| |


 |
| Year : 2015 | Volume
: 9
| Issue : 1 | Page : 1-5 |
|
|
|
|
|
ORIGINAL ARTICLE Increasing preoperative dislocations and total time of dislocation affect surgical management of anterior shoulder instability
Patrick J Denard1, Xuesong Dai2, Stephen S Burkhart2
1 Southern Oregon Orthopedics, Medford; Department of Orthopedics and Rehabilitation, Oregon Health and Science University, Portland, Oregon, USA
2 The San Antonio Orthopedic Group, San Antonio, Texas, USA
Correspondence Address:
Stephen S Burkhart
150 E Sonterra Blvd, Suite 300, San Antonio, Texas 78259
USA
 Source of Support: None, Conflict of Interest: Drs. Denard and Burkhart are consultants for Arthrex, Inc. The other author has no confl icts of interest to report.  | 2 |
DOI: 10.4103/0973-6042.150215
 |
|
|
|
| Date of Web Publication | 28-Jan-2015 |
 Abstract Abstract | | |
Purpose: Our purpose was to determine the relationship between number of preoperative shoulder dislocations and total dislocation time and the need to perform bone deficiency procedures at the time of primary anterior instability surgery. Our hypothesis was that need for bone deficiency procedures would increase with the total number and hours of dislocation.
Materials and Methods: A retrospective review was performed of primary instability surgeries performed by a single surgeon. Patients with <25% glenoid bone loss were treated with an isolated arthroscopic Bankart repair. Those who also had an engaging Hill-Sachs lesion underwent arthroscopic Bankart repair with remplissage. Patients with >25% glenoid bone loss were treated with Latarjet reconstruction. Number of dislocations and total dislocation time were examined for their relationship with the treatment method.
Results: Ten arthroscopic Bankart repairs, 13 arthroscopic Bankart plus remplissage procedures, and 9 Latarjet reconstructions were available for review. Total dislocations (P = 0.012) and total hours of dislocation (P = 0.019) increased from the Bankart, to the remplissage, to the Latarjet groups. Patients with a total dislocation time of 5 h or more were more likely to require a Latarjet reconstruction (P = 0.039). Patients with only 1 preoperative dislocation were treated with an isolated Bankart repair in 64% (7 of 11) of cases, whereas those with 2 or more dislocations required a bone loss procedure in 86% (18 of 21) of cases (P = 0.013).
Conclusion: Increasing number of dislocations and total dislocation time are associated with the development of glenoid and humeral head bony lesions that alter surgical management of anterior shoulder instability. The necessity for the addition of a remplissage to an arthroscopic Bankart repair or the use of a Latarjet reconstruction increases with only 1 recurrent dislocation.
Level of evidence: Level III, retrospective comparative study.
Keywords: Bankart, Latarjet, remplissage, shoulder dislocation
How to cite this article:
Denard PJ, Dai X, Burkhart SS. Increasing preoperative dislocations and total time of dislocation affect surgical management of anterior shoulder instability. Int J Shoulder Surg 2015;9:1-5 |
 Introduction Introduction | |  |
Anterior shoulder dislocation is associated with approximately a 67% chance of recurrence in individuals under the age of 40. [1],[2] Arthroscopic stabilization may reduce the risk of recurrence to <10%. [3],[4] Some authors have therefore proposed primary arthroscopic stabilization for patients with high risk of recurrence, [4],[5] while others have reported that there is no difference in outcome or complication in patients treated with primary stabilization compared to those treated after recurrent dislocations. [6]
Several studies have demonstrated that recurrent anterior instability is associated with the development of associated pathology as well as long-term glenohumeral arthritis. [7],[8],[9],[10] In addition, recurrent instability has been associated with the development of glenoid bone loss and Hill-Sachs lesions. [11],[12],[13] These bony lesions are particularly important because they affect the treatment. In particular, glenoid bone loss >25% or a deep engaging Hill-Sachs lesion are associated with high-risk of recurrence following an isolated arthroscopic Bankart repair. [3],[14],[15] In these settings the addition of an arthroscopic remplissage to a Bankart repair or conversion to a Latarjet reconstruction have been advised. [16],[17] While these procedures have been shown to reduce the risk of recurrent instability, they increase operative complexity and the risk of complication, particularly with regard to Latarjet, which has a complication rate as high as 25%. [18] Therefore, identifying risk factors, which lead to the need for these procedures may be useful in improving outcomes and reducing complications in patients with anterior shoulder instability.
The purpose of this study was to determine the relationship between the number of preoperative shoulder dislocations and total dislocation time and the need for bone deficiency procedures (Latarjet or remplissage) at the time of primary anterior instability surgery. Our hypothesis was that the need for bone deficiency procedures would increase with the total number and hours of dislocation.
 Materials and methods Materials and methods | |  |
Study population
Institutional Review Board approval was obtained prior to commencing the study. A retrospective review was performed of all primary instability surgeries performed by a single surgeon between January 2007 and December 2010. The inclusion criteria were a primary instability procedure consisting of either both an arthroscopic anterior Bankart repair, and an arthroscopic Bankart repair with concomitant remplissage, or an open Latarjet reconstruction. Additional inclusion criteria included a record of the number of dislocations and the total time that the shoulder was dislocated prior to surgery. Exclusion criteria included isolated posterior Bankart repairs, atraumatic multidirectional instability, and revision instability procedures. Seventy nine patients met the inclusion criteria including: 38 arthroscopic anterior Bankart repairs, 29 arthroscopic Bankart repairs with concomitant remplissage procedures, and 12 open Latarjet reconstructions. Complete data about the number of dislocations and total dislocation time was available for 10 Bankart repairs, 13 Bankart plus remplissage procedures, and 9 Latarjet reconstructions.
A chart review was performed to obtain basic demographic data including age at the time of surgery, male or female sex, and dominant extremity. The total number of dislocations prior to surgery and the total hours of dislocation were also obtained by chart review. Total dislocation time was determined by the patient's estimate of the total number of hours that the humeral head was completely separated from the glenoid (total dislocation to reduction time). For example, an individual who dislocated the shoulder 2 times in which the shoulder was out of joint for 30 min prior to reduction the 1 st time and 2 h prior to reduction the 2 nd time would have a total dislocation time of 2.5 h.
Surgical procedures
All surgeries were performed by the senior author. All patients were initially placed in the lateral decubitus position, and a diagnostic arthroscopy was performed. While viewing from an anterosuperolateral portal, the percentage of glenoid bone loss was arthroscopically quantified with a calibrated probe. [19] The depth of the Hill-Sachs lesion was also assessed with a calibrated probe. The arm was then temporarily removed from traction and placed in 90° of abduction and 90° of external rotation to assess for an engaging Hill-Sachs lesion.
During the study period, surgical treatment was based on the following guidelines:
- Patients with <25% glenoid bone loss and a minimal Hill-Sachs lesion were treated with an isolated arthroscopic Bankart repair
- Patients with <25% glenoid bone loss and Hill-Sachs lesion >4 mm in depth that was engaging were treated with an arthroscopic Bankart repair as well as an arthroscopic remplissage
- Patients with >25% glenoid bone loss (confirmed arthroscopically first) were treated with an open Latarjet reconstruction
- Selected patients with <25% glenoid bone loss, who also had a deep Hill-Sachs lesion that extended so far medially or superiorly that the surgeon felt that a remplissage would adversely change the vector of the infraspinatus (thereby contraindicating remplissage as a treatment option), were treated with a Latarjet reconstruction.
The techniques for each of these procedures have previously been described in detail and are not reviewed here since this paper examines the preoperative factors associated with the selection of the procedures, and not the functional outcome or recurrence rate.
Statistical analysis
Statistical analysis was conducted by a trained statistician using SAS 9.2 (SAS Institute; Cary, NC, USA). Continuous data were described by means and 95% confidence intervals (CIs). To examine factors associated with each procedure, Chi-square tests or Fisher's exact tests (where data were sparse) were conducted to determine differences in categorical variables; continuous variables were assessed via Wilcoxon Rank Sum test for nonparametric data. The data were further analyzed combining procedure groups to evaluate:
- No bone loss (Bankart) versus bone loss (remplissage or Latarjet), and
- Open (Latarjet) versus arthroscopic treatment (Bankart and remplissage).
Two-tailed P < 0.05 was considered significant.
 Results Results | |  |
There was no difference in baseline characteristics including age, sex, and dominant arm between the three groups [Table 1].
Patients who underwent Latarjet reconstruction had more dislocations prior to the index surgery, had their shoulders dislocated for a longer period, and had a higher percentage of glenoid bone loss at the time of treatment [Table 2].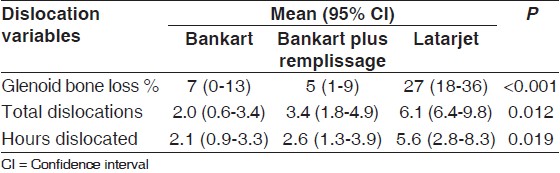 | Table 2: Glenoid bone loss and dislocation characteristics of the study population
Click here to view |
For comparative purposes, the data were also analyzed by arthroscopic treatment (Bankart as well as Bankart plus remplissage) versus open treatment (Latarjet). Patients treated with an arthroscopic approach had a mean 2.8 dislocations (95% CI: 1.8-3.8) compared to 6.1 dislocations (95% CI: 2.4-9.8) in those requiring Latarjet reconstruction (P = 0.012). Patients with 5 or more preoperative dislocations were more likely to be treated with a Latarjet (P = 0.023). The arthroscopic patients also had a shorter dislocation time (2.4 h; 95% CI: 1.5-3.3) compared to the Latarjet group (5.6 h; 95% CI: 2.8-8.3) (P = 0.006). Patients with a total dislocation time of 5 h or more were more likely to require a Latarjet reconstruction (P = 0.039).
Finally, the patients were placed into two groups to compare no bone loss (Bankart) versus bone loss (Bankart plus remplissage; and Latarjet). In the Bankart group, a mean of 2.0 dislocations (95% CI: 0.6-3.4) occurred before surgery, compared to a mean of 4.5 dislocations (95% CI: 2.8-6.2) in the bone loss group (P = 0.014). There was no difference in the total dislocation time between the two groups (2.1 h vs. 3.8 h; P = 0.125). Patients with more than 1 preoperative dislocation were more likely to require a bone loss procedure (P = 0.013). Patients with only 1 preoperative dislocation were treated with an isolated Bankart repair in 64% (7 of 11) of cases, whereas those with 2 or more dislocations required a bone loss procedure in 86% (18 of 21) of cases.
 Discussion Discussion | |  |
This study examined the relationship of how the preoperative number of dislocations and the total dislocation time affect the complexity of a primary glenohumeral stabilization procedure. Our data support the hypothesis that both increasing number of dislocations and the total dislocation time lead to an increased need for more complex procedures to address bone deficiency at the time of primary stabilization procedure. This study adds to the growing recognition that recurrent anterior glenohumeral dislocations have pathological consequences that may affect the ultimate treatment.
In a prospective arthroscopic evaluation of 91 patients with anterior shoulder instability, Habermeyer et al. demonstrated that increasing number of dislocations were associated with progressive damage to the capsulolabral complex. [7] Gutierrez et al. reviewed 96 patients who underwent an arthroscopic Bankart repair and noted that those with more than 1 dislocation were more likely to have associated lesions. [8] A posterior Bankart tear was observed in 28% of 1 st time dislocations, which increased to 47% in patients with 2 or more dislocations. Similarly, superior labrum anterior posterior lesions were observed in 12% of 1 st time dislocations, compared to 24% in recurrent cases.
Recurrent shoulder instability is associated with the development of glenohumeral arthritis. Franceschi et al. noted a 2.3 times increased risk of glenohumeral arthritis with increasing number of preoperative dislocations. [9] At 25 years follow-up Hovelius and Saeboe noted that patients with just 1 recurrent subluxation or dislocation had moderate or severe glenohumeral arthritis in 35% of cases compared to 17% in patients who did not have recurrent instability. [10]
In addition to soft-tissue pathology and glenohumeral arthritis, increasing number of dislocations appears to be related to the development of bony lesions. Studies by Edwards et al. [11] and Sugaya et al., [12] for instance, have demonstrated that Hill-Sachs lesions and some degree of glenoid bone loss are nearly universal in patients with recurrent instability. In 2000, Burkhart and De Beer first brought attention to the impact of these bony defects on recurrence after arthroscopic Bankart repairs. [3] They reported that in the presence glenoid bone loss >25% or an engaging Hill-Sachs lesion, recurrence after an isolated Bankart repair was 67% at a mean follow-up of 27 months. However, when glenoid bone loss was <25% and when the Hill-Sachs lesion was not engaging, an isolated arthroscopic Bankart repair was successful in 96% of cases. Subsequently, Burkhart et al. reported that when an open Latarjet reconstruction was performed for patients with glenoid bone loss >25% or an engaging Hill-Sachs lesion their recurrence rate decreased to 4.9%. [16] Since, the development of bony defects alters treatment protocols, understanding risk factors for the development of these lesions is important. Moreover, preventing the development of these lesions may allow less invasive treatment in the form of arthroscopic stabilization as opposed to open bone block procedures such as the Latarjet.
Milano et al. performed computed tomography scans on 161 patients with anterior shoulder instability and assessed risk factors for the development of glenoid bone defects. [13] They reported that male gender and increasing number of dislocations were associated with the development of a glenoid bone defect. Increasing the number of dislocations in particular was associated with a 9.5 times risk for the development of glenoid bone loss >20%. The current study helps further quantify the impact of recurrent dislocations on the development of bony defects. Patients with a single dislocation were treated with an isolated Bankart repair in 64% of cases. In other words, in 64% of cases the glenoid bone loss or Hill-Sachs defect were not substantial enough to require more than arthroscopic Bankart repair. On the other hand, in patients with 2 or more dislocations there was judged to be a substantial bony lesion requiring a Bankart repair plus remplissage or Latarjet in 86% of cases. In addition, patients with 5 or more dislocations were more likely to undergo a Latarjet reconstruction. In the authors' opinion, these findings support primary arthroscopic stabilization in patients with high risk for recurrent anterior shoulder instability.
To the best of our knowledge and belief, this is the first study to examine the relationship between total dislocation time and method of stabilization so far. Total hours of dislocation increased from a mean of 2.1 in the Bankart group, to 2.6 in the Bankart plus remplissage group, to 5.6 in the Latarjet group. Most notably, patients with a total dislocation time of 5 h or more were more likely to require Latarjet reconstruction. Total dislocation time, therefore, appears to be related to the development of bony lesions and may be another worthwhile factor to consider in the history of a patient with shoulder instability.
This study is limited by the lack of inclusion of postoperative follow-up. Specifically, the rate of postoperative recurrence is not known in this cohort of patients. However, our goal was simply to examine how the number and hours of preoperative dislocations affected treatment. Moreover, these data have previously been published on other cohorts of patients that were treated with a similar algorithm. [3],[16],[17] There is also a potential selection bias toward more bony procedures in patients with more dislocations or a total dislocation time since these factors were known prior to surgery. However, we believe this is unlikely, since, the baseline demographics of the patients were similar, and a consistent surgical algorithm was used based on arthroscopic evaluation. Finally, the major limitation of this was the retrospective collection of a number of dislocations and total dislocation in time. In our experience, when patients are asked these questions that they demonstrate good recall. However, because the questions are not asked prospectively, and we only included patients with complete information regarding number and hours of dislocation, many patients were excluded from the study, limiting the size of the cohort. Prospective evaluation is, therefore, necessary to corroborate our findings.
 Conclusion Conclusion | |  |
Increasing number of dislocations and the total dislocation time are associated with the development of glenoid and humeral head bony lesions that alter surgical management of anterior shoulder instability. The addition of a remplissage to an arthroscopic Bankart repair or the use of a Latarjet reconstruction increases with only 1 recurrent dislocation. These findings support primary arthroscopic stabilization in patients at high risk for recurrent anterior glenohumeral instability.
 Acknowledgments Acknowledgments | |  |
The authors wish to express their appreciation to Shannon Hiratzka, MPH, for her assistance with the statistical analysis of the data for this study.
 References References | |  |
| 1. | Hovelius L, Olofsson A, Sandström B, Augustini BG, Krantz L, Fredin H, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am 2008;90:945-52.  |
| 2. | Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am 2006;88:2326-36.  |
| 3. | Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94.  |
| 4. | Robinson CM, Jenkins PJ, White TO, Ker A, Will E. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder. A randomized, double-blind trial. J Bone Joint Surg Am 2008;90:708-21.  |
| 5. | Chahal J, Marks PH, Macdonald PB, Shah PS, Theodoropoulos J, Ravi B, et al. Anatomic Bankart repair compared with nonoperative treatment and/or arthroscopic lavage for first-time traumatic shoulder dislocation. Arthroscopy 2012;28:565-75.  |
| 6. | Grumet RC, Bach BR Jr, Provencher MT. Arthroscopic stabilization for first-time versus recurrent shoulder instability. Arthroscopy 2010;26:239-48.  |
| 7. | Habermeyer P, Gleyze P, Rickert M. Evolution of lesions of the labrum-ligament complex in posttraumatic anterior shoulder instability: A prospective study. J Shoulder Elbow Surg 1999;8:66-74.  |
| 8. | Gutierrez V, Monckeberg JE, Pinedo M, Radice F. Arthroscopically determined degree of injury after shoulder dislocation relates to recurrence rate. Clin Orthop Relat Res 2012;470:961-4.  |
| 9. | Franceschi F, Papalia R, Del Buono A, Vasta S, Maffulli N, Denaro V. Glenohumeral osteoarthritis after arthroscopic Bankart repair for anterior instability. Am J Sports Med 2011;39:1653-9.  |
| 10. | Hovelius L, Saeboe M. Neer Award 2008: Arthropathy after primary anterior shoulder dislocation-223 shoulders prospectively followed up for twenty-five years. J Shoulder Elbow Surg 2009;18:339-47.  |
| 11. | Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy 2003;19:732-9.  |
| 12. | Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 2003;85-A:878-84.  |
| 13. | Milano G, Grasso A, Russo A, Magarelli N, Santagada DA, Deriu L, et al. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med 2011;39:1870-6.  |
| 14. | Burkhart SS, Danaceau SM. Articular arc length mismatch as a cause of failed Bankart repair. Arthroscopy 2000;16:740-4.  |
| 15. | Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006;88:1755-63.  |
| 16. | Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007;23:1033-41.  |
| 17. | Boileau P, O′Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am 2012;94:618-26.  |
| 18. | Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 2012;94:495-501.  |
| 19. | Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: An indicator of significant glenoid bone loss. Arthroscopy 2004;20:169-74.  |
[Table 1], [Table 2]
|
