| |


 |
| Year : 2013 | Volume
: 7
| Issue : 3 | Page : 83-90 |
|
|
|
|
|
ORIGINAL ARTICLE Non-insertional tendinopathy of the subscapularis
Brian D Dierckman, Nirav R Shah, Connor R Larose, Stacey Gerbrandt, Mark H Getelman
Southern California Orthopedic Institute, CA 91405, USA
Correspondence Address:
Mark H Getelman
Southern California Orthopedic Institute, 6815 Noble Ave., Van Nuys, CA 91405
USA
 Source of Support: Funded by Depuy Mitek, Smith and Nephew as
well as Donjoy Medical., Conflict of Interest: Drs. Dierckman, Shah and
LaRose have no conflicts of interest to report. Mrs. Stacey Gerbrandt has
no conflicts of interest to report. Dr. Getelman is a paid consultant for Depuy
Mitek, and his fellowship at Southern California Orthopedic Institute.
DOI: 10.4103/0973-6042.118876

|
|
|
|
| Date of Web Publication | 25-Sep-2013 |
 Abstract Abstract | | |
Purpose: (1) Describe a previously unreported finding involving the intra-articular portion of the subscapularis, the Conrad lesion. (2) Describe a novel classification system for the spectrum of non-insertional tendinopathy of the subscapularis. (3) Report the outcomes of surgical treatment of this spectrum of pathology.
Materials and Methods: Outcomes of 34 patients (23 males and 11 females, mean age 60.5 ± 7.5) with non-insertional tendinopathy of the subscapularis treated arthroscopically were retrospectively reviewed. All patients had anterior shoulder pain with no weakness during belly-press testing and no subscapularis footprint involvement on magnetic resonance imaging. All patients were managed with subscapularis tendon debridement and side-to-side repair along with treatment of concomitant pathology.
Results: Seven patients had a Type I lesion (so-called Conrad lesion) - a nodule on the leading edge of the subscapularis. Eighteen patients had a Type II lesion - a visible split tear with degeneration in the upper ½ of the intra-articular tendon. Nine patients had a Type III lesion - more extensive splitting in the tendon with advanced tendon degeneration. At a mean follow-up of 24 months, 97% of patients were completely satisfied. Significant improvements were seen in forward elevation (152 ± 12° to 172 ± 5°, P < 0.001) and visual analog scale pain scores (5.9 ± 1.7-0.6 ± 1.0, P < 0.001). Internal rotation strength and external rotation motion at the side were maintained. ASES scores averaged 95.4 ± 7.4, disabilities of arm, shoulder and hand scores averaged 6.19 ± 9.8, Western Ontario Rotator Cuff scores averaged 91.7 ± 9.3 and the average University of California at Los Angeles score was 33.1 ± 2.4.
Conclusions: We present a previously unreported finding of the subscapularis, the Conrad lesion, along with a novel classification system for non-insertional tendinopathy of the subscapularis. Arthroscopic treatment of this spectrum of tendinopathy along with concomitant shoulder pathology eliminated pain and improved patient outcomes without detrimental effects.
Level of Evidence: IV, Retrospective Case Series.
Keywords: Non-insertional, subscapularis, tendinopathy
How to cite this article:
Dierckman BD, Shah NR, Larose CR, Gerbrandt S, Getelman MH. Non-insertional tendinopathy of the subscapularis. Int J Shoulder Surg 2013;7:83-90 |
 Introduction Introduction | |  |
Tears of the subscapularis tendon have received significantly more recognition as a source of shoulder pain and dysfunction over the past decade. [1],[2],[3],[4],[5],[6],[7],[8] Although their incidence is much lower than tears of the supraspinatus tendon, subscapularis tears have to date been under-reported. [5],[9] Reasons cited to explain this discrepancy include inadequate arthroscopic visualization as well as incomplete understanding of the anatomy and function of the upper subscapularis. [9],[10],[11],[12] Knowledge of the subscapularis has improved over the past decade and can be directly linked to advancements in arthroscopic shoulder surgery. [1],[13],[14] Open treatment of subscapularis tendon tears has been recommended in the past, [5],[15],[16],[17],[18] although recent studies reporting the results of arthroscopic subscapularis repair show comparable clinical outcomes. [1],[6],[8],[18],[19]
Current classification systems of subscapularis tears focus on involvement of the tendinous insertion (partial thickness, retracted, articular-sided, etc.). [20] Non-insertional pathology of the subscapularis, albeit uncommon, has not been described or included in any of the current classification systems. Anecdotally, several surgeons have communicated with the senior author regarding their experiences with non-insertional tendinopathy of the subscapularis. They reported noting similar abnormalities of the intra-articular subscapularis and often treated them with debridement and/or repair. Longitudinal split tears have been mentioned in conjunction with footprint disruptions, [13] but no studies have detailed intra-articular subscapularis pathology without disruption of the footprint insertion.
Several years ago, the senior author encountered a patient with anterior shoulder pain thought to be due to biceps pathology. Following the failure of conservative care, patient underwent arthroscopic evaluation. At arthroscopy, patient was found to have a normal appearing biceps tendon and isolated pathology of the upper subscapularis - specifically, a previously undescribed nodule (the Conrad lesion) on the leading edge of the subscapularis tendon adjacent to the middle glenohumeral ligament (MGHL). The isolated nodule was debrided, revealing a "hidden" longitudinal split tear within the substance of the subscapularis, despite an otherwise normal appearing tendon on initial examination. This piqued the interest of the senior author and we have since collected a series of patients with non-insertional intra-articular subscapularis pathology. We suspect these lesions are a source of anterior shoulder pain and dysfunction and may remain as a pain generator if left untreated. We feel they may represent early lesions in the spectrum of subscapularis tears and warrant recognition to stimulate further investigation.
The purpose of this study is to present a unique entity within the spectrum of pathology of the subscapularis, the Conrad lesion. We also aim to present a novel classification system for intra-articular subscapularis tendinopathy not included in any of the previously reported classification systems. Finally, we will report our results following arthroscopic treatment of this subset of subscapularis pathology.
 Materials and Methods Materials and Methods | |  |
This is a retrospective study of one surgeon's experience treating non-insertional tendinopathy of the subscapularis. We included only those patients undergoing primary arthroscopic treatment of non-insertional subscapularis tendinopathy. The indications for surgery in this patient population were: Symptomatic rotator cuff tears or failure of non-operative management (physical therapy and/or corticosteroid injection) in patients with signs of anterior shoulder pain, impingement syndrome or evidence of rotator cuff tendinopathy on magnetic resonance imaging (MRI). No patients treated for concomitant pathology were excluded. Exclusion criteria included: Revision surgery and subscapularis tendon footprint involvement. Between January 2005 and December 2009, 84 arthroscopic subscapularis repairs were performed at our institution by the senior surgeon. Of these, 64 patients had visible tendinopathy of the intra-articular portion of the subscapularis without detachment from the lesser tuberosity and were contacted for the study. 20 patients with tendon detachment from the subscapularis footprint were excluded. 34 patients agreed to participate in the study and constituted the study group. Of the 30 patients who did not participate, 18 patients could not be contacted while 12 patients declined participation due to work and travel commitments.
The study group included 23 males and 11 females with an average age of 60.5 ± 7.5 years (range: 41-78 years) at the time of operation. The average interval from the onset of symptoms to time of surgery was 11.3 ± 13.6 months. The dominant side was involved in 23 of the patients. At the time of surgery, 14 patients had retired, three were manual laborers and 17 were employed in occupations with the minimal physical labor. The average length of follow-up was 23.8 ± 14.0 months (range 12-58).
Evaluation
Each patient was evaluated by the senior author pre-operatively and by an independent examiner post-operatively. All patients were evaluated for a range of motion and strength and also completed the following questionnaires post-operatively: American Shoulder and Elbow Surgery (ASES), University of California at Los Angeles (UCLA), disabilities of arm, shoulder and hand (DASH), Western Ontario Rotator Cuff (WORC) and the short-form-36 (SF-36) health survey. Patients also responded with a yes or no answer to the written question, "are you satisfied with the overall results of your procedure?" Pain was graded using a standard visual analog scale (VAS) score from 0 to 10, while strength was assessed on a scale of 0-5 using the universally accepted classification on motor function. Testing of the subscapularis included strength evaluation with the belly-press test and associated pain response. Rotator cuff strength was evaluated using Jobe's test as well as external rotation with the arm at the side. Range of motion was evaluated in forward flexion, external rotation with the arm at the side as well as internal and external rotation with the arm in 90° of abduction.
Each patient was evaluated with plain radiographs both pre- and post-operatively. These radiographs included a true anteroposterior view of the glenohumeral joint with the arm in neutral rotation, an axillary view and a supraspinatus outlet view. The coracohumeral distance was measured on the axillary radiograph. All patients had a pre-operative MRI scan, which failed to reveal a tear involving the subscapularis footprint.
Operative technique
Following induction of general anesthesia, patient was placed in the lateral decubitus position with the arm in 70° of abduction and 20° of forward flexion with application of 10 pounds of balanced suspension. The 30° arthroscope was inserted through a standard posterior portal. The anterior midglenoid (AMG) portal was established using an inside-out technique over a Wissinger rod. A complete diagnostic arthroscopic examination was performed to identify all concomitant pathology needing to be addressed during the course of the procedure [Table 1].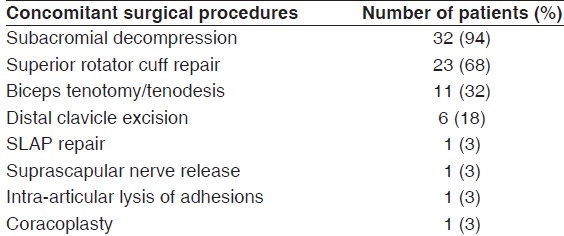 | Table 1: Concomitant procedures performed along with side-to-side repair of subscapularis tendinopathy
Click here to view |
Non-insertional intra-articular pathology of the subscapularis was readily identified during the diagnostic arthroscopy. A shaver in the AMG portal was used to debride the free edge of the subscapularis. Upon doing so, a longitudinal split tear was identified with concomitant degeneration/granulation tissue within the substance of the subscapularis tendon. Following debridement, the tendinous insertion remained intact and the longitudinal split tear was repaired in a side-to-side fashion with absorbable polydioxanone (PDS) suture, analogous to repair of longitudinal split tears in other cases of tendinopathy including the supraspinatus, tibialis anterior and peroneal tendons. [21],[22],[23] Repair was accomplished using the spectrum (Linvatec, Largo, FL) medium-sized crescent hook passed through the two sides of the split tear of the subscapularis tendon [Figure 1]a. We attempted to pass the crescent hook to a depth of roughly 5 mm on each side of the split tear to create a uniform repair, which prevents tissue bunching and limits capturing of the MGHL. A #1 PDS suture (Ethicon, Somerville, NJ) was passed into the joint and retrieved out the same AMG portal [Figure 1]b. The stitch was tied using a locking sliding knot reinforced with three reverse half hitches on alternating posts [Figure 1]c. Typically, one to two sutures were placed and the process was repeated if additional stitches were needed [Figure 1]d.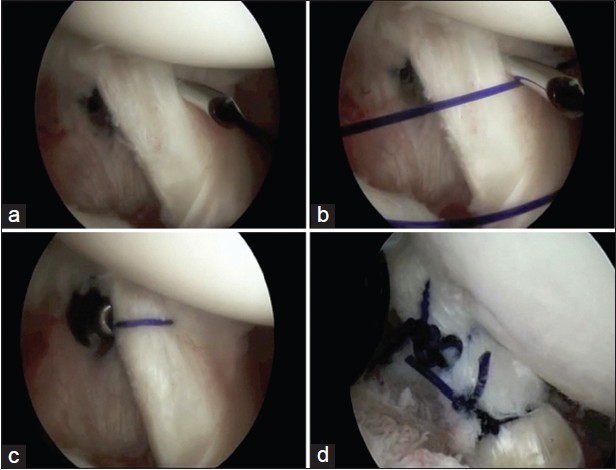 | Figure 1: (a) While viewing from the posterior portal in a right shoulder, a crescent-shaped suture passer was introduced through the anterior midglenoid (AMG) portal and passed through both sides of the split tear of the subscapularis tendon. (b) Polydioxanone suture is passed into the joint, and the suture passer is removed. (c) The free end of the suture is retrieved out the AMG portal and tied. (d) A view of a different patient, showing placement of two sutures for repair of a more extensive subscapularis tear
Click here to view |
Post-operatively, the shoulder was immobilized in a neutral rotation brace for 3 to 6 weeks based on other associated procedures. Elbow and hand motion was initiated immediately and passive supine external rotation in adduction was allowed to comfort immediately. Active shoulder range of motion was begun at 6 weeks post-operatively under the supervision of a physical therapist. Strengthening of the rotator cuff was permitted after 3 months with release to full activities at 4 to 6 months post-operatively.
Statistical analysis
Statistical analyses were performed with Excel (Microsoft, Redmond, WA) using the Wilcoxon rank-sum test. Statistical significance was set at P < 0.05.
 Results Results | |  |
Based on our findings at arthroscopy, we observed that intra-articular subscapularis tendinopathy occurred in one of three distinct patterns. We subsequently developed a classification scheme to delineate our findings, which we believe to be simple and reproducible. Advancing from Type I to III represents progressive tendinopathy in the leading edge of the tendon [Table 2]. The pattern observed most often was Conrad Type II tearing, seen in 18 (52.9%) patients. This was followed by Type III tears in 9 (26.5%) patients and Type I lesions in 7 (20.6%) patients.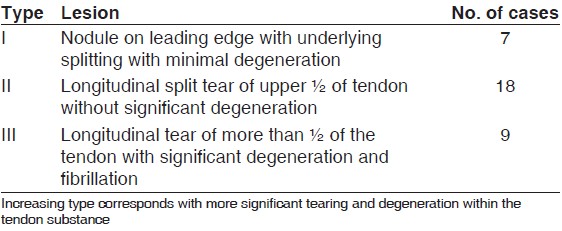 | Table 2: Conrad classification of non-insertional tendinopathy of the subscapularis
Click here to view |
In Type I lesions (the so-called Conrad lesion), there is a distinct, isolated nodule found on the leading edge of the subscapularis tendon adjacent to the MGHL [Figure 2]a. Upon debridement, Type I lesions are always found to have a "hidden" longitudinal intrasubstance split tear [Figure 2]b. The nodule itself is typically 3-4 mm in length; however, the underlying split can extend for a centimeter or more in total length and depth. There is histologically proven granulation tissue and degeneration within the tendon. Following debridement of the lesion to healthy appearing tissue, the insertion to the lesser tuberosity was inspected, revealing an intact footprint in all cases.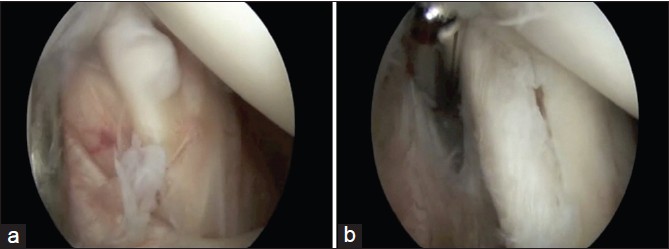 | Figure 2: (a) Arthroscopic view from the posterior portal of a Type I Conrad lesion in a right shoulder. Note the nodule (the so-called Conrad lesion) on the leading edge of the tendon. (b) Following debridement of the nodule, a longitudinal split tear is seen
Click here to view |
Type II lesions involve exposed split tearing of the superior 1/3-1/2 of the tendon. There is again granulation tissue and degeneration within the tendon as well as surrounding synovitis. The split may involve more extensive longitudinal tearing than Type I tears (two or more centimeters in length), but they do not have extensive delamination or fraying [Figure 3]. We feel these represent progression of Type I lesions, where the leading edge nodule has ruptured revealing the split tear on initial inspection. | Figure 3: Arthroscopic view from the posterior portal of a Type II Conrad lesion in a left shoulder. There is a visible split tear on the leading edge of the tendon and the remnant of a Type I Conrad lesion more medially
Click here to view |
Type III lesions are often seen in older patients. The tendinopathy appears more advanced as there is extensive degenerative tearing with advanced fraying and delamination; however, there is no tendon detachment from the tuberosity [Figure 4]. There is frequently less granulation tissue present, which may represent poor vascularity in these advanced lesions. | Figure 4: Arthroscopic view from the posterior portal of a Type III Conrad lesion in a right shoulder. There is extensive fraying and degeneration of the leading edge of the tendon
Click here to view |
No strength deficit was noted in any of the patients on subscapularis evaluation via the belly-press test. Those patients without concomitant supraspinatus tears often experienced isolated anterior shoulder pain as their only complaint. Pre-operative findings typically mimicked impingement syndrome, biceps tendon pathology and/or supraspinatus tears. Patients had decreased forward elevation to an average of 151.8 ± 11.9° and decreased strength to Jobe's testing, with an average of 4.0 ± 0.3 on a scale from 0 to 5. On MRI, no specific signs were identified other than tendinopathy of the subscapularis [Figure 5]a-c. Minimal intratendinous signal abnormalities were seen in Type I lesions while extensive signal abnormalities were seen in Type III lesions. No subscapularis footprint detachment was identified and no fatty infiltration or atrophy of the subscapularis muscle belly (suggestive of footprint detachment) was seen.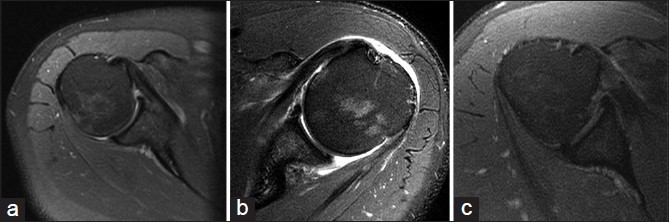 | Figure 5: Axial magnetic resonance images of three patients with non-insertional longitudinal split tears of the subscapularis. (a) Image from a patient with a Type I tear. Note intact subscapularis footprint and minimal tendinopathy. (b) Image from a patient with a Type II tear. Note the intact subscapularis footprint and mild tendinopathy. (c) Image from a patient with a Type III tear. Note the intact subscapularis footprint with extensive tendinopathy
Click here to view |
At follow-up evaluation performed at an average of 23.8 ± 14.0 months post-operatively (range: 12-58 months), 33 of 34 (97.0%) patients were satisfied with the results of their surgery. The one unsatisfied patient underwent subsequent surgery to the ipsilateral shoulder 2 months prior to final evaluation after sustaining a fall. He initially underwent repair of a supraspinatus tear along with repair of a Type II Conrad lesion, at repeat surgery evaluation of his subscapularis tendon revealed healing of his previous longitudinal tear [Figure 6].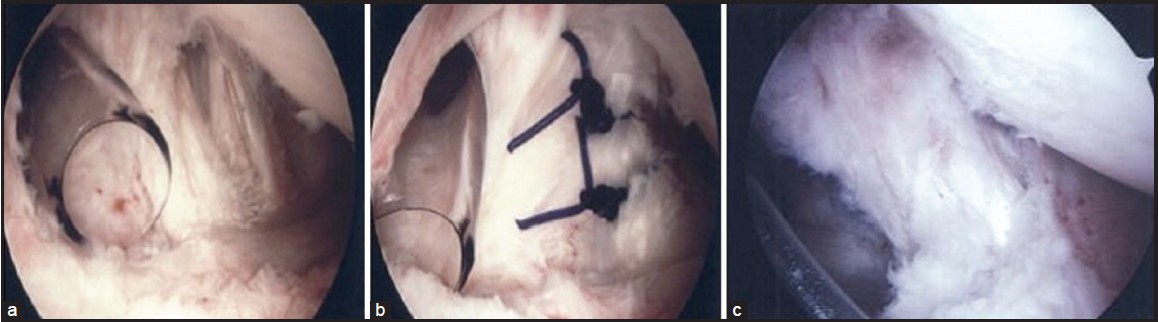 | Figure 6: Second-look arthroscopic views from the posterior portal of a patient with a Type II Conrad tear of the right shoulder. (a) Posterior view during initial arthroscopy showing a degenerative split tear in the tendon consistent with a Type II tear. (b) View at initial arthroscopy following repair of the Type II tear with two polydioxanone sutures. (c) View of a healed Type II Conrad tear at second-look arthroscopy
Click here to view |
Patients had marked improvements in subjective and objective shoulder function [Table 3]. The mean VAS pain scored improved significantly from 5.9 ± 1.7 points pre-operatively to 0.6 ± 1.0 points post-operatively (P < 0.001). Forward elevation also improved from 151.8 ± 11.9 (range: 130-180)° pre-operatively to 173.1 ± 2.8 (range: 160-180)° post-operatively (P < 0.001). However, no difference was observed in external rotation or subscapularis strength compared with pre-operative levels. When comparing the operative to the non-operative side, no statistical differences were found at final follow-up.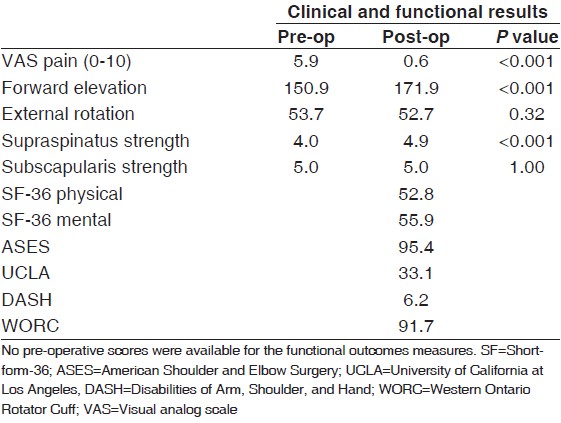 | Table 3: Results of clinical and functional assessment following arthroscopic treatment of non-insertional subscapularis tendinopathy
Click here to view |
Post-operative functional outcomes are presented in [Table 3]. SF-36 scores on the physical domain averaged 52.8 ± 6.7 (range: 37.8-61.2) while the scores on the mental domain averaged 55.9 ± 6.2 (range: 33.7-64.1). The normative score for the U.S. population is set at 50 for both domains. Averages on the other outcomes measures revealed an ASES score of 95.4 ± 7.4 (range: 73.3-100), a DASH score of 6.2 ± 9.8 (range: 0-39.2) and a WORC score of 91.7 ± 9.3 (range: 63.9-100). In addition, the average UCLA score was 33.1 ± 2.4, with all participants reporting good/excellent results (score ≥ 27).
Comparison of functional outcomes between patients with repair of a superior rotator cuff tear along with a subscapularis longitudinal split tear and those with isolated repair of a subscapularis longitudinal split tear revealed no statistically significant differences [Table 4].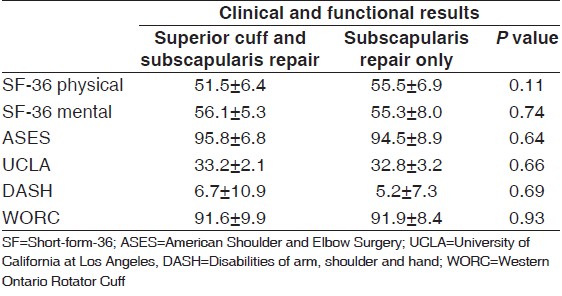 | Table 4: Comparisons of results between patients undergoing repair of a superior cuff tear and subscapularis tendinopathy with those undergoing treatment of subscapularis tendinopathy only
Click here to view |
Examination of the coracohumeral distance on the pre-operative axillary radiograph revealed an average distance of 8.7 ± 4.1 mm (range: 2.0-17.7 mm). 10 patients had an interval less than 6 mm while 19 patients had an interval greater than 8 mm. Only one patient underwent coracoplasty for arthroscopic signs of coracoid impingement and had a coracohumeral distance that measured 6.2 mm. No signs of coracoid impingement (synovitis, fraying of sub-coracoid soft-tissues) were observed in any other patient, even in those with a coracohumeral distance less than 6 mm. No patients have required repeat surgery with coracoplasty for signs of coracoid impingement since we began collecting our series of patients.
No patients in this series developed a complication directly related to the surgery.
 Discussion Discussion | |  |
We present the first reported series of patients with very specific and unique intra-articular subscapularis tendinopathy. The primary intent of our study is to raise awareness of these non-insertional lesions as we suspect they represent early degeneration within the spectrum of subscapularis pathology. While several subscapularis tear classifications exist, this spectrum of pathology is not included in any of the current systems. [20] Little has been published regarding the degenerative process leading to subscapularis tears, but it seems reasonable to assume a similar degenerative process as in the supraspinatus is responsible.
Previous studies have reported on the clinical results of arthroscopic subscapularis repair, but these all detailed tears involving the subscapularis footprint. Burkhart and Tehrany initially reported their results on arthroscopic treatment of subscapularis tears in 25 patients, eight of whom had isolated repairs. [6] Good to excellent results were achieved in 92% of patients, with improvements in pain, forward elevation and functional outcome measures (UCLA scores improved from 10.7 to 30.5). Similarly, Bennett reported results in 8 patients with isolated subscapularis tears treated arthroscopically with a minimum of 2-year follow-up. [8] Significant improvements were made in all outcomes assessed, including VAS pain score, Constant score, and ASES score (improved from 16 to 74). Bartl et al. reported on isolated subscapularis tears with significant improvements in strength and functional capabilities in 21 patients as well. [19] Post-operative MRI confirmed maintenance of repair durability in 20 shoulders at an average follow-up of 21 months. Similarly, Lafosse et al. reported improved objective shoulder function (UCLA scores improved from 16 to 32) and structural integrity of the subscapularis via computed tomography angiography in 15 of 17 patients. [1]
It is unclear whether meaningful comparisons between our results and those of others can be made as previous reports on subscapularis repairs involved tendon footprint detachment from the lesser tuberosity. [3],[4],[10],[16],[17],[18] Supraspinatus tendon disease with footprint disruption represents more advanced tendon degeneration and accompanying shoulder dysfunction in comparison to intratendinous tears. [21] It seems likely that the functional results following side-to-side repair of non-insertional split tears would, at a minimum, reveal results equal or superior to those repairs involving tendon detachment. We feel, it is more likely that treatment of isolated non-insertional tendinopathy would lead to improved functional results compared with repair of footprint avulsions for two reasons. First, pre-operative functional scores of patients with intra-articular subscapularis tendinopathy with an intact footprint would be expected to be higher than more advanced tears involving disruption of the footprint, which would likely lead to higher post-operative scores as well. Unfortunately, pre-operative functional scores on our patients were not available. It is thus unknown, but likely, that patients with these non-insertional lesions are less debilitated pre-operatively than patients with full-thickness lesions. Secondly, side-to-side repair of intratendinous tears is performed and may prevent further tear propagation involving the footprint - and as such, these less advanced tears would be expected to have better outcomes. [24] Despite this, functional outcomes for repairs have not correlated well with anatomic healing to date, at least for the supraspinatus tendon. [25],[26]
The present study did not aim to identify the specific etiology of non-insertional tendinopathy of the subscapularis. Previous studies have identified intratendinous degeneration as a factor in subscapularis tearing. Sakurai et al. showed degeneration of the subscapularis tendon in 17 of 46 cadaveric shoulders. [27] The degeneration was always articular-sided tearing on the superior (leading) edge of the tendon, which was also seen in our patients. Sano et al. showed similar results, with articular-sided degeneration being more prominent than bursal-sided tearing. [28] Despite these findings, there were no comments on lesions without footprint involvement. These studies do emphasize the degree that age-related degeneration plays in subscapularis tears and the histopathologic findings in our patients support degeneration as a likely etiology. All pathology occurred on the articular side of the tendon and in addition, all our patients' tears showed substantial intrasubstance involvement with granulation tissue and degeneration.
Other proposed mechanisms leading to subscapularis tearing include that of anterosuperior impingement as reported by Gerber and Sebesta. [29] They documented increased contact and tensile stress on the deep portion of the subscapularis in a position of forward elevation and internal rotation as the tendon is compressed between the lesser tuberosity and the glenoid/labrum. This impingement explains the increased rate of injury of the biceps tendon, superior glenohumeral ligament and coracohumeral ligament associated with a subscapularis tear in their population. However, aside from some fraying of the biceps tendon in 11 patients, these lesions were not seen in our study population. Nevertheless, anterosuperior impingement may have contributed to the partial articular-sided tears seen in some of our patients.
Lo and Burkhart have popularized the concept of subcoracoid impingement, whereby decreased space between the coracoid and humeral head leads to impingement and tearing of the subscapularis insertion via the "wringer-roller effect." [30] Subcoracoid stenosis has been defined by a coracohumeral interval of less than 6 mm, where a normal interval is 8 mm to 11 mm in both imaging and anatomic studies. [31],[32],[33],[34],[35] Although we found patients with decreased coracohumeral intervals on plain radiographs, we observed only one instance of subcoracoid stenosis/impingement during arthroscopy, with pathologic tissue visible within the subcoracoid space. This discrepancy may be due to inaccuracy of measuring the coracohumeral interval with plain radiographs. In our population however, functional results were not compromised in patients in which coracoplasty was not performed as no patients have required repeat surgery. It is unlikely that subcoracoid stenosis plays a pivotal role in the development of the lesions seen in our study group.
It is our goal to raise awareness of this spectrum of pathology and describe our early experience in a limited group of patients. Since these lesions have not been previously described, our primary intent was to present a simple classification system based upon specific subscapularis pathology. We suspect these lesions represent progressive degeneration in the spectrum of subscapularis tears. Unfortunately, until natural history studies are completed, our classification system will have limited influence on treatment recommendations. However, we hope it will provide a benchmark for other investigators to build upon. Admittedly, our classification system does not provide varying treatment recommendations based on type, as we have chosen to proceed with debridement followed by repair in all types thus far. With further study, we hope to determine the preferred treatment for each of the three types of subscapularis tendinopathy.
It is possible that there may have been associated footprint involvement not seen on MRI or during arthroscopy. These lesions may have been poorly visualized and inadvertently missed as this is a commonly reported issue regarding arthroscopic evaluation and treatment of subscapularis tears. [10],[13] We specifically attempted to minimize this possibility by utilizing specific techniques recommended in the literature. [10],[36] We routinely internally rotated the arm and applied a posteriorly directed force to translate the humeral head. A 70° arthroscope was also made available, although we did not use it routinely.
There are weaknesses of our study that need to be addressed. One limitation is the small number of patients with an isolated longitudinal split tear of the subscapularis (11). Since 23 of the 34 patients underwent associated supraspinatus repair as well, it is unclear whether the excellent results seen in our patient population would have been the same had the subscapularis lesion been left untreated. However, as shown by Sano et al. and Uhthoff and Sano degeneration of the tendon can lead to weakening of the insertion point and eventual mechanical failure of the tendon itself. [37],[38] Therefore, we suspect that the pathology reported in our study represents tendinopathy and early tearing and can be a source of anterior shoulder pain. As such, we feel the pathology encountered should be treated with appropriate debridement and subsequent repair so as to possibly prevent further subscapularis tear progression. No detrimental effects were seen in our population following side to side suture repair of the subscapularis lesion, suggesting it is safe and it may potentially alleviate continued degeneration into a full-thickness tear. No patient has required additional surgery for tearing to the subscapularis following our treatment. In fact, during the second look arthroscopy in our 1 patient who sustained the traumatic re-injury, it was confirmed that the split tear had healed at 12 months following repair.
Due to the retrospective design of our study, pre-operative functional measures were unavailable and prevented direct calculations of improvement related to the surgery. However, significant improvements in VAS and objective measures were achieved in our patient population. Furthermore, current validated outcomes measures focus on the superior rotator cuff, inadequately representing the functional contributions of the subscapularis. [18],[39],[40] Therefore, even if pre-operative data on functional outcome measures were available, changes in scores would likely be primarily attributable to treatment of the supraspinatus tendon rather than repair of the subscapularis. Accordingly, it is not possible to clearly delineate the pre-operative disability and associated pain attributable to these longitudinal tears due to confounding contributions of other pathology.
 Conclusion Conclusion | |  |
Our primary intent is to increase awareness of non-insertional subscapularis tendinopathy by describing the Conrad lesion, presenting a classification of non-insertional pathology of the subscapularis, and reporting our early experience in treating this spectrum of tendinopathy. Results of the present study show that debridement and repair of longitudinal split tears of the subscapularis can result in healing of the subscapularis tendon and when treated along with concomitant pathology, can lead to improvements in pain and function of the shoulder without detrimental effects. Further studies are needed to better understand the clinical significance and natural history of this previously unreported spectrum of pathology as well as the preferred method of treatment for the different types of tendinopathy.
 References References | |  |
| 1. | Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am 2007;89:1184-93. 
|
| 2. | Ticker JB, Burkhart SS. Why repair the subscapularis? A logical rationale. Arthroscopy 2011;27:1123-8. 
|
| 3. | Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: An anatomic and clinical investigation. Arthroscopy 2008;24:997-1004. 
|
| 4. | Ide J, Tokiyoshi A, Hirose J, Mizuta H. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg Am 2007;89:2378-88. 
|
| 5. | Flury MP, John M, Goldhahn J, Schwyzer HK, Simmen BR. Rupture of the subscapularis tendon (isolated or in combination with supraspinatus tear): When is a repair indicated? J Shoulder Elbow Surg 2006;15:659-64. 
|
| 6. | Burkhart SS, Tehrany AM. Arthroscopic subscapularis tendon repair: Technique and preliminary results. Arthroscopy 2002;18:454-63. 
|
| 7. | Kim TK, Rauh PB, McFarland EG. Partial tears of the subscapularis tendon found during arthroscopic procedures on the shoulder: A statistical analysis of sixty cases. Am J Sports Med 2003;31:744-50. 
|
| 8. | Bennett WF. Arthroscopic repair of isolated subscapularis tears: A prospective cohort with 2- to 4-year follow-up. Arthroscopy 2003;19:131-43. 
|
| 9. | Adams CR, Schoolfield JD, Burkhart SS. Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy 2010;26:1427-33. 
|
| 10. | Adams CR, Schoolfield JD, Burkhart SS. The results of arthroscopic subscapularis tendon repairs. Arthroscopy 2008;24:1381-9. 
|
| 11. | Bennett WF. Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of "hidden" rotator interval lesions. Arthroscopy 2001;17:173-80. 
|
| 12. | Koo SS, Burkhart SS. Subscapularis tendon tears: Identifying mid to distal footprint disruptions. Arthroscopy 2010;26:1130-4. 
|
| 13. | David TS, Bravo H, Scobercea R. Arthroscopic visualization of subscapularis tendon lesions. Orthopedics 2009;32:9. 
|
| 14. | Lo IK, Burkhart SS. The comma sign: An arthroscopic guide to the torn subscapularis tendon. Arthroscopy 2003;19:334-7. 
|
| 15. | Kreuz PC, Remiger A, Lahm A, Herget G, Gächter A. Comparison of total and partial traumatic tears of the subscapularis tendon. J Bone Joint Surg Br 2005;87:348-51. 
|
| 16. | Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br 1991;73:389-94. 
|
| 17. | Deutsch A, Altchek DW, Veltri DM, Potter HG, Warren RF. Traumatic tears of the subscapularis tendon. Clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med 1997;25:13-22. 
|
| 18. | Edwards TB, Walch G, Sirveaux F, Molé D, Nové-Josserand L, Boulahia A, et al. Repair of tears of the subscapularis. J Bone Joint Surg Am 2005;87:725-30. 
|
| 19. | Bartl C, Salzmann GM, Seppel G, Eichhorn S, Holzapfel K, Wörtler K, et al. Subscapularis function and structural integrity after arthroscopic repair of isolated subscapularis tears. Am J Sports Med 2011;39:1255-62. 
|
| 20. | Lyons RP, Green A. Subscapularis tendon tears. J Am Acad Orthop Surg 2005;13:353-63. 
|
| 21. | Uchiyama Y, Hamada K, Khruekarnchana P, Handa A, Nakajima T, Shimpuku E, et al. Surgical treatment of confirmed intratendinous rotator cuff tears: Retrospective analysis after an average of eight years of follow-up. J Shoulder Elbow Surg 2010;19:837-46. 
|
| 22. | Grundy JR, O'Sullivan RM, Beischer AD. Operative management of distal tibialis anterior tendinopathy. Foot Ankle Int 2010;31:212-9. 
|
| 23. | Heckman DS, Reddy S, Pedowitz D, Wapner KL, Parekh SG. Operative treatment for peroneal tendon disorders. J Bone Joint Surg Am 2008;90:404-18. 
|
| 24. | Brockmeier SF, Dodson CC, Gamradt SC, Coleman SH, Altchek DW. Arthroscopic intratendinous repair of the delaminated partial-thickness rotator cuff tear in overhead athletes. Arthroscopy 2008;24:961-5. 
|
| 25. | Meyer M, Klouche S, Rousselin B, Boru B, Bauer T, Hardy P. Does arthroscopic rotator cuff repair actually heal? Anatomic evaluation with magnetic resonance arthrography at minimum 2 years follow-up. J Shoulder Elbow Surg 2012;21:531-6. 
|
| 26. | Gulotta LV, Nho SJ, Dodson CC, Adler RS, Altchek DW, MacGillivray JD, et al. Prospective evaluation of arthroscopic rotator cuff repairs at 5 years: Part II - Prognostic factors for clinical and radiographic outcomes. J Shoulder Elbow Surg 2011;20:941-6. 
|
| 27. | Sakurai G, Ozaki J, Tomita Y, Kondo T, Tamai S. Incomplete tears of the subscapularis tendon associated with tears of the supraspinatus tendon: Cadaveric and clinical studies. J Shoulder Elbow Surg 1998;7:510-5. 
|
| 28. | Sano H, Ishii H, Trudel G, Uhthoff HK. Histologic evidence of degeneration at the insertion of 3 rotator cuff tendons: A comparative study with human cadaveric shoulders. J Shoulder Elbow Surg 1999;8:574-9. 
|
| 29. | Gerber C, Sebesta A. Impingement of the deep surface of the subscapularis tendon and the reflection pulley on the anterosuperior glenoid rim: A preliminary report. J Shoulder Elbow Surg 2000;9:483-90. 
|
| 30. | Lo IK, Burkhart SS. The etiology and assessment of subscapularis tendon tears: A case for subcoracoid impingement, the roller-wringer effect, and TUFF lesions of the subscapularis. Arthroscopy 2003;19:1142-50. 
|
| 31. | Lo IK, Parten PM, Burkhart SS. Combined subcoracoid and subacromial impingement in association with anterosuperior rotator cuff tears: An arthroscopic approach. Arthroscopy 2003;19:1068-78. 
|
| 32. | Gerber C, Terrier F, Zehnder R, Ganz R. The subcoracoid space. An anatomic study. Clin Orthop Relat Res 1987;215:132-8. 
|
| 33. | Friedman RJ, Bonutti PM, Genez B. Cine magnetic resonance imaging of the subcoracoid region. Orthopedics 1998;21:545-8. 
|
| 34. | Nové-Josserand L, Boulahia A, Levigne C, Noel E, Walch G. Coraco-humeral space and rotator cuff tears. Rev Chir Orthop Reparatrice Appar Mot 1999;85:677-83. 
|
| 35. | Lo IK, Burkhart SS. Arthroscopic coracoplasty through the rotator interval. Arthroscopy 2003;19:667-71. 
|
| 36. | Burkhart SS, Brady PC. Arthroscopic subscapularis repair: Surgical tips and pearls A to Z. Arthroscopy 2006;22:1014-27. 
|
| 37. | Sano H, Ishii H, Yeadon A, Backman DS, Brunet JA, Uhthoff HK. Degeneration at the insertion weakens the tensile strength of the supraspinatus tendon: A comparative mechanical and histologic study of the bone-tendon complex. J Orthop Res 1997;15:719-26. 
|
| 38. | Uhthoff HK, Sano H. Pathology of failure of the rotator cuff tendon. Orthop Clin North Am 1997;28:31-41. 
|
| 39. | Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am 1996;78:1015-23. 
|
| 40. | Bartl C, Imhoff AB. Management of isolated subscapularis tendon tears. Orthopade 2007;36:848-54. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6]
[Table 1], [Table 2], [Table 3], [Table 4]
|
