| |


 |
| Year : 2014 | Volume
: 8
| Issue : 4 | Page : 95-100 |
|
|
|
|
|
ORIGINAL ARTICLE Age-related joint space narrowing independent of the development of osteoarthritis of the shoulder
Jörn Kircher1, Konstanze Kuerner2, Markus Morhard3, Rüdiger Krauspe2, Peter Habermeyer3
1 Department of Orthopaedics, Shoulder and Elbow Surgery, Klinik Fleetinsel, Admiralitätstrasse 3-4, 20489 Hamburg; Department of Orthopaedics, Medical Faculty, Heinrich-Heine-University, Moorenstrasse 5, 40225 Düsseldorf; Department of Shoulder and Elbow Surgery, ATOS Clinic, Bismarckstrasse 9-15, 69115 Heidelberg, German, Germany
2 Department of Orthopaedics, Medical Faculty, Heinrich-Heine-University, Moorenstrasse 5, 40225 Düsseldorf, Germany
3 Department of Shoulder and Elbow Surgery, ATOS Clinic, Bismarckstrasse 9-15, 69115 Heidelberg, German, Germany
Correspondence Address:
Jörn Kircher
Shoulder and Elbow Surgery, Klinik Fleetinsel, Admiralitätstrasse 3-420489, Hamburg, German state
Germany
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.145213

|
|
|
|
| Date of Web Publication | 21-Nov-2014 |
 Abstract Abstract | | |
Purpose: It is commonly accepted that the glenohumeral joint space remains unchanged until the onset of osteoarthritis, at which point progressive degenerative changes, and joint space narrowing occur. The aim of this study was to evaluate the radiographic width of the glenohumeral joint space in patients of different ages: Those with otherwise normal radiographs, those with a history of instability, those with calcific tendonitis, and those with a radiologic diagnosis of osteoarthritis.
Materials and Methods: In this retrospective study, two independent investigators measured the glenohumeral joint width on true anteroposterior and axillary views of standardized shoulder radiographs taken from 2002 to 2009. The digital image resolution was 0.01 mm. Group I comprised 60 patients with normal shoulder radiographs, Group II comprised 53 patients with instability but normal radiographs, Group III comprised 109 patients with radiologically proven calcific tendonitis, and Group IV comprised 120 patients with manifest osteoarthritis.
Results: The interobserver reliability (r) was 0.621-0.862. The mean joint space width was significantly different among Groups I-IV (central anteroposterior: 4.28 ± 0.75 mm, 3.12 ± 0.73 mm, 2.87 ± 0.80 mm, and 1.47 ± 1.07 mm, respectively; P = 0.001; central axillary: 6.12 ± 1.09 mm, 3.92 ± 0.77 mm, 3.34 ± 0.84 mm, and 1.08 ± 1.12 mm, respectively; P = 0.001). There was a significant negative correlation between the joint space width and age at all measured levels in both projections (P < 0.001).
Conclusions: The glenohumeral joint space width decreases with increasing age beginning in early adulthood, and this effect is enhanced by osteoarthritis.
Level of Evidence: Level II, retrospective study.
Keywords: Aging, cartilage, joint space, osteoarthritis, radiograph, shoulder
How to cite this article:
Kircher J, Kuerner K, Morhard M, Krauspe R, Habermeyer P. Age-related joint space narrowing independent of the development of osteoarthritis of the shoulder. Int J Shoulder Surg 2014;8:95-100 |
 Introduction Introduction | |  |
Osteoarthritis of the shoulder is a common disease and its incidence increases with age. The underlying cause of primary osteoarthritis of the shoulder is unknown. [1],[2] Genetic factors and connective tissue properties have recently become the focus of basic research. [3],[4],[5],[6],[7],[8],[9],[10]
It is commonly accepted that the glenohumeral joint space remains unchanged until the onset of osteoarthritis, at which point progressive degenerative changes, and joint space narrowing occur. [11],[12],[13] The available data on the cartilage thickness of the glenohumeral joint and the radiologically normal joint space are sparse. [11],[12],[13],[14] Alteration of all aspects of the articular cartilage (matrix and chondrocytes) was recently shown to be a continuous age-related process beginning in the early years. [10]
The aim of this study was to evaluate the radiological width of the glenohumeral joint space in patients with normal radiographs and compare these findings with those of patients with other radiologic findings of osteoarthritis, such as caudal osteophytes. We also investigated the influence of aging on the development of glenohumeral joint space narrowing.
 Materials and methods Materials and methods | |  |
We performed a retrospective analysis of standardized shoulder radiographs, including true anteroposterior and axillary projections, at our institutions from 2002 to 2009. The glenohumeral joint space was measured using digital images with a resolution of 0.01 mm at the superior, central, and inferior levels of the anteroposterior view [Figure 1]a and the anterior, central, and posterior levels of the axillary view [Figure 1]b (SIENET Magic View 100; Siemens, Erlangen, Germany). The measurements were made perpendicular to the tangent to the humeral joint surface at each level using the digital measurement tool at the highest available magnification of the screen. The measurements were performed by two independent investigators (first and second authors).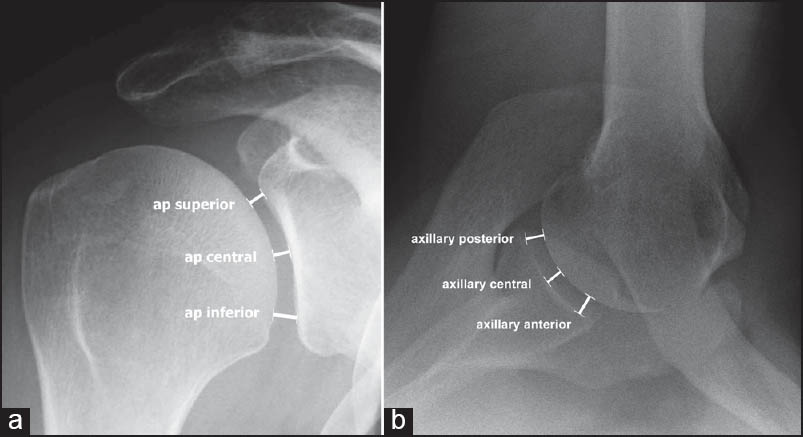 | Figure 1: True (a) anteroposterior and (b) axillary view radiographs of the right shoulder illustrating the levels of joint space width measurement: Superior, central, and inferior anteroposterior in the coronal plane and anterior, central, and posterior axillary in the transverse plane. Measurements were made perpendicular to the articular surface
Click here to view |
We investigated four groups of patients: Group I, 60 patients in early adulthood (14-21 years of age) with normal shoulder radiographs; Group II, 53 patients (16-70 years of age) with instability according to the clinical history, but normal radiographs; Group III, 109 patients (29-69 years of age) with radiographically diagnosed calcific tendonitis; and Group IV, 120 patients (36-86 years of age) with clinical and radiographic evidence of osteoarthritis. The inclusion criteria were as follows. Group I: Early adulthood, closed growth plates, and radiographic absence of bone or joint pathology due to causes other than trauma; Group II: Shoulder instability with no more than two dislocations overall no longer than 2 months ago, absence of bony injury, no previous surgery, and normal shoulder radiographs; Group III: Radiologic presence of calcific tendonitis of the supraspinatus tendon, no history of trauma or instability, no previous surgery, and intact rotator cuff proven by ultrasound; and Group IV: Primary osteoarthritis of the shoulder, intact rotator cuff proven by ultrasound, no history of trauma, no previous surgery, and no glenoid erosion or protrusion.
Because there is no accepted association of calcific tendonitis of the shoulder or instability at an early stage with the presence of osteoarthritis, Groups I, II, and III served as controls for Group IV.
Statistical analysis was performed using the SPSS software package (version 17.0; SPSS Inc., Chicago, IL). Descriptive statistics, the Mann - Whitney U-test for nonparametric independent variables, Spearman's bivariate correlation analysis, partial correlation analysis, intraclass correlation coefficient. Level of significance was set to P < 0.05. Power analysis was performed using G*Power software (version 3.0.10; University of Kiel, Germany).
All patients gave informed consent for their participation in the study and the anonymous use of their data.
 Results Results | |  |
The age distributions of the patients in all four groups are presented in [Table 1] and [Figure 2]. With the exception of Group IV, in which male patients were significantly younger than female patients, there were no differences in sex among Groups I-III.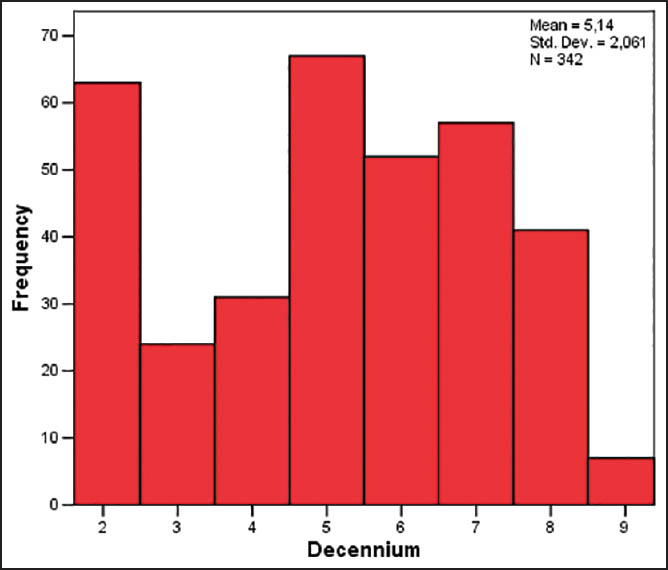 | Figure 2: Histogram illustrating the age distribution in each 10 year age group (Groups I-IV pooled)
Click here to view |
The joint space width measurement results are listed in [Table 2]. No significant difference between the left and right sides was observed among the four groups (P > 0.05).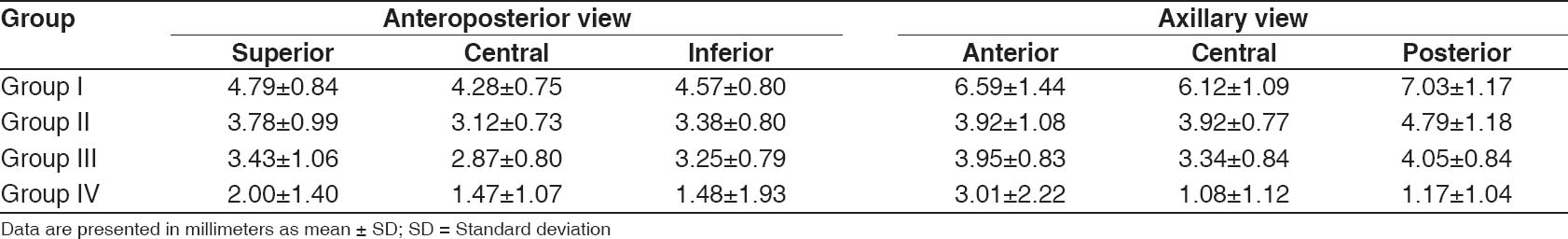 | Table 2: Joint space width in two planes (anteroposterior and axillary) at three levels
Click here to view |
Group I
The interobserver reliability (r) was 0.887-0.910 in the anteroposterior projection and 0.879-0.886 in the axillary projection. Male patients had significantly larger values in the axillary projections than did female patients (anterior axillary, 7.05 ± 1.34 vs. 5.74 ± 1.09, P = 0.003; central axillary, 6.64 ± 0.94 vs. 4.71 ± 1.00, P = 0.001; posterior axillary, 7.48 ± 1.09 vs. 6.16 ± 0.80, P = 0.001).
Group II
The interobserver reliability was excellent in both the anteroposterior projection (r = 0.883-0.871) and axillary projection (r = 0.875-0.862). Male patients had significantly larger values in the inferior anteroposterior and posterior axillary projections than did female patients (inferior anteroposterior, 3.50 ± 0.73 vs. 3.13 ± 0.89, P = 0.041; posterior axillary, 5.16 ± 1.09 vs. 4.16 ± 1.10, P = 0.005).
Group III
The interobserver reliability was excellent in both the anteroposterior projection (r = 0.870-0.866) and axillary projection (r = 0.847-0.811). Male patients had wider joint spaces in the posterior axillary view than did female patients (4.22 ± 0.71 vs. 3.93 ± 0.92, P = 0.32).
Group IV
The interobserver reliability was excellent in the anteroposterior projection (r = 0.830-0.826), but inferior in the axillary projection (r = 0.621-0.732). Male patients had wider joint spaces in the anterior axillary (3.83 ± 2.27 vs. 2.07 ± 1.76, P = 0.001) and central axillary projections than did female patients (1.24 ± 1.10 vs. 0.91 ± 1.12, P = 0.012).
The differences in joint space width among the four groups were all statistically significant at P < 0.001 with the exception of the differences in the central anteroposterior, inferior anteroposterior, and anterior axillary views between Groups I and II [Table 2].
We pooled the data of all four groups and analyzed the relationship between age and joint space width [Figure 3]a and b. There was a significant negative correlation [Table 3] between the joint space width and age at all measured levels in both projections (P < 0.001). This negative correlation was only slightly smaller, but still clearly significant for all measurements, when the patients with osteoarthritis (Group IV) were excluded from the pooled data [Table 3].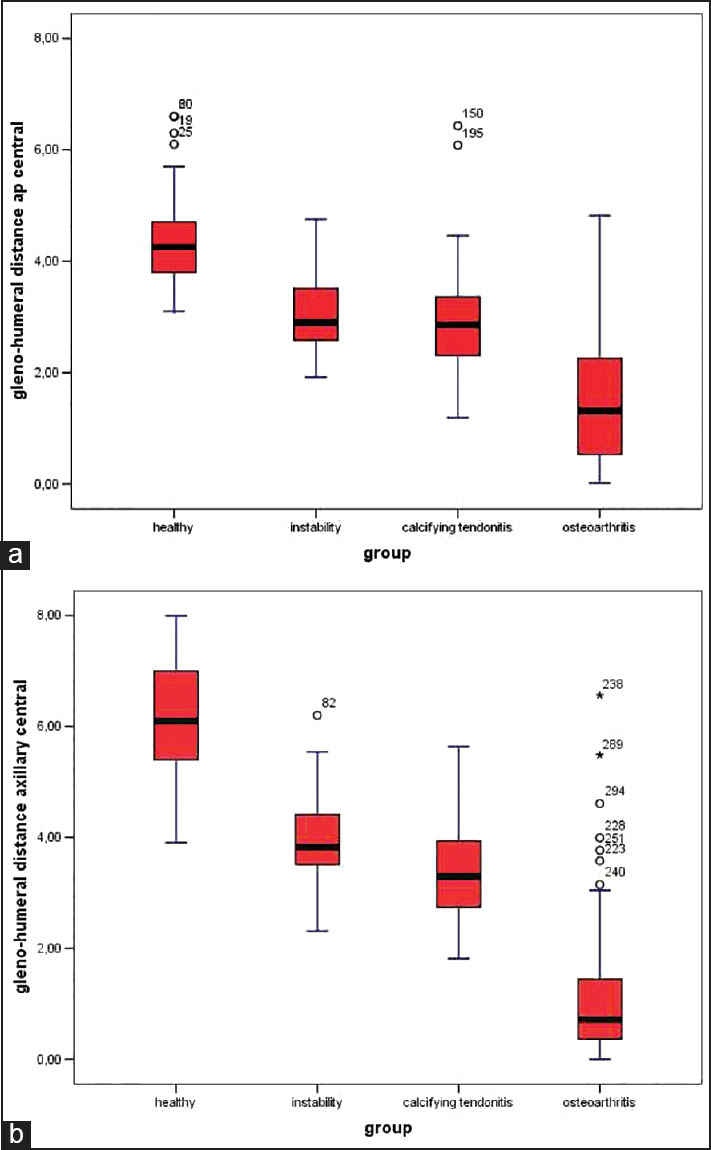 | Figure 3: Box- and -whisker plot shows the glenohumeral distance for the pooled data of Groups I-IV at different ages (e.g., 10-19 years = second decennium) at the central level in the (a) anteroposterior and (b) axillary projections in millimeters. The horizontal line in the middle of each box indicates the median, and the top and bottom borders of the box mark the 75th and 25th percentiles, respectively. The whiskers mark the 90th and 10th percentiles
Click here to view |
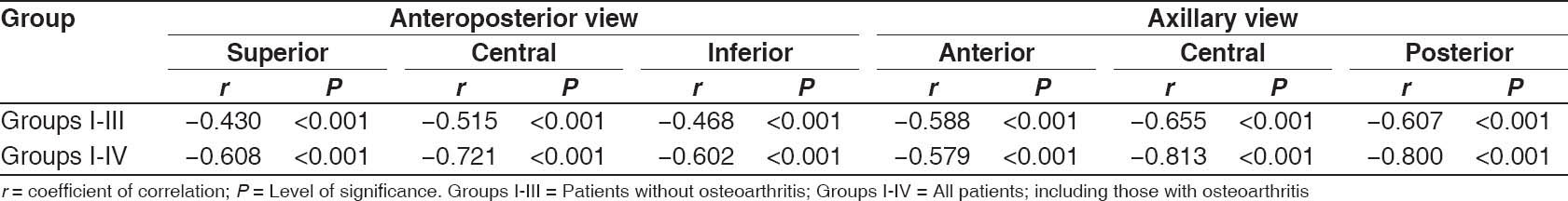 | Table 3 Bivariate correlation (Spearman) between age and joint space width for all measured levels
Click here to view |
 Discussion Discussion | |  |
Our data illustrate a reliable way of assessing the glenohumeral joint space width. A comparable measurement technique was used by Petersson and Redlund-Johnell in 1983 in the frontal plane only. [12] In contrast to the method used in our study, which involves measurement at three distinct levels in two planes, the smallest joint space width should be regarded as the most reliable measurement in clinical settings. This becomes more important in cases of osteoarthritis because this disease is frequently accompanied by the development of caudal humeral osteophytes and dorsal decentering of the humeral head with dorsal glenoid erosion. These changes significantly influence the joint space measurement results because the almost spherical humeral head compared with the greater radius of the glenoid cavity (radiological mismatch) together with dorsal decentering of the head simulate a falsely high measurement in the transverse plane. Otherwise, the measurements at the central level at the anteroposterior and/or axillary projection seem to be sufficient.
Data on the normal shoulder joint space width are sparse. [15] Walch et al. defined partial joint space loss of 2-5 mm in their study, although there was no clear description of the distribution of the values. [14] Petersson and Redlund-Johnell described a normal joint space as about 4-5 mm. [12] They measured the joint space width at three levels with a ruler in the anteroposterior projection with external rotation of the forearm in 88 men and 87 women (10-11 patients in each 10 year age group). They observed significantly higher values for men than women without differences between left and right. They found a significant positive correlation (the r-value illustrating the amount of correlation was not provided) between age and joint space width in women, but not in men, in the superior and central regions (not at the inferior level) with an increase in the joint space over time. The main discrepancy between their results and ours is most likely due to the differences between the methodologies used. We used neutral rotation of the forearm when obtaining the anteroposterior radiographs. Humeral rotation significantly influences biometric measurements at the shoulder. We also used the axillary view in a much larger number of patients. Digital imaging may also improve measurement accuracy [Figure 3]a and b. [16]
The measurement tool used is very important. Digital X-ray allows for increased accuracy by at least one magnitude compared with an ordinary ruler; the differences among the age groups in this study were relatively small compared with the maximum accuracy used [Figure 3]a and b.
In another study, the author measured the cartilage thickness of the humeral head in 19 patients in three different age groups (<65, 65-75, and >75 years) with values of 1.98 ± 0.25 mm, 1.90 ± 0.24 mm, and 1.13 ± 0.32 mm at three measuring sites without significant differences among the age groups (although a P-value was not provided). [11] A post-hoc power analysis revealed a power of 0.1-0.3 for the reported values in that study, which was not sufficient to substantiate the conclusions.
Nové-Josserand et al. reviewed the data of 200 patients (400 shoulders) aged 70-101 years in a geriatric ward. They categorized the glenohumeral joints of patients into three groups: Normal, presence of inferior humeral osteophytes without joint space narrowing, and loss of joint space consistent with osteoarthritis. The glenohumeral joint was found to be normal without any signs of remodeling in 72.00% (288 shoulders). Osteophytes were found in 23.25% (93 shoulders), and complete loss of joint space was found in 7.00% (14 shoulders). [17]
Using light microscopy, Meachim found a mean 1.48 mm thickness of the uncalcified cartilage at the central articulating humeral surface in 32 formal saline-fixed tissue specimens from 16 female patients without macroscopic fibrillation. [13] The author did not observe a significant difference among three consecutive age groups (25-44 years, n = 9; 45-64 years, n = 13; and 65-75 years, n = 10). Again, the number of patients compared with the relatively small differences in the observed joint space width (1.48, 1.42, and 1.47 mm, respectively) is not sufficient to substantiate such an analysis in our opinion. The fact that the use of formal saline fixation may have influenced the cartilage thickness, and the missing glenoid cartilage measurements limit the comparability with our results.
In another publication, the author described the aging process of 37 left shoulder joints to initially involve the periphery with fibrillation of the humeral cartilage surface and almost similar at the glenoid cavity, which could occur as early as the second decade of life. However, involvement of the central region was exceptional under the age of 50 years. [18]
We observed significant differences between male and female patients in some projections of our investigated groups, in contrast to the findings of some other authors (see above). [12],[17] In general, men have larger humeral heads, [15] which influences the measurements. The data should be interpreted cautiously because the number of patients decreases as subgroups are defined, and the conclusion of the absence of a significant relationship may not have enough statistical power to exclude a type II error, which is a problem in many studies in orthopedic surgery. [19]
Our study is one of the first to measure the glenohumeral joint space width on radiographs in young adult patients (age range, 14-21 years) with otherwise normal shoulder radiographs. The observation of a gradual decrease in the glenohumeral joint space width beginning in early adulthood has never been previously described and is in contrast to findings by other authors. [12],[13]
According to our results, measurements of the joint space width on standardized shoulder radiographs should be interpreted about the patient's age and not as absolute figures, even in the absence of manifest osteoarthritis. The strong correlation of joint space narrowing with osteoarthritis in our study suggests that this finding should be integrated into the routinely used description and classification, which is currently based on the size of humeral osteophytes alone. [20]
There are some limitations of our study. First, we indirectly investigated the cartilage thickness by measuring the glenohumeral joint space from bone to bone. Equating the joint space width on X-rays with the cartilage thickness would presuppose tight contact among the joint components at all measured sites. Because of the much larger glenoid cavity diameter than the humeral head diameter, there is a potential for mismatch of the joint, which is intrinsically unstable and is passively and actively balanced by the soft tissues, such as the glenohumeral ligaments, capsule, and surrounding muscles, especially the rotator cuff. Any factor that influences joint balance has the potential to influence joint space measurements. The presence of a mechanism involving the maturation and aging of the soft tissues is possible. Such changes would cause loss of elasticity of the capsule, glenohumeral ligaments, and rotator cuff tendons with time with an increase in the joint reaction forces and a reduction in the cartilage thickness. Decreased shoulder joint mobility and hyperlaxity with increasing age has been confirmed in several studies. [21],[22],[23],[24],[25],[26]
Measurements using digital radiographs are more accurate than traditional measurements using a ruler but are still prone to variability because of the distances involved (i.e., the distances between the tube and patient and between the patient and detector) and the different thicknesses of the patients. Because there is no practicable way to limit this variability further, we believe that the number of patients is large enough to statistically equalize the data.
Another mechanism responsible for joint space narrowing is aging of the cartilage itself. Several studies have shown that articular cartilage undergoes age-dependent changes in its matrix (structural, molecular, and mechanical) and chondrocyte function (synthetic activity, mitotic activity, and responsiveness to anabolic cytokines and mechanical stimuli). [10],[27],[28],[29] This process does not start at a given age, as previously suggested by several authors, but is apparently continuously detectable from the early years of life to old age. [10]
We, therefore, believe that our data illustrate the aging process of the glenohumeral cartilage with joint space narrowing over time. Our results are very reliable in contrast to the above-described historical studies because of the refined methodology used, which have higher accuracy, and the greater number of patients studied.
Because standardized radiographs of the shoulder are still the gold standard for the diagnosis of osteoarthritis, the data of this study are relevant for clinical practice and decision-making regarding shoulder surgery. [1],[2],[30] The accuracy of joint space measurements for individual patients is limited for the above-described reasons and should be used cautiously.
 Conclusions Conclusions | |  |
The glenohumeral joint space width decreases with increasing age beginning in early adulthood. This age-dependent joint space narrowing is enhanced in patients with osteoarthritis.
 References References | |  |
| 1. | Habermeyer P, Engel G. Endoprothetik. In: Habermeyer P, editor. Schulterchirurgie. 3 rd ed. München, Jena: Elsevier, Urban & Fischer; 2005. p. 497-553.  |
| 2. | Matsen FA, Rockwood CA, Wirth MA, Lippitt SB, Parsons M. Glenohumeral arthritis and its management. In: Rockwood CA, Matsen FA, Wirth MA, Lippitt SB, editors. The Shoulder. Philadelphia: Saunders; 2004. p. 879-1007.  |
| 3. | Valdes AM, Spector TD. The contribution of genes to osteoarthritis. Med Clin North Am 2009;93:45-66.  |
| 4. | Aigner T, Fundel K, Saas J, Gebhard PM, Haag J, Weiss T, et al. Large-scale gene expression profiling reveals major pathogenetic pathways of cartilage degeneration in osteoarthritis. Arthritis Rheum 2006;54:3533-44.  |
| 5. | Aigner T, Zien A, Hanisch D, Zimmer R. Gene expression in chondrocytes assessed with use of microarrays. J Bone Joint Surg Am 2003;85-A Suppl 2:117-23.  |
| 6. | Zien A, Gebhard PM, Fundel K, Aigner T. Phenotyping of chondrocytes in vivo and in vitro using cDNA array technology. Clin Orthop Relat Res 2007;460:226-33.  |
| 7. | Aspden RM. Osteoarthritis: A problem of growth not decay? Rheumatology (Oxford). 2008;47:1452-60.  |
| 8. | Loughlin J. The genetic epidemiology of human primary osteoarthritis: Current status. Expert Rev Mol Med 2005;7: 1-12.  |
| 9. | Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol 2007;213:626-34.  |
| 10. | Martin JA, Buckwalter JA. The role of chondrocyte senescence in the pathogenesis of osteoarthritis and in limiting cartilage repair. J Bone Joint Surg Am 2003;85-A Suppl 2:106-10.  |
| 11. | Petersson CJ. Degeneration of the gleno-humeral joint. An anatomical study. Acta Orthop Scand 1983;54:277-83.  [ PUBMED] |
| 12. | Petersson CJ, Redlund-Johnell I. Joint space in normal gleno-humeral radiographs. Acta Orthop Scand 1983;54:274-6.  [ PUBMED] |
| 13. | Meachim G. Effect of age on the thickness of adult articular cartilage at he shoulder joint. Ann Rheum Dis 1971;30:43-6.  [ PUBMED] |
| 14. | Walch G, Boulahia A, Boileau P, Kempf JF. Primary glenohumeral osteoarthritis: Clinical and radiographic classification. The Aequalis Group. Acta Orthop Belg 1998;64 Suppl 2:46-52.  |
| 15. | Kircher J, Morhard M, Magosch P, Ebinger N, Lichtenberg S, Habermeyer P. How much are radiological parameters related to clinical symptoms and function in osteoarthritis of the shoulder? Int Orthop 2010;34:677-81.  |
| 16. | Nyffeler RW, Werner CM, Sukthankar A, Schmid MR, Gerber C. Association of a large lateral extension of the acromion with rotator cuff tears. J Bone Joint Surg Am 2006;88:800-5.  |
| 17. | Nové-Josserand L, Walch G, Adeleine P, Courpron P. Effect of age on the natural history of the shoulder: A clinical and radiological study in the elderly. Rev Chir Orthop Reparatrice Appar Mot 2005;91:508-14.  |
| 18. | Meachim G, Emery IH. Cartilage fibrillation in shoulder and hip joints in Liverpool necropsies. J Anat 1973;116:161-79.  [ PUBMED] |
| 19. | Pike J, Leith J. Type II error in the shoulder and elbow literature. J Shoulder Elbow Surg 2009;18:44-51.  |
| 20. | Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am 1983;65:456-60.  [ PUBMED] |
| 21. | Larsson LG, Baum J, Mudholkar GS, Srivastava DK. Hypermobility: Prevalence and features in a Swedish population. Br J Rheumatol 1993;32:116-9.  |
| 22. | Larsson LG, Baum J, Mudholkar GS. Hypermobility: Features and differential incidence between the sexes. Arthritis Rheum 1987;30:1426-30.  |
| 23. | Jansson A, Saartok T, Werner S, Renström P. General joint laxity in 1845 Swedish school children of different ages: Age- and gender-specific distributions. Acta Paediatr 2004; 93:1202-6.  |
| 24. | Jansson A, Saartok T, Werner S, Renström P. Evaluation of general joint laxity, shoulder laxity and mobility in competitive swimmers during growth and in normal controls. Scand J Med Sci Sports 2005;15:169-76.  |
| 25. | Gedalia A, Press J. Articular symptoms in hypermobile schoolchildren: A prospective study. J Pediatr 1991;119: 944-6.  |
| 26. | Wordsworth P, Ogilvie D, Smith R, Sykes B. Joint mobility with particular reference to racial variation and inherited connective tissue disorders. Br J Rheumatol 1987;26:9-12.  [ PUBMED] |
| 27. | Buckwalter JA, Woo SL, Goldberg VM, Hadley EC, Booth F, Oegema TR, et al. Soft-tissue aging and musculoskeletal function. J Bone Joint Surg Am 1993;75:1533-48.  |
| 28. | Buckwalter JA, Mankin HJ. Articular cartilage. Part I: Tissue design and chondrocyte-matrix interactions. J Bone Joint Surg Am 1997;79:600-11.  |
| 29. | Buckwalter JA, Martin J, Mankin HJ. Synovial joint degeneration and the syndrome of osteoarthritis. Instr Course Lect 2000;49:481-9.  |
| 30. | Walch G, Badet R, Riand N, Boulahia A, Kempf JF. Primary gleno-humeral osteoarthritis: Clinical and radiological classification. In: Walch G, Boileau P, editors. Shoulder Arthroplasty. Berlin, Heidelberg New York: Springer; 1999. p. 195-202.  |
[Figure 1], [Figure 2], [Figure 3]
[Table 1], [Table 2], [Table 3]
|
