| |


 |
| Year : 2014 | Volume
: 8
| Issue : 2 | Page : 51-54 |
|
|
|
|
|
CASE REPORT Sudden severe postoperative dyspnea following shoulder surgery: Remember inadvertent phrenic nerve block due to interscalene brachial plexus block
Arpit Jariwala1, Pavan Kumar B. C. Raju2, David M Coventry2
1 Department of Orthopaedics, Ninewells Hospital and Medical School, Dundee DD1 9SY, United Kingdom
2 Department of Anaesthesia, Ninewells Hospital and Medical School, Dundee DD1 9SY, United Kingdom
Correspondence Address:
Arpit Jariwala
Department of Orthopaedics, Ninewells Hospital and Medical School, Dundee DD1 9SY
United Kingdom
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.137528
 |
|
|
|
| Date of Web Publication | 24-Jul-2014 |
 Abstract Abstract | | |
Advanced imaging techniques, improved operative techniques, and instrumentation combined with better patient awareness and expectations have resulted in an exponential increase in upper limb surgical procedures during recent times. Surgical teams expect superior analgesia and regional blocks have matched these expectations quite often resulting in improved patient satisfaction and early rehabilitation to achieve best results. Ultrasound-guided interscalene brachial plexus block (ISB) is commonly used to provide analgesia for procedures involving shoulder girdle. We report a case of symptomatic hemi-diaphragmatic paresis (HDP) due to the phrenic nerve block following ISB for arthroscopic sub-acromial decompression of the shoulder presenting as severe postoperative dyspnea. There is strong evidence of HDP following ISB in anesthetic literature, but not reported in related surgical specialties such as orthopedics. We wish to inform upper-limb surgeons and educate junior doctors and other ancillary staff working in upper-limb units to be aware of this serious but reversible complication.
Keywords: Acute postoperative dyspnea, hemi-diaphragmatic paresis, interscalene brachial plexus block, phrenic nerve block
How to cite this article:
Jariwala A, Raju PB, Coventry DM. Sudden severe postoperative dyspnea following shoulder surgery: Remember inadvertent phrenic nerve block due to interscalene brachial plexus block. Int J Shoulder Surg 2014;8:51-4 |
How to cite this URL:
Jariwala A, Raju PB, Coventry DM. Sudden severe postoperative dyspnea following shoulder surgery: Remember inadvertent phrenic nerve block due to interscalene brachial plexus block. Int J Shoulder Surg [serial online] 2014 [cited 2016 Aug 23];8:51-4. Available from: http://www.internationalshoulderjournal.org/text.asp?2014/8/2/51/137528 |
 Introduction Introduction | |  |
Shoulder disorders are frequently presented in general practice with up to 20% of the adult population experiencing problems with their shoulder at some time. [1] High-resolution magnetic resonance scanners and improved arthroscopic techniques have led to an exponential increase in surgical procedures undertaken for impingement, cuff tears, instability and arthritis of the shoulder. Surgical teams are investigating for superior quality pain relief to aid early initiation of the rehabilitation protocols to achieve best possible outcome. Peripheral nerve blocks have the ability to provide such good quality analgesia for both arthroscopic and open procedures on the shoulder girdle. Peripheral nerve blocks provide better quality of analgesia, reduce supplemental opioid requirement, both during intraoperative and postoperative period, and the associated side-effects and lead to an improved patient satisfaction. [2] The interscalene brachial plexus block (ISB) is the most common method used for analgesia for shoulder procedures. [2] ISB aims to block the brachial plexus at the level of nerve roots or trunks, thus being ideal for procedures around the shoulder joint, lateral two-thirds of the clavicle and proximal humerus. Ultrasound guided ISB is extremely safe and there is growing evidence to suggest its better safety profile and efficacy. However, the rare complications, although reduced in incidence, are not completely eliminated.
We describe a case of symptomatic hemi-diaphragmatic paresis (HDP) due to phrenic nerve blockade following ISB for arthroscopic sub-acromial decompression of the shoulder presenting as severe postoperative dyspnea.
 Case report Case report | |  |
A 73-year-old woman was scheduled for arthroscopic sub-acromial decompression of the right shoulder. She had a history of well-controlled hypertension and had undergone mastectomy for breast cancer many years previously, but had remained otherwise healthy, having never smoked and with a good exercise tolerance. She had a body mass index of 30. During preoperative assessment, she reported an extremely unpleasant experience due to pain after mastectomy previously and this made her very apprehensive with respect to postoperative pain after the current procedure. After discussion, she opted to have a combination of regional anesthesia in the form of ISB and general anesthesia.
Ultrasound guided ISB was performed using a Zonare z.one ultrasound machine and a 5-10 MHz linear probe. An in-plane technique was employed successfully to block the C5 and C6 nerve roots with 10 ml of 0.2% ropivacaine under the direct supervision, without any immediate complications. General anesthesia was then uneventfully induced.
Arthroscopic sub-acromial decompression was carried out in the "deck-chair" position. Standard sub-acromial decompression was carried out using cutting block technique. Good clearance was obtained and no further procedures were required. Surgery took a total of 35 min during which a standard general anesthesia was maintained. No adverse events or complications were noted on completing the procedure. After an uneventful time in recovery, she was transferred to the ward for further postoperative management.
90 min following the procedure, in the ward, she was changed from semi-recumbent to supine position. This triggered her complaint of sudden onset of shortness of breath and inability to speak. She was immediately seated upright and high-flow oxygen was administered via a nonrebreathing mask. Once she resumed sitting position, the symptoms of shortness of breath and inability to speak improved very quickly. She was continuously monitored for oxygen saturation, blood pressure, heart rate, temperature, and GCS and they were within the normal limits. Chest auscultation revealed decreased air entry at the right base.
Bedside chest radiograph was organized to rule out any serious complication due to ISB such as pneumothorax. Interestingly, it revealed an elevated hemi-diaphragm, a classical picture of HDP occurring due to the phrenic nerve block caused by ISB [Figure 1].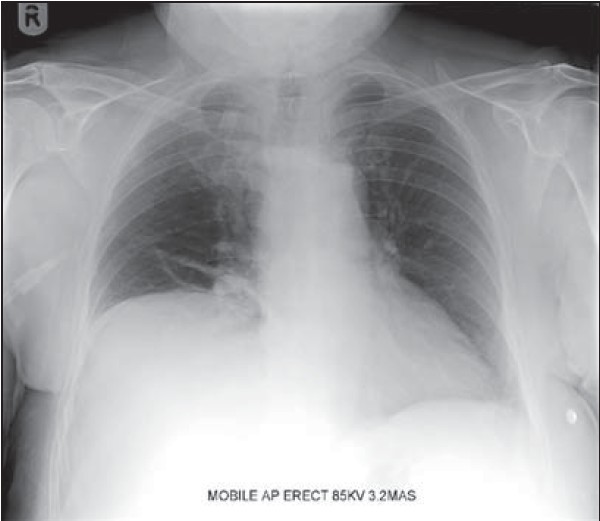 | Figure 1: Radiograph of the patient with elevation of the right hemidiaphragm indicating right side phrenic nerve paresis
Click here to view |
Reassurance was given to the patient and was monitored closely in a semi-recumbent position. Dyspnea never recurred and she remained comfortable and stable during the remainder of the postoperative period. No further complications occurred and she was discharged home the following day.
The patient was reviewed 2 weeks following initial discharge due to the untoward event occurring during the immediate postoperative period. The event was discussed again in detail with the patient and a satisfactory explanation was given. She informed the surgical team that she had no further similar episodes and was functioning well in her daily activities. Her shoulder pain had improved and she was able to move her right shoulder better when compared to before surgery. She was referred for physiotherapy for her shoulder with a review appointment after 6 weeks.
 Discussion Discussion | |  |
Hemi-diaphragmatic paresis due to ISB is well-documented in the anesthetic literature, but interestingly there is no information in the mainstream orthopedic literature. Hence, we wish to highlight this potential complication due to ISB among upper limb surgeons and educate junior doctors and other ancillary staff working in upper limb units to be aware of this complication.
Interscalene brachial plexus block is increasingly used for site specific anesthesia and analgesia for shoulder surgery. It offers excellent intraoperative and postoperative pain relief, reduced supplementary opioid requirement and possibility of early discharge and initiation of rehabilitation. The aim of ISB is to selectively block C5-6 roots or upper trunk of brachial plexus to provide analgesia for shoulder surgery. In the past decade, ultrasound has demonstrated the potential to become the gold standard for nerve localization while performing ISB although it has not quite achieved the status. [3] It allows direct visualization of the nerves and the surrounding structures and helps in correct placement of the needle and local anesthetic, thus reducing the inadvertent serious complications such as neurovascular injuries.
Phrenic nerve (C 2, 3, 4 ) has its origin close to the brachial plexus nerve roots [4] and is separated by a thin fascia. Inadvertent puncture of this fascia or spread of local anesthetic solution around the nerve may lead to unintended ipsilateral phrenic nerve paresis. Use of ultrasound has led to use of low volumes of local anesthetic and hence, has reduced the incidence of HDP due to phrenic nerve blockade. [5],[6] The choice dose of 0.2% ropivacaine in our practice is based on the local audit results. [7] However, McCartney and Patel's recent editorial gives a scientific explanation behind achieving an ideal balance between onset, efficacy, and duration of peripheral nerve block techniques while reducing adverse effects to the lowest level possible. [8] Hence, a cautious approach needs to be employed, while using very low volumes of local anesthetic without compromising on the duration of the block, although further studies are required to determine the optimal dose for a block. Patients with conditions where they cannot withstand a 25% decrease in pulmonary function such as chronic obstructive pulmonary disease, morbid obesity, and severe asthma are more prone to developing dyspnea following HDP.
It is also important to note that asymptomatic HDP occurs almost always with ISB in a significant proportion of patients with some series reporting the incidence to be anything up to 100%. [9] It remains more commonly asymptomatic as patients with no compromise in pulmonary function compensate well for the decrease in pulmonary function. The present case reports the occurrence of symptomatic hemi-diaphragmatic phrenic nerve palsy in a previously fit patient even when using low dose of local anesthetic under ultrasound-guidance for ISB.
In the majority of reported cases, respiratory distress presented reasonably soon after the insertion of ISB. [10] However, in the present case, there was a symptom free period of approximately 90 min before respiratory distress developed. The most probable reason for the delay is the absence of a triggering factor and in this case, it was change in patient's position. Until the change in position, the patient was nursed in semi-recumbent position. The pulmonary function was already compromised by ipsilateral HDP, but was well compensated. The symptoms appeared when it was further compromised by supine position. Furthermore, improvement in her symptoms once she was seated upright explains the degree of pulmonary function that worsened with supine position. Although, patient did not have any previous respiratory ailments, we acknowledge that the age of this patient may have been a contributing factor for the compromise in ventilation. HDP usually lasts until the effect of block persists and disappears once the local anesthetic effect wears off along with the analgesic effect of the block. It can become symptomatic when there is a further compromise in the pulmonary function. This highlights the importance of close monitoring and supplemental oxygenation. The majority of patients recover completely although there are occasional reports of continued dysphonic symptoms over a prolonged period. [11] Our patient did not experience similar symptoms again in the postoperative period and had recovered well at the time of discharge. She was having an uneventful recovery at 2 weeks during her first follow-up.
The incidence of HDP is very high with traditional ISBs regardless of the approach and the method used to detect the plexus. [9] Asymptomatic HDP is regarded by some anesthetists as a side-effect of ISB instead of a complication with majority of patients developing it. [12] However, there should be a high index of suspicion of HDP when a patient develops respiratory distress following ISB in the immediate postoperative period and this can be easily confirmed by a chest radiograph revealing elevated diaphragm on one side.
 Conclusion Conclusion | |  |
We wish to inform doctors involved in the care of patients undergoing ISB for upper limb surgery by highlighting the present case report regarding HDP due to phrenic nerve block, a potentially reversible and easily identifiable complication. We advise to add it to any lists of postoperative conditions presenting with sudden onset dyspnea including potential life-threatening complications such as pneumothorax, acute coronary event, or rarely pulmonary embolism. In addition, we strongly recommend cautious and close postoperative monitoring with a high index of suspicion for phrenic nerve block induced hemi-diaphragmatic paresis following ISBs and patient should be nursed in a semi-recumbent position until the effect of the block wears off.
 References References | |  |
| 1. | Hasvold T, Johnsen R. Headache and neck or shoulder pain - Frequent and disabling complaints in the general population. Scand J Prim Health Care 1993;11:219-24. 
|
| 2. | Bowens C Jr, Sripada R. Regional blockade of the shoulder: Approaches and outcomes. Anesthesiol Res Pract 2012;2012:971963. 
|
| 3. | Marhofer P, Harrop-Griffiths W, Kettner SC, Kirchmair L. Fifteen years of ultrasound guidance in regional anaesthesia: Part 1. Br J Anaesth 2010;104:538-46. 
|
| 4. | Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: Implications for the interscalene brachial plexus block. Reg Anesth Pain Med 2008;33:545-50. 
|
| 5. | Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med 2009;34:498-502. 
|
| 6. | Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth 2008;101:549-56. 
|
| 7. | Satapathy A, Munirama S, Coventry D. A prospective audit of the analgesic efficacy and duration of action of a 20 mg bolus of ropivacaine for interscalene brachial plexus block following shoulder surgery. Anaesthesia 2012;67:s1:23. 
|
| 8. | McCartney CJ, Patel S. Local anesthetic volume for peripheral nerve blocks: How low can (or should) we go? Reg Anesth Pain Med 2012;37:239-41. 
|
| 9. | Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg 1991;72:498-503. 
|
| 10. | Chaudhuri S, Gopalkrishna M, Paul C, Kundu R. Can bilateral bronchospasm be a sign of unilateral phrenic nerve palsy after supraclavicular brachial plexus block? J Anaesthesiol Clin Pharmacol 2012;28:249-51. 
[PUBMED]  |
| 11. | Ediale KR, Myung CR, Neuman GG. Prolonged hemidiaphragmatic paralysis following interscalene brachial plexus block. J Clin Anesth 2004;16:573-5. 
|
| 12. | Neal JM, Hebl JR, Gerancher JC, Hogan QH. Brachial plexus anesthesia: Essentials of our current understanding. Reg Anesth Pain Med 2002;27:402-28. 
|
[Figure 1]
|
