| |


 |
| Year : 2013 | Volume
: 7
| Issue : 3 | Page : 105-109 |
|
|
|
|
|
ORIGINAL ARTICLE Relationship between the functional outcomes and radiological results of conservatively treated displaced proximal humerus fractures in the elderly: A prospective study
Mehmet Kerem Canbora1, Ozkan Kose2, Atilla Polat1, Levent Konukoglu1, Mucahit Gorgec1
1 Department of Orthopaedics and Traumatology, Haydarpasa Numune Education and Research Hospital, Istanbul, Turkey
2 Department of Orthopaedics and Traumatology, Antalya Education and Research Hospital, Antalya, Turkey
Correspondence Address:
Mehmet Kerem Canbora
Barbaros mah. B 6 Blok, Daire 3, Uphill Court Sitesi, Atasehir, Postal Code 34746, Istanbul
Turkey
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/0973-6042.118911

|
|
|
|
| Date of Web Publication | 25-Sep-2013 |
 Abstract Abstract | | |
Purpose: The purpose of this prospective study is to investigate the relationship between the functional outcome and the radiographic results of conservatively treated two-, three- and four-part proximal humeral fractures in patients aged over 65 years.
Materials and Methods: The study comprised 29 prospectively followed cases aged over 65 years who presented with displaced proximal humerus fracture between 2009 and 2011. The fractures were classified according to the Neer classification and all met the displacement criteria described by Neer. Standard physical therapy program was applied. Patients were evaluated clinically using Constant shoulder score, quick form of disabilities of arm, shoulder and hand score and visual analog scale. At the final follow-up, humeral head position in the coronal plane was assessed with neck-shaft angle. Any complication was recorded during the treatment period. Correlation between the functional outcomes and final radiologic results were statistically analyzed.
Results: Data were analyzed from 29 cases (21 female, 8 male) with a mean age was 78 ± 8.6 years (range 65-93 years). The mean follow-up period was 18.2 ± 4.07 months (range 12-26 months). Functional results were significantly related with initial fragmentation. However, there was no correlation between the functional outcomes and the final geometry of the humeral head. Despite the union occurred with deformity, the functional outcome were satisfactory.
Conclusion: The results of this study show that initial fragmentation has a negative effect on the functional results. However, the changed position of the humeral head on coronal plane does not affect the final functional results.
Keywords: Functional outcomes, non-operative treatment, proximal humerus fractures
How to cite this article:
Canbora MK, Kose O, Polat A, Konukoglu L, Gorgec M. Relationship between the functional outcomes and radiological results of conservatively treated displaced proximal humerus fractures in the elderly: A prospective study. Int J Shoulder Surg 2013;7:105-9 |
How to cite this URL:
Canbora MK, Kose O, Polat A, Konukoglu L, Gorgec M. Relationship between the functional outcomes and radiological results of conservatively treated displaced proximal humerus fractures in the elderly: A prospective study. Int J Shoulder Surg [serial online] 2013 [cited 2016 May 22];7:105-9. Available from: http://www.internationalshoulderjournal.org/text.asp?2013/7/3/105/118911 |
 Introduction Introduction | |  |
Proximal humeral fractures (PHFs) account for 4-5% of all fractures. These fractures are more prevalent in older patients, many of whom have osteoporosis. [1] Most PHF are minimally displaced and can be treated conservatively. [2] On the other hand, almost 15-20% of PHF are displaced and require surgical intervention. [1] Neer defined significant displacement as more than 1cm of translation or more than 45° of angulation in any major fracture fragment. [3]
It is difficult for orthopedic surgeons to render the ideal treatment for displaced PHFs in elderly patients. The leading recommended treatment options include open reduction and internal fixation, hemiarthroplasty and conservative approach for these fractures; however, there is no straightforward indication. [4],[5] Surgical treatment of displaced PHFs in elderly is not always an excellent choice and often results in failure due to severe osteoporosis and patient related co-morbidities. [5],[6] Recently, reports of satisfactory results have encouraged orthopedic surgeons to prefer conservative treatment for displaced PHFs in elderly. [7],[8],[9]
Most authors have suggested that functional outcomes associated with the initial displacement and the number of fracture fragments. However, it is not clear that poor functional outcomes are related to the final geometry of the humeral head after fracture union. [9],[10],[11],[12] We hypothesized that final geometry of the humeral head after the union is related with the functional outcome rather than the initial fracture comminution. This study aimed to investigate the relationship between the severity of the humeral head fragmentation and the final geometry of the humeral head after union from the functional and clinical results of elderly patients treated conservatively for displaced PHFs.
 Materials and Methods Materials and Methods | |  |
This prospective study comprised 34 consecutive cases aged 65 years and over who presented at our clinic between March 2009 and April 2011 with displaced PHF and were treated conservatively. In all the patients, surgery was planned, but could not be performed due to either patient had high risk anesthesia, American Society of Anesthesiology IV (ASA IV) or patient did not elect to undergo surgery despite recommendation. The fractures were classified according to the Neer classification and all met the displacement criteria (45° angulation of fragments and/or more than 1 cm translation). [3] Any cases of open fracture, pathological fracture, polytrauma patients or those with neurological or psychiatric problems, which would prevent them following the rehabilitation protocol, were excluded from the study. This study was carried out according to the Declaration of Helsinki and Institutional Review Board approved the study protocol.
The patient demographic data (age, gender, affected side, dominant side, comorbidities) and fracture type were recorded. Initial radiologic examination was made by anteroposterior and scapular Y radiographs. Computerized tomography (CT) was used if any doubt existed as to the degree of comminution or position of the displaced fracture parts. No reduction was made on any case. The arm was immobilized in a sling for the 1 st week. The physical therapy was started with pendular shoulder exercises in the 2 nd week and gradually increased as the patient tolerated. Passive shoulder exercises were encouraged in the 3 rd week and active and active-assisted shoulder movements were began in the 6 th week. Rotational movements were not allowed until the 6 th week to avoid further translation of the fragments.
Following the rehabilitation program, patients came for clinical follow-up at the 3 rd month, 6 th month, 1 year and then yearly thereafter. Patients were evaluated clinically using Constant shoulder score (CS), quick form of disabilities of arm, shoulder and hand score (Q-DASH) and visual analog scale (VAS) in each visit and the last follow-up. [13],[14] After fracture union, active shoulder movements were evaluated. The capacity for pain-free flexion, abduction, external rotation, internal rotation and other active range of movements were measured by goniometry. The shoulder range of movements was compared with the contralateral side. When measuring the capacity for internal rotation, as patients were not capable of internal rotation while the shoulder was at 90° abduction, the highest vertebral level that could be reached with the hand behind the back was stated as the level of internal rotation. Muscle strength was accepted as the highest level of shoulder flexion achieved while holding a 1 kg weight with the shoulder at 90° abduction. [5] CS results were evaluated as more than 70 points, excellent, 50-70 points, satisfactory and below 50 points, poor. [15]
Union was monitored radiologically and clinically on a weekly basis for the first 2-6 weeks then at the 3 rd , 6 th and yearly thereafter. At the end of 1 year, a shoulder CT was performed. Shoulder CT and radiographs were assessed for union, malunion, humeral head coronal plane position, osteoarthritis and possible osteonecrosis. After union, the humeral head coronal plane position was determined by the angle at the intersection of the line drawn between the tip of the tuberculum majus and the tip of the inferior joint surface and the line drawn parallel to the humeral diaphysis cortices and this was compared with the contralateral side [Figure 1]. [8] Throughout the treatment, all cases were monitored for possible complications (non-union, impingement, osteonecrosis and stiffness of the shoulder and neurological deficit). Samilson and Prieto criteria were used to classify potential glenohumeral arthritis and the Cruess classification was used for the stages of osteonecrosis. [16],[17]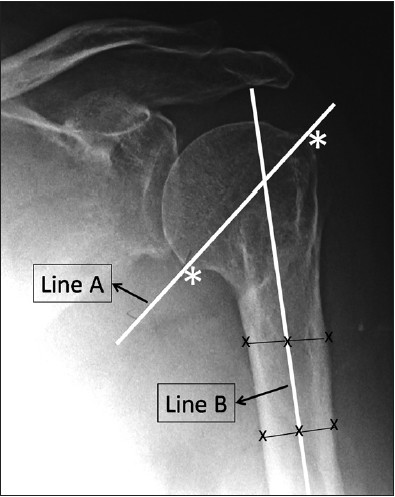 | Figure 1: Measurement of humeral neck-shaft angle. Line A is drawn between the tuberculum majus and inferior joint surface (asterisks) and represents the alignment of the neck. Line B represents the alignment of the humeral shaft. Neck-shaft angle is defined as the angle between the Line A and Line B
Click here to view |
Continuous variables were stated as mean and standard deviation and categorical variables as percentages and frequency distribution. Repeated measurements were analyzed using the Friedman test. Mann-Whitney test was used to compare the independent samples. The Spearman correlation test was used to determine relationships between variables. A P < 0.05 was considered statistically significant.
 Results Results | |  |
During the course of this study, three cases died for various reasons and two cases experienced cerebrovascular attack, which caused plegia at the injured side; thus, these patients were excluded from the study. Remaining 29 patients who were able to be followed-up for at least 1 year were included in the final analysis.
There were 21 female and 8 male patients. The mean age of the patients was 78 ± 8,6 years (range 65-93 years). The mechanism of injury was a simple fall in 24 patients, fall from height in two patients and traffic accident in three patients. Fifteen fractures involved the right upper extremity and the remaining 14 involved the left upper extremity. In 13 patients, fractures involved the dominant extremity. A total of 22 patients could not be operated due to the reason for high risk anesthesia (ASA IV). Seven patients were ASA III, but they all rejected surgical treatment. There were 15 Neer type three-part, 9 Neer type two-part and 5 Neer type four-part fractures.
The mean follow-up period was 18.2 ± 4.07 months (range 12-26 months). Mean CS at 3 th months, 6 th months and the final follow-up were 41.8 ± 9.0, 60.6 ± 12.6 and 72.2 ± 14.0 points respectively. Throughout the follow-up period, the CS was seen to significantly increase (P = 0.0001). According to CS scoring, 18 cases (62%) had excellent (>70 points), seven cases (24%) satisfactory (50-70 points) and four cases (14%) had poor results (<50 points). The mean VAS score at the final follow-up was 1.3 ± 1.5 points (range 0-5). The mean Q-DASH score at the final follow-up was 25.4 ± 20.1 (range 2.3-70.5) points. At the final follow-up, a mean range of motion (forward flexion) of 75% (range 30-96%) was determined to have been regained when a comparison was made with the healthy shoulder [Figure 2]. | Figure 2: A 79-year-old female patient with Neer type two-part fracture. (a) Initial shoulder antero-posterior shoulder radiograph. (b) Final follow-up radiograph. (c) 3D computerized tomography (CT) and (d) coronal CT reconstruction. (e and f) Clinical appearance of the patient at the final follow-up at 22 months
Click here to view |
Bony union was achieved in 28 cases (96.5%). The average duration of union was 5.2 ± 0.7 months (range 4-6 months). There was non-union in one case, thus humeral head neck-shaft angle could not be measured in this case. The mean humeral head neck-shaft angle was 63.8 ± 16.2° (range 26-88). 13 cases united with varus deformity and 15 cases united with valgus deformity. No significant relationship was found between functional outcomes (CS, Q-DASH and VAS at final follow-up) and humeral head neck-shaft angle. CS, ρ = −0.031 P = 0.876, Q-DASH, ρ = −0.129 P = 0.512 and VAS ρ = −0.193 P = 0.325). However, there was a significant reverse relation between the Neer type (humeral head comminution) and CS (ρ = −0.665 P = 0.0001). On the other hand, Q-DASH and VAS scores did not correlate with Neer type (Q-DASH r = 0.113 P = 0.558, VAS r = 0.264 P = 0.167). Functional results were compared between valgus malunited and varus malunited subgroups, again there were no significant difference between groups (CS 0.650, Q-DASH P = 0.821 and VAS P = 0.928 respectively). The CS was not related with the age of the patient (r = −0.298 P = 0.117).
In four cases, avascular necrosis of the humeral head was determined (two cases stage 2, one case stage 4 and one case stage 5). One case had pseudoarthrosis and one case had stage 2 glenohumeral osteoarthritis.
 Discussion Discussion | |  |
This prospective study investigated the relationship between the final geometry of the humeral head and the functional results in elderly patients who were treated conservatively for displaced PHFs. Our hypothesis was final geometry of the humeral head dictates the functional results. However, we could not show any relationship between the final geometry of the humeral head and the functional outcomes in this study. Although all of our cases united with either varus or valgus deformity, functional outcomes were excellent or satisfactory in 25 cases (86%). In elderly patients, full glenohumeral movement is not essential for daily activities and normal shoulder function should not be expected even in healthy subjects. [18] In the current study, the functional level of the patients prior to the fracture could not be obtained. However, at the final follow-up, pain scores were low and an average of 75% shoulder movement was regained.
Treatment of humerus proximal fractures in the elderly is an unsolved and difficult problem for orthopedic surgeons. However, recent literature advocates the conservative treatment as a valid option, despite complete functional recovery could not be obtained. [7],[8],[9],[19] Current literature contains conflicting knowledge about the functional and radiologic results of displaced proximal humerus fractures in the elderly. Zyto et al. recommended conservative treatment, despite lower functional scores and non-anatomic reduction of fractures in their two different studies. [9],[20] Hanson et al. reported that initial fragmentation and displacement of the fracture determined the functional results after the conservative treatment in elderly patients. [7] However, Court-Brown and McQueen suggested that age of the patient is another important factor that affected the functional results as well as the initial fracture type. [8],[18] On the other hand, Rasmussen et al. claimed that functional results are independent from the age. [15] Furthermore, Yόksel et al. proposed that neither the initial fragmentation nor the age of the patient determine the final functional status of the patients. [10] In our study, we have found that the initial fracture fragmentation (Neer type) is strongly related with the functional results, however the age is not. Based on our results and the literature, fracture comminution is a prognostic factor for the final functional recovery. Thus, estimation of the functional loss at the initial admission may lead the management of these fractures and realize the patients' expectations.
According to the recent literature, coronal angulations of the proximal humerus are well tolerated in the elderly. Therefore, the final radiological outcomes do not reflect the functional results. [7],[8] Court-Brown and McQueen reported no association between the varus angulation and the shoulder functions and the pain. He claimed that the poor outcomes are related with the increasing age. [8] Yόksel et al. proposed that there is no need for reduction due to the fact that there is no relation between the head-neck angulations and the CS. [10] Similarly, in our study, contrary to our initial hypothesis, we could not show any relationship between the varus or valgus malunions and the CS. However, contrary reports are also found in the relevant literature. Blonna et al. proposed that varus angulation more 25° results with poor functional outcomes; therefore they suggested surgical intervention for these fractures. [11] Furthermore, Sόdkamp et al. claimed that varus angulation more 30° decreases CS significantly. [12] Majority of our patients (86%) resulted with satisfactory functional outcomes, so we do not suggest surgery for these patients.
Although various rates have been reported in literature, at the final follow-up of our cases, 13.7% were determined as having osteonecrosis. [19],[20] The mean age of our cases with osteonecrosis was 84 years, but there was an insufficient number to make an association with age. Advanced stage osteonecrosis in the shoulder joint is linked to severe functional limitations. Therefore, the elderly age group with a high number of fragments should be kept under observation after conservative treatment for the possibility of osteonecrosis.
This study has some strengths limitations. We analyzed limited number of patients and the study group consisted of heterogeneous cases in terms of fracture classification. As conservative treatment was the only treatment option applied, there was no possibility to compare with alternative treatment methods. The mean follow-up period of 18 months may be short. However, this study is a prospective study and no patients were lost from follow-up.
 Conclusion Conclusion | |  |
Conservative treatment is a viable option for displaced PHFs in the elderly. Despite varus or valgus malunion, the functional results are satisfactory. The results of this study show that initial fragmentation has a negative effect on the functional results. However, the changed position of the humeral head on coronal plane does not affect the final functional results.
 Acknowledgment Acknowledgment | |  |
The Author would like to thank the patient for providing consent to use his photograph in this article.
 References References | |  |
| 1. | Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res 2006;442:87-92. 
[PUBMED] |
| 2. | Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: Epidemiology and outcome in 507 cases. Acta Orthop Scand 2003;74:580-5. 
[PUBMED] |
| 3. | Neer CS 2 nd . Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077-89. 
|
| 4. | Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults-A systematic review of management. Injury 2001;32:363-72. 
[PUBMED] |
| 5. | Lanting B, MacDermid J, Drosdowech D, Faber KJ. Proximal humeral fractures: A systematic review of treatment modalities. J Shoulder Elbow Surg 2008;17:42-54. 
[PUBMED] |
| 6. | Smith AM, Mardones RM, Sperling JW, Cofield RH. Early complications of operatively treated proximal humeral fractures. J Shoulder Elbow Surg 2007;16:14-24. 
[PUBMED] |
| 7. | Hanson B, Neidenbach P, de Boer P, Stengel D. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg 2009;18:612-21. 
[PUBMED] |
| 8. | Court-Brown CM, McQueen MM. The impacted varus (A2.2) proximal humeral fracture: Prediction of outcome and results of nonoperative treatment in 99 patients. Acta Orthop Scand 2004;75:736-40. 
[PUBMED] |
| 9. | Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury 1998;29:349-52. 
[PUBMED] |
| 10. | Yüksel HY, Yilmaz S, Akşahin E, Celebi L, Muratli HH, Biçimoğlu A. The results of nonoperative treatment for three- and four-part fractures of the proximal humerus in low-demand patients. J Orthop Trauma 2011;25:588-95. 
|
| 11. | Blonna D, Rossi R, Fantino G, Maiello A, Assom M, Castoldi F. The impacted varus (A2.2) proximal humeral fracture in elderly patients: Is minimal fixation justified? A case control study. J Shoulder Elbow Surg 2009;18:545-52. 
|
| 12. | Südkamp NP, Audigé L, Lambert S, Hertel R, Konrad G. Path analysis of factors for functional outcome at one year in 463 proximal humeral fractures. J Shoulder Elbow Surg 2011;20:1207-16. 
|
| 13. | Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group. Development of the QuickDASH: Comparison of three item-reduction approaches. J Bone Joint Surg Am 2005;87:1038-46. 
|
| 14. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;214:160-4. 
[PUBMED] |
| 15. | Rasmussen S, Hvass I, Dalsgaard J, Christensen BS, Holstad E. Displaced proximal humeral fractures: Results of conservative treatment. Injury 1992;23:41-3. 
[PUBMED] |
| 16. | Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am 1983;65:456-60. 
[PUBMED] |
| 17. | Hattrup SJ, Cofield RH. Osteonecrosis of the humeral head: Relationship of disease stage, extent, and cause to natural history. J Shoulder Elbow Surg 1999;8:559-64. 
[PUBMED] |
| 18. | Court-Brown CM, Garg A, McQueen MM. The translated two-part fracture of the proximal humerus. Epidemiology and outcome in the older patient. J Bone Joint Surg Br 2001;83:799-804. 
[PUBMED] |
| 19. | Schai P, Imhoff A, Preiss S. Comminuted humeral head fractures: A multicenter analysis. J Shoulder Elbow Surg 1995;4:319-30. 
[PUBMED] |
| 20. | Zyto K, Ahrengart L, Sperber A, Törnkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br 1997;79:412-7. 
|
[Figure 1], [Figure 2]
|
