| |


 |
| Year : 2015 | Volume
: 9
| Issue : 1 | Page : 9-12 |
|
|
|
|
|
CASE SERIES A new tear pattern of the rotator cuff and its treatment: Fosbury flop tears
Alexandre Lädermann1, Patrick J Denard2, Frank C Kolo3
1 Division of Orthopaedics and Trauma Surgery, La Tour Hospital, Meyrin; Faculty of Medicine, University of Geneva, Switzerland
2 Department of Orthopaedics and Rehabilitation, Oregon Health and Science University, Portland, USA
3 Rive Droite Radiology Center, Geneva, Switzerland
Correspondence Address:
Alexandre Lädermann
La Tour Hospital, Av. J.-D.-Maillard 3, 1217 Meyrin/Geneva
Switzerland
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/0973-6042.150217
 |
|
|
|
| Date of Web Publication | 28-Jan-2015 |
 Abstract Abstract | | |
Purpose: The purpose of this report is to describe a new full-thickness tear pattern of the posterosuperior rotator cuff with reversal healing. We describe the specific radiologic signs associated with this tear pattern and the arthroscopic rotator cuff repair technique.
Materials and Methods: A prospective radiologic and clinical study collected all patients with a magnetic resonance imaging arthrogram that underwent an arthroscopic rotator cuff repair over a 1 year period.
Results: Among 97 patients, five demonstrated a tear of the posterosuperior rotator cuff with reversal healing. Characteristic radiographic findings included a thicker tendon than normal, the presence of a stump and accumulation of liquid in the superior-medial part of the subacromial bursa, and adhesions between the supraspinatus tendon and the wall of the subacromial bursa.
Conclusion: Avulsion of the posterosuperior rotator cuff with reversal healing on its bursal-side is a less common condition. This type of lesion and distinct radiographic signs that can be recognized to facilitate anatomic repair of the rotator cuff.
Level of evidence: Level IV.
Keywords: Arthroscopic repair, fosbury flop supraspinatus sign, full-thickness tear, infraspinatus, magnetic resonance imaging, rotator cuff tendon, supraspinatus
How to cite this article:
Lädermann A, Denard PJ, Kolo FC. A new tear pattern of the rotator cuff and its treatment: Fosbury flop tears. Int J Shoulder Surg 2015;9:9-12 |
 Introduction Introduction | |  |
The musculotendinous units of the rotator cuff play a crucial role in nonpathological and pathologic conditions of the shoulder. [1] Tears of the supraspinatus may occur at the musculotendinous junction, [2] bone insertion, [3] or within the tendon itself. [4] Tearing of the tendon from the bone is most common and is typically described a partial bursal-sided tear, partial articular-sided tendon tear, [5] interstitial partial-thickness tear or a full-thickness tear [Figure 1].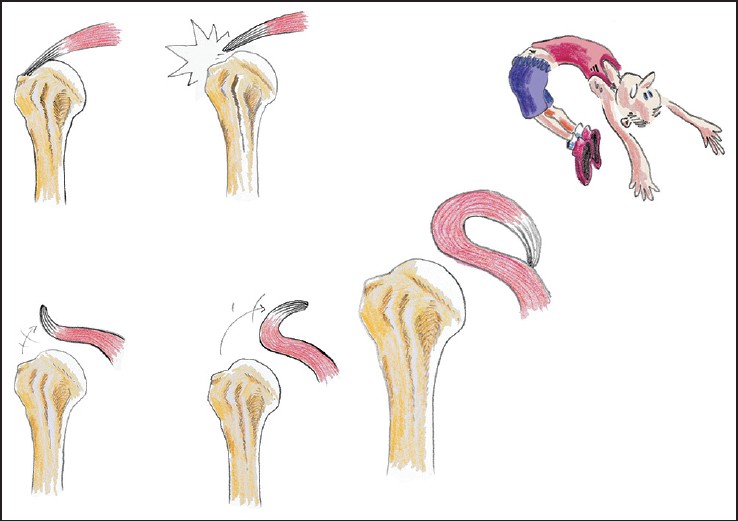 | Figure 1: Arthroscopic view of a right shoulder through lateral portal after bursectomy and creation of a bone socket for medial row anchor placement. The supraspinatus tendon unusually thick and has the appearance of ulcerations and flanges of the bursal-side (H = Hole of the tap; HH = Humeral head; SS = Supraspinatus tendon)
Click here to view |
Full-thickness tears come in a variety of patterns often classified as crescent tears, L-shaped tears, reverse L-shaped tears, and U-shaped tears. [6] Recognizing the tear pattern is important in understanding the pathology, proposing treatment, and eventually planning repair.
The purpose of this report was to analyze a new full-thickness tear pattern of the posterosuperior rotator cuff associated with reversal healing which we have termed the "Fosbury flop" tear, to determine its prevalence, and to describe the arthroscopic rotator cuff repair technique. The hypothesis was that this tear pattern had specific radiologic signs associated with this tear and the arthroscopic rotator cuff repair technique.
 Materials and methods Materials and methods | |  |
Study population
Between March 2010 and September 2011, the authors noted two intraoperative cases of particular healing of the supraspinatus and/or infraspinatus on itself that were retrospectively correlated with specific radiological images. Based on these findings, a prospective radiologic and clinical study was undertaken from October 2011 to September 2012. Prior to the beginning, the study was approved by the Local Ethics Committee. These cases were part of a prospective cohort of all patients undergoing arthroscopic rotator cuff repair at one institution. Inclusion criteria were all patients that underwent an arthroscopic rotator cuff repair and had a preoperative magnetic resonance imaging (MRI) of the shoulder with an intraarticular contrast.
Data collection
Background information (age, gender, side of shoulder pathology, hand dominance, workers' compensation status), detailed medical and surgical history, and tobacco use was routinely documented at the initial evaluation. Preoperatively, Constant Score, [7] American Shoulder and Elbow Surgeons score, [8] range of motion, visual analog scale pain score graded from 0 (no pain) to 10 points (maximal pain).
Radiographic evaluation
Preoperative MRI arthrograms were systematically collected with intraoperative findings being the gold standard control. One experienced musculoskeletal radiologist analyzed all MRIs. Rotator cuff abnormalities were assessed qualitatively. The extent of tendon retractions, tendon thickness, degree of fatty infiltration, [9] and morphological description of rotator cuff tears were recorded.
Surgical technique
The operations were performed by a single surgeon who used a consistent operative technique. The patient was placed in a beach chair position with the arm in horizontal traction. A diagnostic arthroscopy was performed with an arthroscopic pump maintaining pressure at 50 mm Hg. The biceps was tenotomized or tenodesed according to previously described factors. [10] The subscapularis tendon was inspected, and the lesion classified according to Lafosse et al., [11] and if torn, repaired to the lesser tuberosity bone bed with a single-row suture technique following a three-sided release. Attention was then turned to the posterosuperior rotator cuff (supraspinatus and infraspinatus tendons). Rotator cuff tear size was assessed after subacromial bursectomy but before rotator cuff debridement; tears were classified as small, medium, large, or massive based on the anterior-to-posterior dimension. [12] The appearances of the tears were unusual with thick tendons and images looking like ulcerations on the bursal-side [Figure 1]. After a progressive dissection, medial adhesions of the bursal layer were found. Excavation of the rotator cuff permitted return of the bursal layer from 180° (video illustration). Mobilization of the rotator cuff margins allowed repair [Figure 2]. To the lateral bone bed. The decision to use single-row or fixation depended on the tissue quality and tension on the repair. [13] All subjects took part in a standardized rehabilitation protocol. [14] 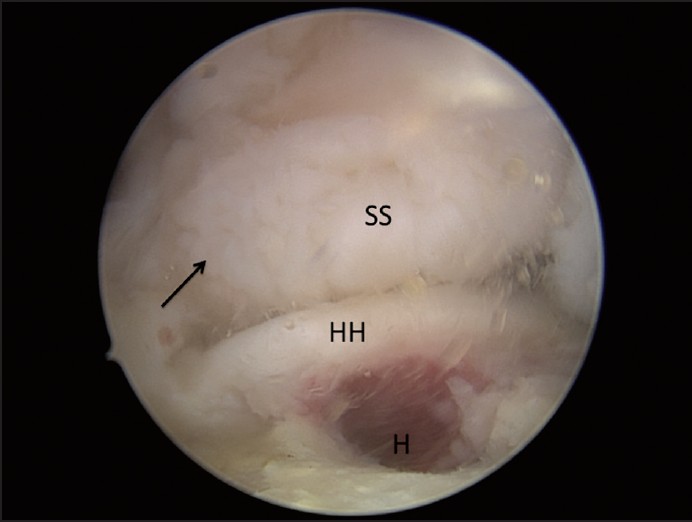 | Figure 2: Arthroscopic view of a right shoulder viewed from lateral portal demonstrates a complete single row repair of the posterosuperior rotator cuff following mobilization of a Fosbury flop tear
Click here to view |
Statistical analysis
The descriptive analysis consisted of frequencies and percentages for discrete data. Means and standard deviations were used for continuous data.
 Results Results | |  |
During the study period, 97 patients underwent an arthroscopic rotator cuff repair. Among them, five demonstrated the unique Fosbury flop tear pattern (prevalence 5%). The baseline characteristics are summarized in [Table 1].
Radiological findings
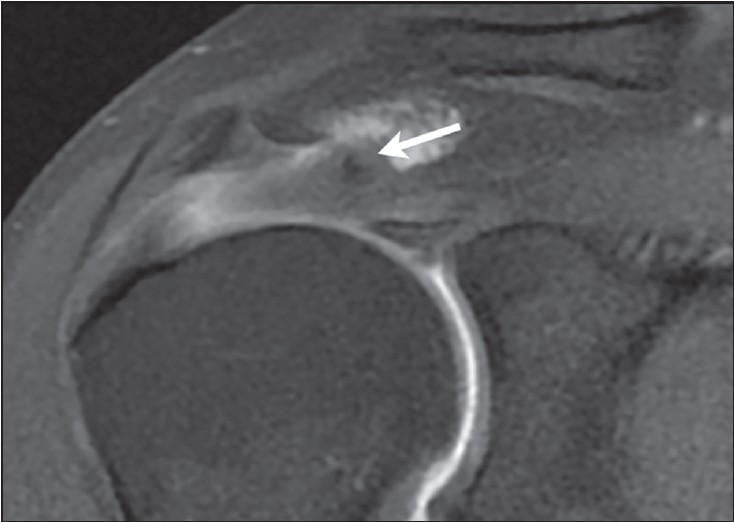
Compared to other patients with full-thickness tear patients with reversal healing showed distinct morphological differences. The mean thickness of the supraspinatus tendon was 11.2 ± 1.1 mm [Figure 3]. The tendon stump was visualized in five patients on the bursal-side of the retracted supraspinatus tendon arboring a superomedial orientation [Figure 4]. These patients also showed accumulation of fluid in the superomedial part of the subacromial bursa, and finally adhesions between the wall of the subacromial bursa and the supraspinatus tendon [Figure 5]. On T1-weighted images with fat saturation abnormal orientation of the tendon, fibers were always noted in the reversed healed stump. Fatty infiltration was stage 0 in three cases and stage 1 in two cases. | Figure 3: Coronal intermediate weighted image without fat saturation of a right shoulder that demonstrate (black arrow) an abnormally thickened supraspinatus (9.5 mm)
Click here to view |
 | Figure 4: Coronal intermediate weighted image without fat saturation that shows the tendon stump projecting on top of the superomedial part of the subacromial bursa. A two-layered structure with the stump is clearly differentiated
Click here to view |
 | Figure 5: Coronal T1-weighted with fat saturation of a right shoulder. Adherences between the bursal tendon side and the wall of the subacromial bursa, fluid in the subacromial bursa, and abnormal orientation of the fibers in the tendon stump (write arrow) are noted
Click here to view |
Intraoperative findings
The supraspinatus tendon was torn in all cases. One was an isolated supraspinatus tears, the subscapularis was involved in one of the five cases and the infraspinatus was involved in three of the five cases. The former was a type-2 tear of the subscapularis that necessitated repair. The mean posterosuperior rotator cuff tear size was 3.6 ± 1.1 cm (range: 2-5 cm). A mean of 2.4 ± 1.3 anchors were used for repair (range: 1-4 anchors). The tension on the torn tendon(s) after the releases allowed a double-row reconstruction in three patients. Poor tissue quality of the reversed part necessitated partial cuff debridement in one case. A complete repair was achieved in all cases. A concomitant modified subacromial decompression, which involved an acromial smoothing and lateral bevel, with preservation of the coracoacromial arch, was performed in all patients. Additional procedures included a distal clavicle excision in two cases.
 Discussion Discussion | |  |
Arthroscopic rotator cuff repair allows a complete evaluation of the glenohumeral joint and the subacromial space, a complete evaluation of the tear pattern and its mobility, and treatment of the frequent concomitant pathology, with minimal trauma afforded to the deltoid insertion.
This case series presents an unusual avulsion of the posterosuperior rotator cuff with reversal healing on its bursal-side we have termed the "Fosbury flop" tear. The prospective design allowed us to provide the prevalence of this lesion. Interestingly, the current study is, to the best of our knowledge, the first detailed report of this tear pattern in the literature. However, this type of lesion and associated radiographic signs has to be recognized. Effectively, the contrary would lead to a nonanatomic repair or to the impossibility to perform the latter.
Important radiographic markers were discovered in the course of this study [Table 2]. The frontal images of the supraspinatus tendon showed a tendon, which appeared thicker than normal [Figure 3]. Furthermore, the tendon stump could be recognized in the supermedial part of the subacromial bursa on the frontal view [Figure 4]. The normal maximum thickness of the supraspinatus tendon is 4.91 ± 0.41 mm. [15] In the present study, the mean thickness was 11.2 ± 1.1 mm. This image was thus termed appropriately the "Fosbury flop sign" since the apparent increased thickness results from the tendon flipping upon itself. Unusual thickness of rotator cuff tendon could be, theoretically, encountered in the context of chronic tendinopathy. However, to the best of our knowledge, such measurement has not been described in the literature. Furthermore, mobilization of the tendon demonstrated that the thickening in the current cases was due to the tendon flipping on itself rather than intrinsic thickening.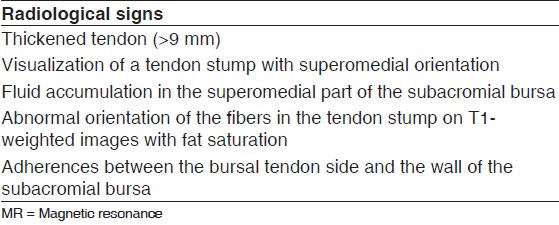 | Table 2: Typical arthro-MR findings in case of Fosbury flop of posterosuperior rotator cuff tears
Click here to view |
Limitations
The main limitation is the lack of mid-to long-term follow-up in order to determine if this particular pathology has the same prognosis than other types of rotator cuff lesions.
 Conclusion Conclusion | |  |
Avulsion of the posterosuperior rotator cuff with reversal healing on its bursal-side is a less common condition. This type of lesion and distinct radiographic signs that can be recognized to facilitate anatomic repair of the rotator cuff.
 References References | |  |
| 1. | Cofield RH. Rotator cuff disease of the shoulder. J Bone Joint Surg Am 1985;67:974-9.  [ PUBMED] |
| 2. | Lädermann A, Christophe FK, Denard PJ, Walch G. Supraspinatus rupture at the musclotendinous junction: An uncommonly recognized phenomenon. J Shoulder Elbow Surg 2012;21:72-6.  |
| 3. | Greiner S, Scheibel M. Bony avulsions of the rotator cuff: Arthroscopic concepts. Orthopade 2011;40:21-4, 26.  |
| 4. | Kneeland JB, Middleton WD, Carrera GF, Zeuge RC, Jesmanowicz A, Froncisz W, et al. MR imaging of the shoulder: Diagnosis of rotator cuff tears. AJR Am J Roentgenol 1987;149:333-7.  [ PUBMED] |
| 5. | Snyder SJ. Arthroscopic Treatment of Partial Articular Surface Tendon Avulsions. Paper Presented at the AAOS/AOSSM Comprehensive Sports Medicine: The Athletic Perspective to Treatment, Controversies and Problem Solving, Lake Tahoe, NV; February 2, 2001.  |
| 6. | Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: A system linking tear pattern to treatment and prognosis. Arthroscopy 2010;26:417-24.  |
| 7. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;160-4.  |
| 8. | Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: Reliability, validity, and responsiveness. J Shoulder Elbow Surg 2002;11:587-94.  |
| 9. | Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and post-operative evaluation by CT scan. Clin Orthop Relat Res 1994;78-83.  |
| 10. | Cunningham G, Lädermann A. Tendon of the long head of the biceps brachii: Tenotomy versus tenodesis? Leading Opin 2011;2:16-8.  |
| 11. | Lafosse L, Lanz U, Saintmard B, Campens C. Arthroscopic repair of subscapularis tear: Surgical technique and results. Orthop Traumatol Surg Res 2010;96 8 Suppl:S99-108.  |
| 12. | DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am 1984;66:563-7.  [ PUBMED] |
| 13. | Denard PJ, Burkhart SS. Techniques for managing poor quality tissue and bone during arthroscopic rotator cuff repair. Arthroscopy 2011;27:1409-21.  |
| 14. | Liotard J. Painful shoulder rehabilitation: How to do it simple. Rev Rhum Monogr 2010;77:239-45.  |
| 15. | Akturk M, Karaahmetoglu S, Kacar M, Muftuoglu O. Thickness of the supraspinatus and biceps tendons in diabetic patients. Diabetes Care 2002;25:408.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
[Table 1], [Table 2]
|
