex within the humeral head in the ABER position allowing full range of motion of the glenohumeral joint [Figure 9]. Fixation of the graft in any position other than ABER will subsequently lead to significant limitation in range of motion. Following this principle, normal shoulder range of motion was obtained in both cases. [Figure 10] shows the slack graft in the axillary pouch (AP) during neutral rotation. Anterior arthrotomy after completion of the procedure confirmed correct position of the humeral graft attachment [Figure 11].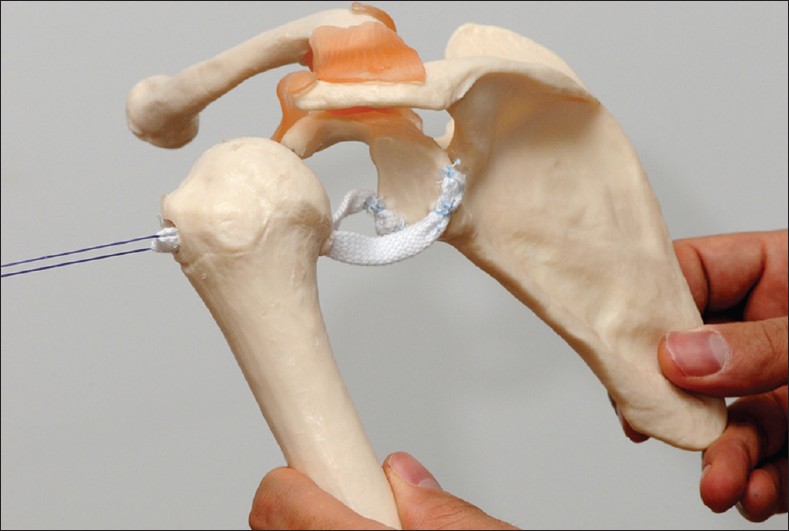 | Figure 7: Pull out of the graft sling: the apex of the graft is pulled inside-out into the humeral head using a graft embracing PDS shuttle
Click here to view |
 | Figure 8: Fixation of the sling apex with the head using a outside-in interference screw 7 × 3 mm MegaFix® Karl Storz GmbH and Co KG, Tuttlingen, Germany)
Click here to view |
 | Figure 9: To obtain full of range motion, it is mandatory to fix the interference screw in the abduction external rotation position
Click here to view |
 | Figure 10: Arthroscopic view of the slack graft within the joint. There is no tension on the graft since the shoulder is in neutral position
Click here to view |
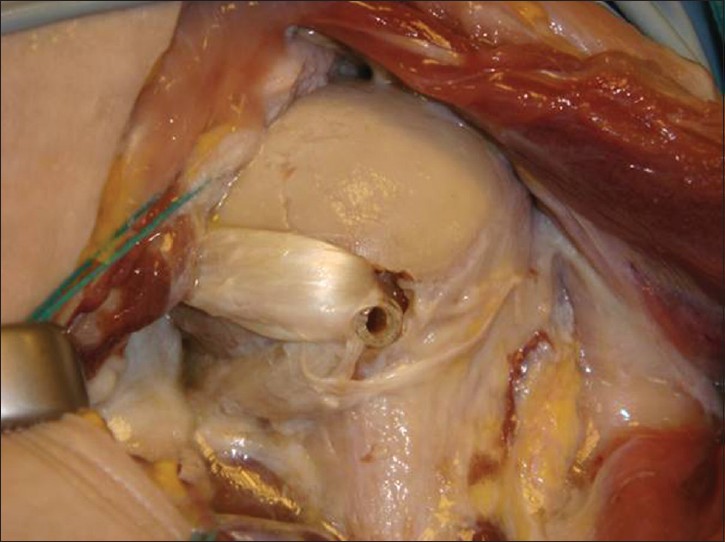 | Figure 11: Post-procedure arthrotomy of a shoulder specimen: Central intraarticular position of the humeral graft attachment. Notice the reconstructed triangular IGHL complex spanning over the anteroinferior aspect of the humeral head
Click here to view |
 Discussion Discussion | |  |
The complex architecture of the IGHL with its three parts, AB, AP, and PB, provides selective resistance to anterior-inferior movement of the humeral head during ABER. With progression into the late cocking throwing position, the IGHL complex shifts from inferiorly upward like a double reinforced sheet in front of the anterior aspect of the humeral head. With chronic insufficiency, especially of the anterior band, the humeral head can easily glide over the anterior-inferior glenoid rim causing recurrent instability. Arthroscopic or open Bankart repair indeed re-attaches the capsulo-labral structures to the glenoid, but does not restore the anatomical and functional properties of the IGHL complex in cases of chronic insufficiency. Open procedures to reconstruct or reinforce the anterior joint capsule were described, but they are not anatomical and extensive surgical exploration is mandatory. [20],[21] Long-term results for these salvage procedures are not available. Extra-anatomical bone block procedures provide good to excellent results. [13],[14],[15],[16] Usually they are the "last line of defense" in treatment of chronic instability, and revision surgery after failure is difficult.
With the above-described and illustrated surgical technique, we successfully demonstrated the technical feasibility of a completely arthroscopic and anatomical reconstruction of the anterior and posterior band of the IGHL. The two graft limbs were shown to restore the original IGHL function, moving in front of the humeral head in the ABER position and limiting pathological anterior-inferior humeral translation. The graft did not limit or disturb normal glenohumeral range of motion. Additional anterior capsulorraphy with double-armed suture anchors may be considered to reduce the volume of the anterior capsule and to create a soft-tissue envelope for better healing of the anterior graft tail. Using newer knotless anchoring systems may also theoretically reduce complexity of the procedure.
The critical points of the procedure were careful and simple suture management (additional suture portals) once the graft was inserted into the shoulder joint, and the fixation of the interference screw in the ABER position. Preliminary storage of the graft in the AP allowed for sufficient visualization of anterior and posterior graft attachment to the glenoid.
We believe this procedure is suitable for revision surgery after failed arthroscopic Bankart repair, especially in the absence of major glenoidal bone loss, or as an alternative to open and extra-anatomical bone block procedures. Since arthroscopic Bankart repair is a common and successful primary surgical intervention in the treatment of acute anterior-inferior shoulder instability with low failure rate, [9],[10],[11],[12] we do not think that anatomical IGHL reconstruction should be considered for index repair.
However, further biomechanical and clinical investigations are mandatory to prove the mechanical properties and clinical impact of this technique.
 Acknowledgment Acknowledgment | |  |
We thank Mr. Mike Müller for his close technical support with arthroscopic implants, cadaver specimens, and his excellent imaging performance.
 References References | |  |
| 1. | Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am 1981;63:1208-17. 
|
| 2. | O'Connell PW, Nuber GW, Mileski RA, Lautenschlager E. The contribution of the glenohumeral ligaments to anterior stability of the shoulder joint. Am J Sports Med 1990;18:579-84. 
|
| 3. | Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res 2002;400:32-9 
|
| 4. | Sachs RA, Lin D, Stone ML, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg Am 2007;89:1665-74. 
|
| 5. | Hovelius L, Olofsson A, Sandstrom B, Augustini BG, Krantz L, Fredin H, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am 2008;90:945-52. 
|
| 6. | Hobby J, Griffin D, Dunbar M, Boileau P. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. J Bone Joint Surg Br 2007;89:1188-96. 
|
| 7. | Kropf EJ, Tjoumakaris FP, Sekiya JK. Arthroscopic shoulder stabilization: Is there ever a need to open? Arthroscopy 2007;23:779-84. 
|
| 8. | Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: Nonoperative and surgical treatment. Arthroscopy 2009;25:298-304. 
|
| 9. | Voos JE, Livermore RW, Feeley BT, Altchek DW, Williams RJ, Warren RF, et al. Prospective evaluation of arthroscopic bankart repairs for anterior instability. Am J Sports Med 2010;38:302-7. 
|
| 10. | Carreira DS, Mazzocca AD, Oryhon J, Brown FM, Hayden JK, Romeo AA. A prospective outcome evaluation of arthroscopic Bankart repairs: Minimum 2-year follow-up. Am J Sports Med 2006;34:771-7. 
|
| 11. | Kim SH, Ha KI, Cho YB, Ryu BD, Oh I. Arthroscopic anterior stabilization of the shoulder: Two to six-year follow-up. J Bone Joint Surg Am 2003;85-A: 1511-8. 
|
| 12. | Mazzocca AD, Brown FM Jr, Carreira DS, Hayden J, Romeo AA. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med 2005;33:52-60. 
|
| 13. | Allain J, Goutallier D, Glorion C. Long-term results of the latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 1998;80:841-52. 
|
| 14. | Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007;23:1033-41. 
|
| 15. | Hovelius L, Sandstrom B, Sundgren K, Saebo M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: Study I--clinical results. J Shoulder Elbow Surg 2004;13:509-16. 
|
| 16. | Warner JJ, Gill TJ, O'Hollerhan JD, Pathare N, Millett PJ. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med 2006;34:205-12. 
|
| 17. | Ryu RK, Ryu JH. Arthroscopic revision Bankart repair: A preliminary evaluation. Orthopedics 2011;34:17. 
|
| 18. | Bartl C, Schumann K, Paul J, Vogt S, Imhoff AB. Arthroscopic capsulolabral revision repair for recurrent anterior shoulder instability. Am J Sports Med 2011;39:511-8. 
|
| 19. | Kim SH, Ha KI, Kim YM. Arthroscopic revision Bankart repair: A prospective outcome study. Arthroscopy 2002;18:469-82. 
|
| 20. | Iannotti JP, Antoniou J, Williams GR, Ramsey ML. Iliotibial band reconstruction for treatment of glenohumeral instability associated with irreparable capsular deficiency. J Shoulder Elbow Surg 2002;11:618-23. 
|
| 21. | Alcid JG, Powell SE, Tibone JE. Revision anterior capsular shoulder stabilization using hamstring tendon autograft and tibialis tendon allograft reinforcement: Minimum two-year follow-up. J Shoulder Elbow Surg 2007;16:268-72. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10], [Figure 11]
|
