| |


 |
| Year : 2014 | Volume
: 8
| Issue : 1 | Page : 15-20 |
|
|
|
|
|
ORIGINAL ARTICLE Single-row, double-row, and transosseous equivalent techniques for isolated supraspinatus tendon tears with minimal atrophy: A retrospective comparative outcome and radiographic analysis at minimum 2-year followup
Frank McCormick, Anil Gupta, Ben Bruce, Josh Harris, Geoff Abrams, Hillary Wilson, Kristen Hussey, Brian J Cole
Division of Sports Medicine, Department of Orthopedics, Rush University Medical Center, Chicago, Illinois, USA
Correspondence Address:
Frank McCormick
Rush University Medical Center, 1611 W. Harrison St. Suite 300, Chicago, IL 60612
USA
 Source of Support: None, Conflict of Interest: None  | 9 |
DOI: 10.4103/0973-6042.131850
 |
|
|
|
| Date of Web Publication | 2-May-2014 |
 Abstract Abstract | | |
Purpose: The purpose of this study was to measure and compare the subjective, objective, and radiographic healing outcomes of single-row (SR), double-row (DR), and transosseous equivalent (TOE) suture techniques for arthroscopic rotator cuff repair.
Materials and Methods: A retrospective comparative analysis of arthroscopic rotator cuff repairs by one surgeon from 2004 to 2010 at minimum 2-year followup was performed. Cohorts were matched for age, sex, and tear size. Subjective outcome variables included ASES, Constant, SST, UCLA, and SF-12 scores. Objective outcome variables included strength, active range of motion (ROM). Radiographic healing was assessed by magnetic resonance imaging (MRI). Statistical analysis was performed using analysis of variance (ANOVA), Mann - Whitney and Kruskal - Wallis tests with significance, and the Fisher exact probability test <0.05.
Results: Sixty-three patients completed the study requirements (20 SR, 21 DR, 22 TOE). There was a clinically and statistically significant improvement in outcomes with all repair techniques (ASES mean improvement P = <0.0001). The mean final ASES scores were: SR 83; (SD 21.4); DR 87 (SD 18.2); TOE 87 (SD 13.2); (P = 0.73). There was a statistically significant improvement in strength for each repair technique (P < 0.001). There was no significant difference between techniques across all secondary outcome assessments: ASES improvement, Constant, SST, UCLA, SF-12, ROM, Strength, and MRI re-tear rates. There was a decrease in re-tear rates from single row (22%) to double-row (18%) to transosseous equivalent (11%); however, this difference was not statistically significant (P = 0.6).
Conclusions: Compared to preoperatively, arthroscopic rotator cuff repair, using SR, DR, or TOE techniques, yielded a clinically and statistically significant improvement in subjective and objective outcomes at a minimum 2-year follow-up.
Level of Evidence: Therapeutic level 3.
Keywords: Outcomes, rotator cuff, shoulder, surgical techniques
How to cite this article:
McCormick F, Gupta A, Bruce B, Harris J, Abrams G, Wilson H, Hussey K, Cole BJ. Single-row, double-row, and transosseous equivalent techniques for isolated supraspinatus tendon tears with minimal atrophy: A retrospective comparative outcome and radiographic analysis at minimum 2-year followup. Int J Shoulder Surg 2014;8:15-20 |
How to cite this URL:
McCormick F, Gupta A, Bruce B, Harris J, Abrams G, Wilson H, Hussey K, Cole BJ. Single-row, double-row, and transosseous equivalent techniques for isolated supraspinatus tendon tears with minimal atrophy: A retrospective comparative outcome and radiographic analysis at minimum 2-year followup. Int J Shoulder Surg [serial online] 2014 [cited 2016 Aug 23];8:15-20. Available from: http://www.internationalshoulderjournal.org/text.asp?2014/8/1/15/131850 |
 Introduction Introduction | |  |
Controversy exists regarding the optimal treatment for rotator cuff tears. Over the last decade, some surgeons have promoted a progression from single-row (SR) to double-row (DR) and transosseous equivalent (TOE) techniques. The impetus for this change is to restore the anatomic rotator cuff footprint and maximize the tendon-bone contact area. The development of newer suture anchors has allowed surgeons to efficiently achieve these goals. While biomechanical studies support the evolution of these techniques, clinical data remains inconclusive. [1] Recent studies suggest that footprint restoration via double-row repair may improve re-tear rates; however, this additional footprint restoration may not be cost-effective. [2],[3],[4]
Recent high-level evidence has demonstrated no significant difference in outcomes between the two techniques. For example, arthroscopic single-row and double-row techniques were compared with results showing no clinically significant difference. [5],[6],[7]] Transosseous equivalent studies have shown comparable clinical outcomes. [8] However, there is a paucity of clinical outcome studies comparing the three repair techniques using prospectively collected data. [3] Despite the lack of evidence, the current clinical equipoise is that the arthroscopic transosseous equivalent technique may be clinically superior due to anatomic footprint restoration with the improved tendon-bone contact area.
The purpose of this study was to measure and compare the subjective, objective, and radiographic healing outcomes of single-row (SR), double-row (DR), and transosseous equivalent (TOE) suture techniques for arthroscopic rotator cuff repair. The null hypothesis is that arthroscopic rotator cuff repair will not improve clinical outcome of any cohort undergoing arthroscopic rotator cuff repair. A secondary purpose was to compare the subjective, objective, and radiographic outcomes between surgical repair techniques.
 Materials and Methods Materials and Methods | |  |
Study design
This study represents a retrospective review data from a single surgeon. After Institutional Review Board approval, patient records and surgical reports from July 2000 through July 2010 were reviewed via a query of the electronic billing records using ICD-9 and CPT codes to identify consecutive patients who underwent arthroscopic rotator cuff repair by the senior surgeon. Participants were retrospectively selected into three groups based upon the timeframe of the surgeon's technique progression from single-row to double-row to transosseous equivalent. The operative reports were retrospectively reviewed to confirm the appropriate timeframe of surgery, surgical repair technique performed, and intraoperative findings. A pre-hoc power analysis was performed to determine the cohort sizes and patients were then matched according to age, sex, and tear size. Tear size was determined at the time of surgery and was based upon the maximal medial retraction, with anterior to posterior limited to the supraspinatus. Inclusion criteria consisted of the patient aged 18 or above, primary rotator cuff repair of a single tendon tear, Gouttalier classification of 1 or 2 changes on preoperative magnetic resonance imaging (MRI), failure of conservative treatment of physical therapy, activity modification, and anti-inflammatory medication for a minimum of 6 weeks. Exclusion criteria consisted of revision rotator cuff repair, concomitant anterior instability pathology, subscapularis tears, two or more tendon tears, or concurrent tendon transfers. The primary outcome measure was the American Shoulder and Elbow Society (ASES) score for each technique, measured before and after surgical intervention. Secondary outcomes were the Constant score, SST (Simple Shoulder Test) score, UCLA (University of California at Los Angeles) score, and SF-12 (Short-Form-12) score with an independent physical examination of range of motion via goniometer and isokinetic strength measurement. A blinded, independent observer collected outcome data.
All patients in the double-row and transosseous equivalent cohorts were eligible for a radiographic evaluation of healing using MRI at a minimum of 2 years follow-up. These scores were graded according to the Suguya classification and compared to a previously published surgical cohort of single-row repair performed within the same time period by the senior author. [9] A 3.0 T Hitachi Airis II (Tokyo, Japan) open magnet with a dedicated Hitachi quad coil was used for imaging. Pulse sequences included axial T2 (field of view, 200; repetition time [TR]/time to echo [TE] 4665/125, matrix 192/224; thickness, 4 mm; interval, 5 mm), coronal T1 (field of view, 200; TR/TE 400/20; matrix 180/256; thickness, 4 mm; interval 5, mm), coronal T2 (field of view, 200; TR/TE 4665/125; matrix, 192/224; thickness, 4 mm; interval, 5 mm), coronal IR (field of view, 200; TR/TE 2300/25; matrix 160/256; thickness, 4 mm; interval, 5 mm), sagittal T2 (field of view, 200; TR/TE 4506/125; matrix 192/224; thickness, 4 mm; interval, 5 mm), and sagittal IR (field of view, 200; TR/TE 2300/25; matrix 160/256; thickness, 4 mm; interval, 5 mm). MRIs were evaluated by two orthopedic surgeons (AG, BB) with inter and intraobserver variability measured.
Surgical technique
Patients were prepped and draped in the beach chair position. A standard posterior portal was created, and a 30-degree arthroscope was inserted for visualization. An anterior portal was created under direct visualization with a spinal needle through the rotator interval. A diagnostic glenohumeral arthroscopy was performed. Next, the camera was moved to the subacromial space. A subacromial decompression was performed through a lateral portal using an arthroscopic shaver and radiofrequency device to establish visualization. An anterolateral high accessory portal was then established for suture management and anchor placement. Tissue mobilization and releases were performed to obtain a tension-free restoration of the anatomic footprint. The cortical surface of the rotator cuff tear insertion was lightly decorticated to achieve punctate bleeding. The surgical repair technique was determined by the senior surgeon, and based on time wise technique progression with first generation techniques being applied to the initial cohort, second generation double row techniques to the second cohort, and transosseous equivalent techniques applied to the third cohort [Figure 1]. In all cases, suture was passed through the tendon using a spectrum suture passer (Conmed-Linvatec Utica, NY). In general, single row repairs were performed with two double-loaded 5-mm suture anchors (Corkscrew, Arthrex, Naples, FL) inserted just in the lateral aspect of the prepared footprint separated by 1 cm. Horizontal mattress suture configuration was performed for each suture: The sutures spanned the anterior to posterior tear length and were placed approximately one cm proximal to the tendon tear. The tendon was repaired to bone using established knot-tying principles (alternating half-hitches over alternating suture posts). A double-row repair consisted of the same anchor placement in the medial row placed at the articular margin with an additional two similar suture anchors placed laterally at the medial edge of the greater tuberosity to secure the distal tendon to the prepared footprint. The transosseous equivalent technique was performed utilizing a similar medial row configuration. Lateral fixation was achieved with two 4.5 mm Pushlock (Arthrex, Naples, FL) anchors. One limb from each anchor was brought over the top of the repair and secured to the greater tuberosity with the knotless anchor placed 1 cm lateral to the medial row and 1 cm from the other lateral row anchor. One limb from the second and fourth knots was similarly secured in line with, but 1 cm posterior to the first lateral anchor. Sutures were tensioned under direct visualization before lateral anchor insertion. All suture ends were cut and the repair probed for security. Additional pathology identified during diagnostic arthroscopy was addressed at the time of surgery.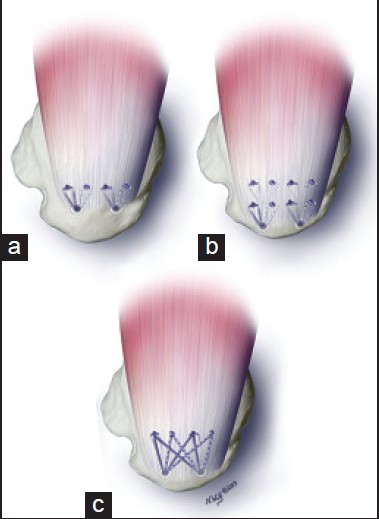 | Figure 1: Three-dimensional arthroscopic supraspinatus rotator cuff repair technique illustration (a) Single-row is performed by a single row of two double loaded suture anchors in a horizontal-mattress suture confi guration (b) A double row is performed by a medial and lateral row of two double loaded suture anchors in a horizontal-mattress suture confi guration (c) A transosseous repair technique is performed in the same way as a single row, in addition, one limb from each anchor was brought over the top of the repair and secured to the greater tuberosity with the knotless anchor placed one cm lateral to the medial row and one centimeter from the other lateral row anchor. One limb from the second and fourth knots was similarly secured in line with, but one centimeter posterior to the fi rst lateral anchor
Click here to view |
Postoperative protocol
All patients were treated with the same rotator cuff progressive phases and closely monitored protocol consisting of three progressive phases: Phase 1- sling and passive range of motion for the first 4-6 weeks inclusive of closed chain scapulothoracic and nonrotator cuff activities; phase 2-active range of motion until full range of motion obtained; phase 3-progressive scapulothoracic and rotator cuff strengthening at 12-16 weeks.
Statistical analysis
All demographic and outcome data were analyzed descriptively. An a priori power analysis was performed based upon an expected 6.4 point minimally clinically significant ASES improvement with a standard deviation of 10, which identified that a total of 18 patients needed to be enrolled in each arm for a sufficient power (beta = 0.2). [10] ANOVA was used to compare the demographic and independent variables between study groups and between respondents and nonrespondents. A Mann - Whitney U test was used to compare the prospective ASES outcomes as the primary objective for each technique; a Kruskal - Wallis test was performed between technique cohorts to evaluate for differences between techniques. A Freeman - Halton extension of the Fisher exact probability test was performed for the MRI re-tear rate analysis. A Pearson Coefficient was tested for the interobserver reliability of tear assessment. Results were considered significant at P<x = 0.05. All statistics were performed using SPSS 16.0 (SPSS Inc., Chicago, IL).
 Results Results | |  |
Sixty-three patients completed the study requirements (20 SR, 21 DR, 22 TOE) at a mean followup of 4.0 years (range 2-7.5 years). Fifty percent of eligible patients completed the study requirements [Figure 2]. Cohort's demographic data are listed in [Table 1]. There was no statistically significant demographic differences between technique cohorts' ages at surgery (mean 62 years; range 34-81), sex (54% male), and rotator cuff tear size (mean 2.75 cm; range 0-5). There was a trend toward larger tears in the technique progression, with the larger tears treated with a transosseous equivalent technique. The mean cohort date of surgery was statistically different, with the TOE repairs performed nearly 2 years after. Single-row repair techniques were from the earliest period in the study and had a longer follow-up duration, which was statistically significant but not considered clinically significant.
Each repair technique had a clinically and statistically significant positive response to surgery based on the prospectively collected ASES outcome (P < 0.001 for all groups) [Figure 3]. The double-row repair technique had the highest mean improvement of 22.3 ASES points over the study period; however, this was not significantly better than the TOE (mean improvement = 18.7,) nor the SR (mean improvement = 17.5) (P = 0.94) [Figure 3]. There was a statistically significant improvement in supraspinatus strength for each repair technique (P < 0.001). There was a trend toward improved range of motion in the supraspinatus plane for each technique (P = 0.01) [Table 2].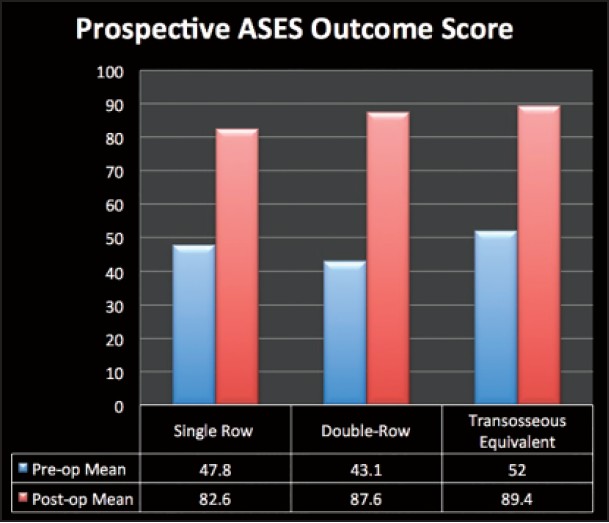 | Figure 3: Using the ASES outcome score as the primary outcome, each technique provided a statistically and clinically signifi cant improvement in outcome over the study period. However, we did not demonstrate a difference between repair techniques
Click here to view |
Comparing final outcomes between techniques, we found, no clinical or statistically significant difference in the mean final follow-up ASES (P = 0.73), constant (P = 0.56), SST (P = 0.55), UCLA (P = 0.46), SF-12 physical (P = 0.65), SF-12 mental (P = 0.38). ROM forward flexion (P = 0.55) and strength forward flexion (P = 0.25)/ER (P = 0.92) was observed [Table 3].
Over 80% of patients completed an MRI evaluation at final followup to evaluate the rotator cuff integrity. There was a progressive decrease in re-tear rates from single row (22% 11/49), based a previously published study by the senior surgeon, to double-row (18% 3/17) to transosseous equivalent (11% 2/19); however, this difference was not statistically significant (P = 0.6). There was a strongly positive interobserver correlation between surgeons (0.82) and intraobserver correlation of (0.80) at 2 weeks.
 Discussion Discussion | |  |
The purpose of this study was to quantify the improvement via validated outcomes of single-row, double-row suture and transosseous equivalent techniques for repair of the rotator cuff with a minimum two-year follow-up with a single surgeon whose techniques evolved over time for the same tear pattern. This retrospective comparative investigation of three different arthroscopic rotator cuff repair techniques has demonstrated a clinically and statistically significant improvement for patients undergoing arthroscopic rotator cuff repair of a single supraspinatus tendon tear with good biology as determined by MRI grading utilizing any of the three techniques based on the primary outcome of the prospectively-collected ASES scores. As an adjunct, this conclusion is supported by statistically significant mean improvements in the Constant SST outcome scores, forward flexion strength improvement, with an improvement trend of floward flexion range of motion. From an individual group standpoint, this trend resembles previously published data. [5],[11],[12],[13] In comparing the primary and secondary outcome measures, we found no difference between groups. However, a post-hoc analysis demonstrated our analysis to have insufficient power to accept our secondary null hypothesis for the ASES outcome measure. Future work will require a large study of approximately 660 patients to provide sufficient power to analyze the difference between ASES outcomes scores for the three current arthroscopic repair techniques.
Within our follow-up period, the vast majority of patients obtained good to excellent outcomes based on all of our measures, making for a ceiling effect. Future studies may have to extend the following up period, apply more sensitive outcome tools, or expand the subjects analyzed to detect a significant difference between outcomes. To date, there is no comparative study comparing the clinical results of single row versus double row versus TOE techniques for primary repair of rotator cuff tears.Therefore, this study provides clinically relevant information pertaining to three current arthroscopic techniques performed by a single surgeon. The results of this study demonstrate a benefit with all three techniques.
The goal of arthroscopic rotator cuff repair is to improve pain and function in symptomatic patients.Therefore, the goal of surgery is to provide stable fixation, minimize gap formation, and maximize tendon-to-bone healing.Controversy exists as to the ideal repair technique for rotator cuff tears, but literature supports improved outcomes in patients with healed rotator cuffs. [14],[15],[16],[17] Good to excellent clinical results have been reported with single-row, double-row, transosseous, and transosseous-equivalent suture techniques.
The most common arthroscopic repair method is via single- or double-row techniques.Single-row repairs have demonstrated improved clinical outcomes compared to preoperative baseline function. [18] Double-row techniques evolved in an attempt to improve overall healing rates by increasing construct stiffness, contact pressure, and initial fixation strength as demonstrated in in-vitro biomechanical models. [19] Despite increased strength, double-row techniques have not demonstrated significant differences in clinical outcome compared to single-row techniques for small to large full-thickness rotator cuff tears.In a recent randomized controlled trial comparing single-and double-row fixation, despite improved healing rates on postoperative ultrasound or MRI, there was no overall difference in function or quality of life outcomes at minimum two-year follow-up. [5] Transosseous-equivalent repair techniques have demonstrated improved outcomes.Such techniques lead to greater contact area and pressure over the native cuff footprint than single or double-row suture and equivalent to traditional transosseous techniques. [20],[21] Early results have demonstrated improved clinical and radiographic healing at short-term follow-up. [11]
Similar to the current study, in a recent level one evidence randomized controlled trial comparing single- versus double -row rotator cuff repairs for medium to large rotator cuff tears at two-year follow up, there was a significant improvement in ASES, UCLA, and Constant Score for both groups but no significant difference between groups with cuff tears between 10 to 30-mm in size.For larger sized tears, however, the ASES and UCLA scores were significantly higher for the double-row group. [12] Similarly, in another recent randomized controlled trial evaluating single versus double-row rotator cuff repair outcomes with two-year follow-up, there was a significant improvement in ASES index, UCLA score, and shoulder strength in both groups but no significant differences between groups for cuff tears less than 30-mm in size.For tears greater than 30-mm, there was a significant difference in strength with the double-row group demonstrating a greater improvement versus single row. [13] Pennington et al. (2010) demonstrated improved healing rates for double row repairs compared with single row technique in similarly sized tears. [22] In a recent systematic review evaluating prospective level one and two evidence comparing single versus double-row repair, there was no significant difference in functional ASES or Constant scores between groups.There was a trend toward a higher re-tear rate in the single-row group, but this was not significant. [23]
While the literature has not identified a clinically significant difference in outcome between repair techniques at early and mid-term follow-up, some suggest that radiographic evidence of healing rates within this follow-up period would predict maintenance of long-term function. Thus, there is an emphasis on re-tear rates amongst techniques. While we found an improved re-tear rate based on technique progression, this difference was not statistically significant. This is in accordance with Mihataet al. [3] finding a superior re-tear rate with the TOE technique (4.7%) as compared to the single row (10.8%) and double-row (26.1%) [3] However, other studies have shown comparable rates between the double-row (24%) to the TOE (20%) [8] The finding of lower re-tear rates without with lateral anchor placement is supported by two recent systematic reviews. [2],[6] Whether this translates to improved outcomes over a longer period will need further study.
There are several limitations to this study.This study was not powered to detect a difference between groups.Post-hoc power analysis demonstrated 660 patients would be required for adequate power, indicating the need for a meta-analysis or multi-center study. Smaller tears, which may be more likely to heal, may not have been felt to require double row fixation.Alternatively, a patient with a retracted tear with minimal excursion may have been amenable to single row repair only, to avoid complications associated with over tensioning the native cuff. Additionally, lack of subject and surgeon blinding may have led to performance bias. Moreover, the improvement in retear rates may be a manifestation of the surgeon's learning curve and tear pattern recognition. While the major determinant of surgical technique as the timewiseprogession of surgical technique, there was no randomization which introduces a selection bias for the surgeon based on his intra-operative decision making. The large variability for rotator cuff size tear inclusion may also introduce a performance bias.The mean followup time for the single row was greater than the other two groups.Arthroscopically-repaired rotator cuffs have been shown to increase their healing rates over time. [24] This may introduce a time bias into the current study as more single-row repairs were performed early in the study period. The increased re-tear rate analyzed in our study is from another cohort so a direct comparison between the single row outcomes and retear rates cannot be performed.There was a trend toward larger tears in the TOE cohort which introduces a performance bias and selection bias. The orthopedic surgeons grading the MRI were not independent, nor blinded, and were compared to a separate historical group of single rows. Lastly, the study authors were unable to achieve 80% follow-up on all patients, rendering the possibility of transfer bias. Financial limitations precluded more imaging analysis.
 Conclusions Conclusions | |  |
Compared to pre-operatively, arthroscopic rotator cuff repair, using SR, DR, or TOE techniques, yielded a clinically and statistically significant improvement in subjective and objective outcomes at a minimum two-year follow-up.
 References References | |  |
| 1. | Wall LB, Keener JD, Brophy RH. Double-row vs single-row rotator cuff repair: A review of the biomechanical evidence. J Shoulder Elbow Surg 2009;18:933-41. 
|
| 2. | Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med 2010;38:835-41. 
|
| 3. | Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, et al. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med 2011;39:2091-8. 
|
| 4. | Genuario JW, Donegan RP, Hamman D, Bell JE, Boublik M, Schlegel T, et al. The cost-effectiveness of single-row compared with double-row arthroscopic rotator cuff repair. J Bone Joint Surg Am 2012;94:1369-77. 
|
| 5. | Lapner PL, Sabri E, Rakhra K, McRae S, Leiter J, Bell K, et al. A multicenter randomized controlled trial comparing single-row and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am 2012;94:1249-57. 
|
| 6. | DeHaan AM, Axelrad TW, Kaye E, Silvestri L, Puskas B, Foster TE. Does double-row rotator cuff repair improve functional outcome of patients compared with single-row technique? A systematic review. Am J Sports med 2012;40:1176-85. 
|
| 7. | Saridakis P, Jones G. Outcomes of single-row and double-row arthroscopic rotator cuff repair: A systematic review. J Bone Joint Surg Am 2010;92:732-42. 
|
| 8. | Kim KC, Shin HD, Lee WY, Han SC. Repair integrity and functional outcome after arthroscopic rotator cuff repair: Double-row versus suture-bridge technique. Am J Sports Med 2012;40:294-9. 
|
| 9. | Cole BJ, McCarty LP, Kang RW, Alford W, Lewis PB, Hayden JK. Arthroscopic rotator cuff repair: prospective functional outcome and repair integrity at minimum 2-year follow-up. J Shoulder Elbow Surg 2007;16:579-85. 
|
| 10. | Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: A systematic review of four questionnaires. Arthritis Rheum 2009;61:623-32. 
|
| 11. | Toussaint B, Schnaser E, Bosley J, Lefebvre Y, Gobezie R. Early structural and functional outcomes for arthroscopic double-row transosseous-equivalent rotator cuff repair. Am J Sports Med 2011;39:1217-25. 
|
| 12. | Carbonel I, Martinez AA, Calvo A, Ripalda J, Herrera A. Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: A prospective randomized clinical study. IntOrthop 2012;36:1877-83. 
|
| 13. | Ma HL, Chiang ER, Wu HT, Hung SC, Wang ST, Liu CL, et al. Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: A prospective randomized trial. Arthroscopy 2012;28:16-24. 
|
| 14. | Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: A prospective study. J Shoulder Elbow Surg 2006;15:290-9. 
|
| 15. | Cole BJ, Rodeo SA, O'Brien SJ, et al. The anatomy and histology of the rotator interval capsule of the shoulder. Clinical orthopaedics and related research 2001:129-37. 
|
| 16. | Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with the use of the double-row suture anchor technique. J Bone Joint Surg Am 2007;89:1533-41. 
|
| 17. | Huijsmans PE, Pritchard MP, Berghs BM, van Rooyen KS, Wallace AL, de Beer JF. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am 2007;89:1248-57. 
|
| 18. | Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am 1998;80:832-40. 
|
| 19. | Kim DH, Elattrache NS, Tibone JE, Jun BJ, DeLaMora SN, Kvitne RS, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med 2006;34:407-14. 
|
| 20. | Park MC, Idiadi JA, Elattrache NS, Tibone JE, McGarry MH, Lee TQ. The effect of dynamic external rotation comparing 2 footprint-restoring rotator cuff repair techniques. Am J Sports Med 2008;36:893-900. 
|
| 21. | Behrens SB, Bruce B, Zonno AJ, Paller D, Green A. Initial fixation strength of transosseous-equivalent suture bridge rotator cuff repair is comparable with transossseous repair. Am J Sports Med 2012;40:133-40. 
|
| 22. | Pennington WT, Gibbons DJ, Bartz BA, Dodd M, Daun J, Klinger J, et al. Comparative analysis of single-row versus double-row repair of rotator cuff tears. Arthroscopy 2010;26:1419-26. 
|
| 23. | DeHaan Am, Axelrad TW, Kaye E, Silvestri L, Puskas B, Foster TE. Does double-row rotator cuff repair improve functional outcome of patients compared with single-row technique? A systematic review. Am J Sports Med 2012;40:1176-85. 
|
| 24. | Nho SJ, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: Subgroup analysis. J Shoulder Elbow Surg 2009;18:697-704. 
|
[Figure 1], [Figure 2], [Figure 3]
[Table 1], [Table 2], [Table 3]
| This article has been cited by | | 1 |
Single-row arthroscopic cuff repair with double-loaded anchors provides good shoulder function in long-term follow-up |
|
| Mladen Miškulin,Goran Vrgoc,Goran Sporiš,Oliver Dulic,Gordan Gavrilovic,Zoran Milanovic | | International Orthopaedics. 2014; | | [Pubmed] | [DOI] | |
|
 |
|
