| |


 |
| Year : 2015 | Volume
: 9
| Issue : 4 | Page : 103-109 |
|
|
|
|
|
ORIGINAL ARTICLE Biomechanical evaluation of inferior scapula notching of reverse shoulder arthroplasty depending on implant configuration and scapula neck anatomy
Tomas Smith1, Alexandra Bäunker1, Manuel Krämer2, Christof Hurschler2, Melena Kaufmann1, Marc Frederic Pastor1, Mathias Wellmann PhD 1
1 Department of Shoulder-, Knee- and Sports-Orthopaedics, Hannover Medical School, Anna von Borries Street 1-7, 30625 Hannover, Germany
2 Laboratory of Biomechanics and Biomaterials, Hannover Medical School, Anna von Borries Street 1-7, 30625 Hannover, Germany
Correspondence Address:
Mathias Wellmann
Department of Shoulder-, Knee- and Sports-Orthopaedics, Hannover Medical School, Anna von Borries Street 1-7, 30625 Hannover
Germany
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.167932
 |
|
|
|
| Date of Web Publication | 22-Oct-2015 |
 Abstract Abstract | | |
Purpose: The presence of inferior scapula notching is significantly affected by the anatomy the scapula and can be influenced by the glenosphere design and position and the onlay type.
Materials and Methods: A biomechanical study was undertaken with 13 human shoulder specimens in a robot-assisted shoulder simulator. Inferior scapula contact during adduction of the humerus was detected using a contact pressure film. Computed tomography scans with three-dimensional reconstructions of each specimen were performed.
Results: The greatest improvement of the scapula notching angle (SNA) was achieved by simultaneous implantation of a shallow humeral onlay and an eccentric glenosphere design: 16.3-19.0° (P < 0.005). The SNA was significantly decreased by 5.8° when shifting from a 38 mm centric glenosphere to a 42 mm centric glenosphere (P < 0.005) and by 8.9° comparing the 38 mm centric glenosphere with 38 mm eccentric glenosphere (P < 0.005). The solitary implantation of a shallow onlay significantly decreased the SNA depending on the glenosphere size between 7.4° and 8.0° (P = 0.001). A more inferior position of the metaglene as well as a long scapula neck (P = 0.029) and a large lateral scapula pillar angle (P = 0.033) were correlated with a lower SNA.
Conclusion: This study demonstrates the importance of inferior glenosphere placement and the benefit of eccentric glenosphere and shallow humeral cup design to reduce the adduction deficit of the reverse shoulder. The presence of a short neck of the scapula can have a negative prognostic effect on inferior impingement during adduction of the arm.
Level of Evidence: Basic Science Study
Keywords: Adduction angle, biomechanics, implant configuration, reverse shoulder arthroplasty, scapula anatomy, scapula notching
How to cite this article:
Smith T, Bäunker A, Krämer M, Hurschler C, Kaufmann M, Pastor MF, Wellmann M. Biomechanical evaluation of inferior scapula notching of reverse shoulder arthroplasty depending on implant configuration and scapula neck anatomy. Int J Shoulder Surg 2015;9:103-9 |
How to cite this URL:
Smith T, Bäunker A, Krämer M, Hurschler C, Kaufmann M, Pastor MF, Wellmann M. Biomechanical evaluation of inferior scapula notching of reverse shoulder arthroplasty depending on implant configuration and scapula neck anatomy. Int J Shoulder Surg [serial online] 2015 [cited 2016 Sep 20];9:103-9. Available from: http://www.internationalshoulderjournal.org/text.asp?2015/9/4/103/167932 |
 Introduction Introduction | |  |
Reverse shoulder arthroplasty has been described as an effective treatment for several pathological conditions of the shoulder, such as cuff tear arthropathy, fracture sequelae, and revision shoulder arthroplasty. [1],[2],[3],[4],[5],[6],[7] However, inferior scapular notching has been a frequently reported complication with an incidence ranging between 44% and 96%. [7],[8],[9] Caused by the reversed implant design concept, inferior impingement occurs between the humeral cup and the scapular neck during adduction of the arm and has been recognized as a mechanical factor of inferior scapular notching. [8],[9] Furthermore, polyethylene wear may create a biologic reaction of the joint with inflammation and local osteolysis [10] and progression of the notch. [11] The clinical impact of inferior scapular notching remains unclear since controversial reports exist on this topic. For example, Werner et al. and Boileau et al. did not observe any influence of notching on clinical parameters. [7],[8] In contrast, Simovitch et al., Sirveaux et al. and Wellmann et al. found inferior Constant score results in the presence of scapular notching. [5],[9],[12]
Clinical studies have shown that an inferior position of the baseplate and glenosphere can reduce the incidence of notching. [8],[13] Furthermore, the effect of implant placement on inferior impingement and adduction deficit has been investigated biomechanically. [8],[14],[15] In concordance with the clinical observations, increased inferior overlap of the glenosphere reduced the adduction deficit. The reduction of the humeral neck-shaft angle and cup depth improved the impingent-free adduction and lateralization of the center of rotation resulted in an overall increased range of motion. [8],[15] de Wilde et al. investigated the influence of the size and position of the glenosphere, the inclination angle of the humeral epiphysis and the depth of the humeral cup on inferior scapular impingement in a two-dimensional (2D) computer model and concluded that increased inferior overhang of the glenosphere reduced the adduction deficit of the reverse prosthesis most effectively. [16] The computerized scapula model in this study was based on an average anatomical shape using the data of 200 scapulae investigated by Middernacht et al. [17]
The purpose of this biomechanical study was not only to investigate the influence of the glenosphere position and implant design features on the inferior contact between the humeral component and the scapula during adduction of the arm. Furthermore, the simultaneous effect of the individual scapular anatomy on this conflict was studied. Our hypothesis was that the size and position of the glenosphere, the humeral cup depth and the anatomy of the scapula had a combined influence on the inferior scapular impingement of the reverse shoulder arthroplasty.
 Materials and Methods Materials and Methods | |  |
Specimen preparation and mounting
Thirteen human cadaveric shoulder specimens with no radiographic evidence of glenohumeral osteoarthritis or cuff tear arthropathy were obtained for the study. The mean age of the donors was 70.4 ± 14 years. Prior to the preparation and biomechanical testing, all specimens were evaluated by computed tomography (CT) scans defining different parameters of scapula anatomy. Only shoulders without any signs of fracture sequelae were included. None of the specimens had a pathologic glenoid retroversion (>25°) or a significant posterior subluxation of the humeral head. For further fixation of the shoulders in the testing apparatus, the soft tissue of the medial scapula margin to the scapula neck was dissected leaving the lateral portion of the rotator cuff muscles and the musculotendinous junction intact.
The specimens were then mounted in the testing apparatus. Briefly, the scapula was potted in a custom made box using a two-component polyurethane casting resin (UREOL FC 53, Vantico GmbH, Wehr, Germany). Afterward, the scapula block was rigidly attached to the mounting tower using three threaded rods. Neutral rotation of the humerus was defined by placing a K-wire in the humerus shaft, which was aligned to the axis of the forearm. The humerus was then transected approximately 20 cm distal to the center of the humeral head and potted in a brass cylinder.
The humeral and global coordinate system were defined as previously described. [18] At the time, the humeral head was centered in the glenoid the geometric center of the humeral head was defined to be zero point to measure anterior-posterior and superior-inferior translations. This zero point was saved for each specimen in the intact condition and re-established by the robot at the beginning of every following test condition.
Testing setup
The setup consists of a guided industrial robot (Kuka GmbH, Augsburg, Germany), outfitted with a six-component force-moment sensor (FMS) (IpeA, GmbH, Berlin, Germany) to which the humerus is attached. The robot applies controlled motion and loading to the glenohumeral joint [Figure 1]a. Thereby the scapula is fixed to the mounting tower. The scapula is first aligned to the tower by placing the metaglene of the prosthesis exactly in the vertical plane. The specimens were adjusted by inserting a threaded rod in the central drill hole of the glenosphere. The direction of the rod was then brought into line with the horizontal axis using a water level bubble.
The robot is able to control motion by means of specially written control software and by the load and moment data provided by the FMS. In the current study, a load controlled algorithm was utilized, the robot/FMS system enables measurement of motion with a resolution of 0.02 mm and measurement of joint loading with a resolution of <0.3 N force.
For implantation of the reverse prosthesis (Delta Xtend, DePuySynthes) an extended deltopectoral approach was used. Thereby the subscapularis tendon, supraspinatus tendon, and infraspinatus tendon were dissected in the course of soft tissue preparation. Further, the pectoralis major tendon was released at the proximal 1/3 of its humeral insertion, and the long head of the triceps was released from the inferior scapula neck. The aim of the extensive soft tissue preparation was to get a clear view on the scapula neck for visual control of the testing procedure.
The resection of the humeral head was performed with an inclination of 155° and with neutral version (aligned to the K-wire placed in the humeral head collinear with forearm axis) using a cutting guide. The humeral implant was implanted in a cemented fashion. The preparation of the glenoid included a circumferential release of the glenoid labrum and a dissection of the remaining joint capsule to achieve a clear view of the entire glenoid fossa. The central peg of the metaglene was then placed at the center of the inferior circle of the glenoid so that its border followed the inferior edge of the glenoid. Before fixation of the metaglene, a contact pressure film was interposed between the glenoid and the metaglene surface completely covering the inferior scapula neck (Tekscan 5051, Tekscan, Inc., South Boston, MA) [Figure 1]a. The film was fixed by compression screw fixation of the metaglene. After fixation of the Tekscan-film pressure measurements were reset to zero. The measurement range of the Tekscan-film is given with 50 pounds force per square inch (psi), and the resolution is defined by a number of 62 pressure sensors/cm 2 .
Testing protocol
Serial testing of the specimens was performed using a 38 and 42 mm glenosphere in a centric and an eccentric (inferior overlap) design. The testing sequence was set to be: 38 mm centric, 42 mm centric, 38 mm eccentric, 42 mm eccentric. Further, each type of glenosphere was tested using a standard humeral onlay first and using a more shallow onlay (high mobility onlay) in a second step.
The starting position was defined to be 30° of glenohumeral abduction in the neutral rotation of the arm. In this position, the joint was centered applying 20 N of axial compression and 20 N of lateral compression to the arm. In this position, the center of rotation of the shoulder was defined for each test condition using an algorithm published before. During the testing procedure, the arm of the specimen was adducted by the robot in the scapular plane with an angular velocity of 0.2°/s. The arm movement was operated under force control with a maximum moment of 3 Nm to avoid structural damage to the joint.
Thereby the contact force measured at the scapula neck was simultaneously monitored. With the appearance of contact pressure higher than 5 N/cm 2 (7,25 psi) the movement of the robot was stopped, and the scapula notching angle (SNA) was measured [Figure 1]b. The angle was defined to be positive if the arm was measured to be in an abduction position and it was defined to be negative, if the arm was measured to be in an adduction position. The threshold of 5 N/cm 2 for the contact pressure measurements was defined during pretests to reflect an impingement of the prosthesis with scapula neck and to exclude any bias by soft tissue interposition. All contact pressure measurements were double checked visually. Each condition was tested twice to determine the average adduction angle of both tests.
Computed tomography scans
Computed tomography scans of the specimens were performed before and after reverse shoulder arthroplasty and biomechanical testing. The CT scans before implantation of the prosthesis were performed to exclude specimens with pathologic glenoid retroversion, pathologic glenoid inclination and with a significant glenoid defect or severe glenoid erosion. Further, the humeral anatomy was investigated to exclude cases of fracture sequelae. For each specimen, three-dimensional (3D) reconstructions of the glenoid with elimination of the humerus were performed. The following parameters were defined on the postoperative 3D reconstructions: Implantation height of the metaglene: Distance of the inferior aspect of metaglene to the most inferior aspect of the glenoid (V), length of the scapula neck (H), lateral pillar angle (α): Angle between the margo lateralis scapulae and the inferior scapula neck [Figure 2]a and b.
Statistical analysis
Statistical analysis of the data for the intact/vented joint and for all sequential conditions was performed using both unpaired and paired Student's t-tests (SPSS Inc., Chicago, IL, USA). Statistical significance was set at P < 0.05 and corrected for multiple tests.
 Results Results | |  |
We found a significant influence of the glenosphere size on the SNA [Figure 3]. The SNA was decreased by 5.8° when shifting from a 38 mm centric glenosphere to a 42 mm centric glenosphere (P < 0.005). Comparing the 38 mm centric glenosphere with 38 mm eccentric glenosphere, the SNA decreased by 8.9° (P < 0.005). Comparing the 42 mm centric glenosphere with 42 mm eccentric glenosphere, the SNA decreased by 5.2° (P < 0.005). The solitary change of the glenosphere geometry from a standard (centric) to an eccentric design significantly decreased the SNA for each glenosphere size [Figure 4]. The increase was higher for the 38 mm glenosphere compared to the 42 mm glenosphere. The solitary replacement of the standard onlay to the more shallow HMO-onlay significantly decreased the SNA depending on the glenosphere size tested [Figure 5]: 7.7° with a 38 mm centric glenosphere, 7.4° with a 38 mm eccentric glenosphere, 8.2° with a 42 mm centric glenosphere, 8.0° with a 42 mm eccentric glenosphere (P = 0.001). The simultaneous replacement of the onlay (standard to HMO) and the glenosphere from the standard design to the eccentric design resulted in the following improvements (decrease) of the SNA: 16.3 ± 5.8°, shifting from 38 mm centric to 38 mm eccentric glenosphere; 19.0 ± 7.3°, shifting from 32 mm centric to 42 mm eccentric glenosphere [Figure 6]. Regarding the superior-inferior position of the metaglene the SNA was found to significantly correlate with the implantation height of the metaglene [Figure 7]. Thereby a more inferior position of the metaglene was correlated with a lower SNA. The SNA significantly correlated with the scapula neck length (P = 0.029) and with the lateral pillar angle (a) [Figure 8] and [Figure 9]. A long scapula pillar length and a large lateral pillar angle were correlated with a lower SNA.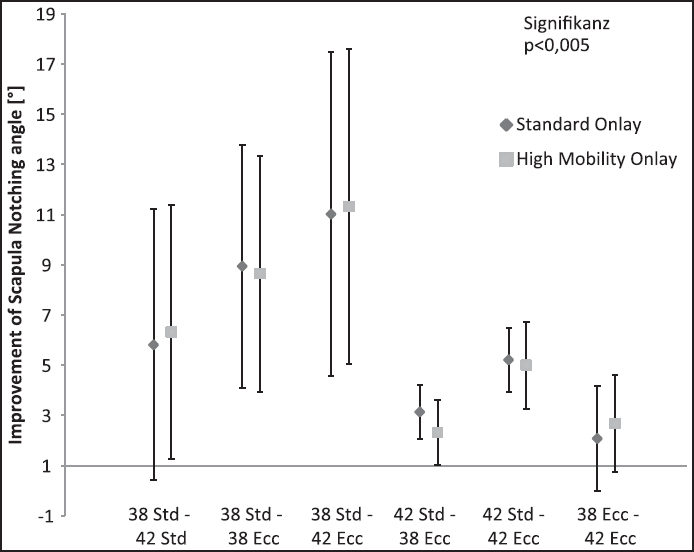 | Figure 3: Improvement of humerus adduction given by the scapula notching angle by changing the glenosphere size. The results are shown for the standard onlay and the more shallow high mobility onlay. Data given as mean and standard deviation. All differences were found to be significant (P < 0.05)
Click here to view |
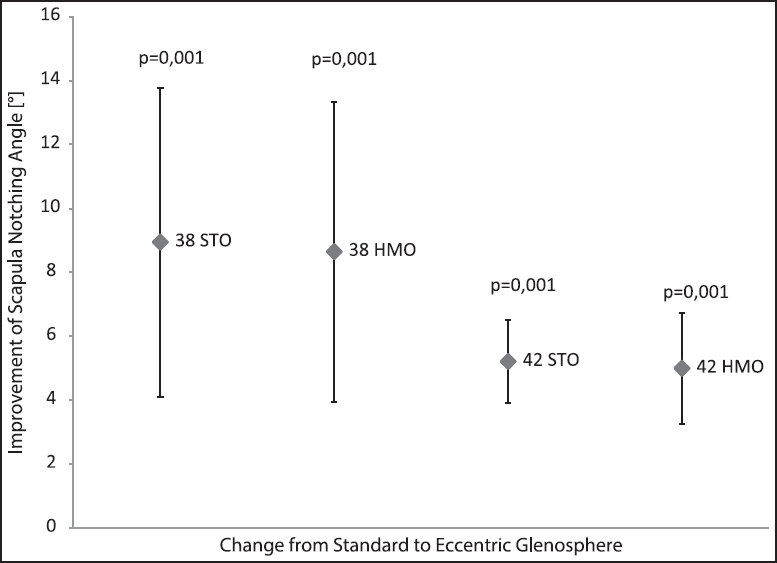 | Figure 4: Improvement of the scapula notching angle by changing the geometry of the glenosphere from a centric to an eccentric design
Click here to view |
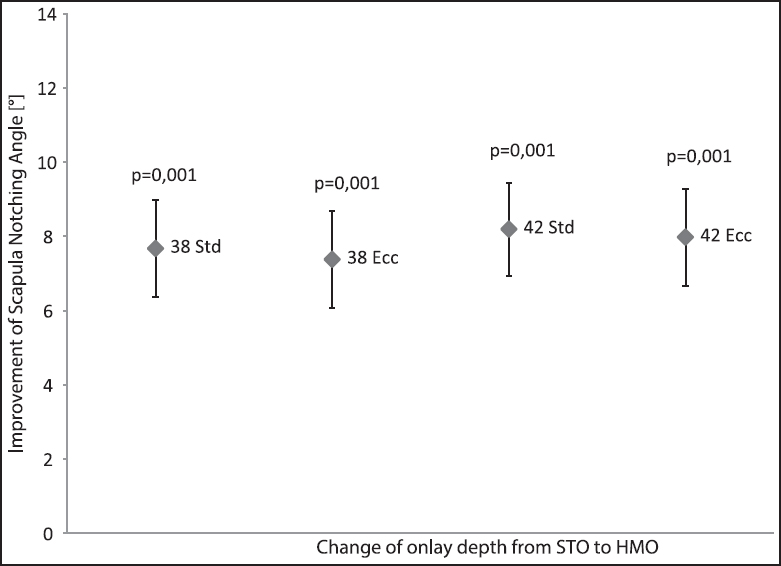 | Figure 5: Improvement of the scapula notching angle by a solitary change from the standard to the high mobility onlay
Click here to view |
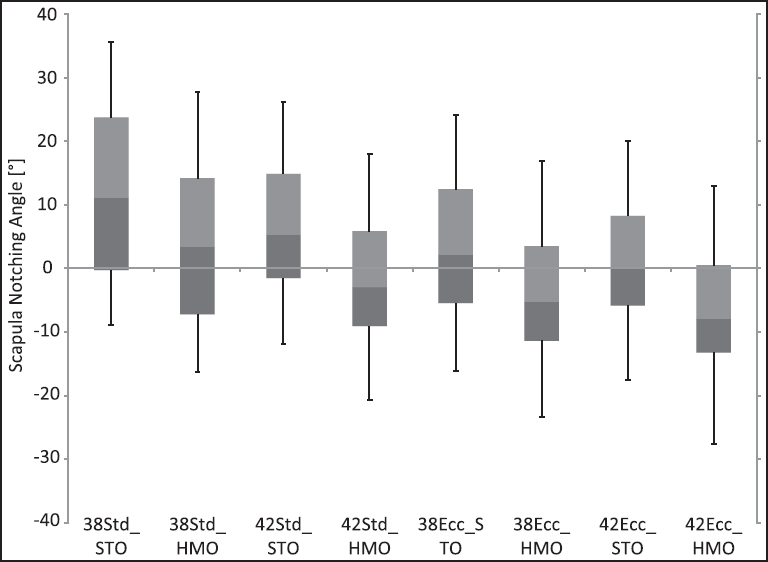 | Figure 6: Scapula notching angle dependent on the glenosphere/onlay combination. Positive values indicate a notching in an abduction position whereas negative values indicate a notching in an adduction position of the humerus. The boxplots display the median, the upper and lower quartile as well as the maximum and minimum value
Click here to view |
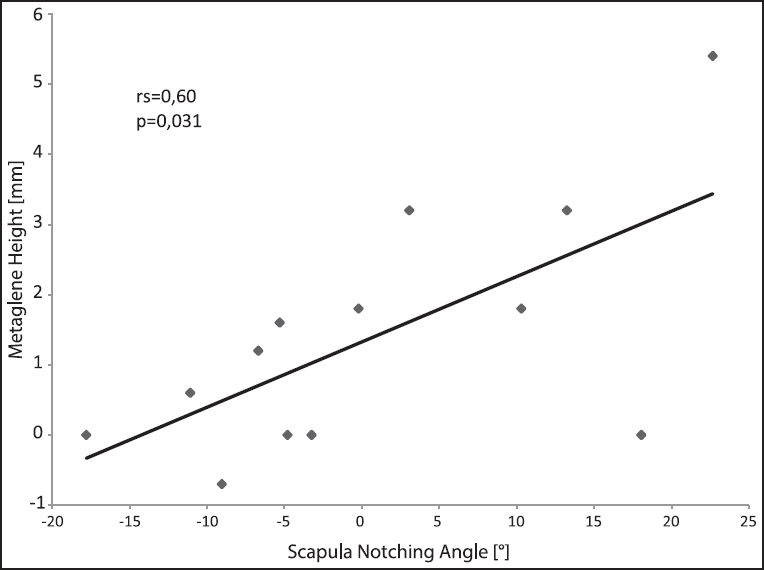 | Figure 7: Correlation of the scapula notching angle with the superior-inferior implantation height of the glenosphere
Click here to view |
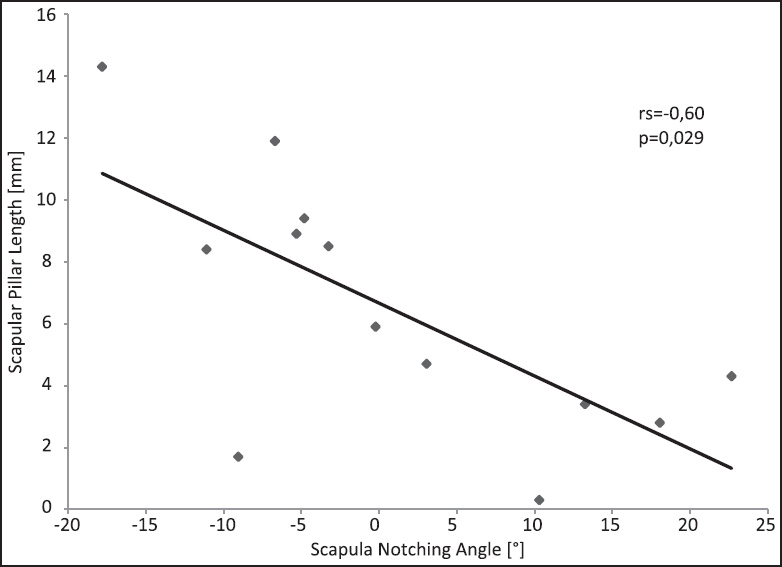 | Figure 8: Correlation of the scapula notching angle with the scapula neck length
Click here to view |
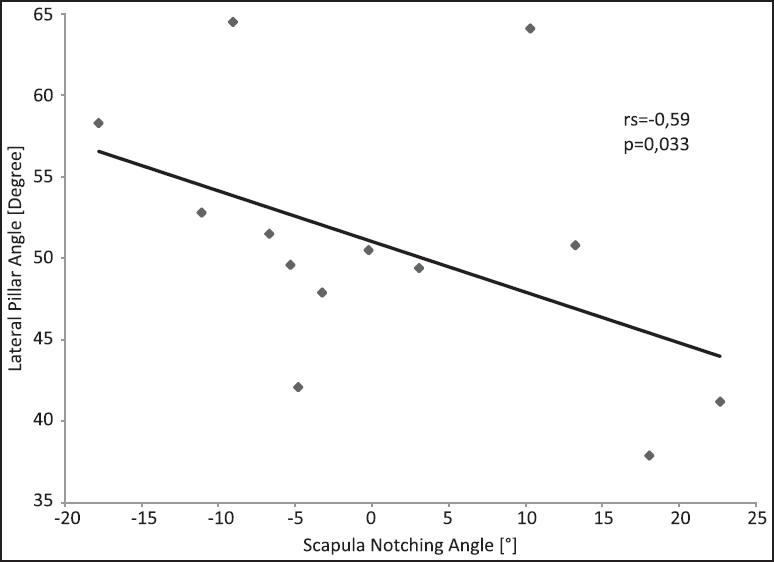 | Figure 9: Correlation of the scapula notching angle with the lateral pillar angle
Click here to view |
 Discussion Discussion | |  |
In our study, an increased inferior overlap of the glenosphere resulted in a reduction of the adduction deficit of the Grammont style reverse Delta Xtend prosthesis. This finding confirms the results of previous biomechanical investigations [15] and the 2D computer model study by de Wilde et al. In accordance, clinical studies have shown a reduced appearance of inferior scapular notching in the presence of an increased inferior overlap of the glenosphere. [8],[9],[13] However, multiple technical strategies exist to achieve an inferior overhang. First, inferior baseplate placement flush to the inferior glenoid rim is an important precondition. Our study has demonstrated a significant increase of the adduction deficit in the case of superior position of the metaglene baseplate. In concordance, previous authors recommended an inferior baseplate placement. [8],[15] Furthermore, a larger diameter of the glenosphere can create pronounced inferior overlap. However, in our study, the selection of a concentric 42 mm diameter implant showed only a small effect on the reduction of the adduction deficit compared to the 38 mm concentric glenosphere, which was previously been shown by Gutiérrez et al. [15] The gain of adduction with the larger diameter implant previously was attributed to increased inferior overlap in the 2D computer model study by de Wilde et al. [16] Another technical option to achieve increased inferior overlap is the selection of an eccentric glenosphere. Our results confirmed this theory and reduced adduction deficits were observed in the presence of eccentric implants. Interestingly, the eccentric 38 mm glenosphere showed better adduction angles than the 42 mm concentric implant, although the design given inferior distance from the central screw to the most inferior rim is identical for both glenospheres. This finding is explained by the smaller humeral diameter of the 38 mm cup compared to the larger 42 mm size, which results in later contact with the scapula during adduction. However, the 42 mm eccentric glenosphere allowed more adduction compared to the 38 mm eccentric glenosphere since the inferior overlap of the size 42 mm implant was 2 mm larger.
Eccentric glenospheres may increase rocking horse forces on the baseplate, potentially leading to implant loosening. [19],[20] This issue has not been investigated in this study, but in our own clinical experience, we have not seen this complication with the glenosphere design used here.
In accordance with the 2D computer model study by de Wilde et al., [16] the reduction of the humeral cup depth resulted in improved adduction angles, regardless the size of glenosphere. However, biomechanically, the increased range of motion with reduced humeral cup depth has the disadvantage of decreased stability, which must be considered in clinical practice. [20],[21],[22]
Regarding a further parameter affecting scapula notching Oh et al. [23] found a significant increase of adduction with decreasing neck-shaft angles of the humeral prosthesis. In a biomechanical setup, the authors found 2° of abduction for a 155° neck-shaft angle, 7° of adduction for a 145° neck-shaft angle and 12° of adduction for a 135° neck-shaft angle. A maximum adduction of 7-12° was achievable using a 42 mm eccentric glenosphere in combination with a shallow onlay.
A further biomechanical cadaver study by Berhouet et al. [24] confirmed an increased size of the glenosphere as well as a lateralization of the center of rotation to result in an improved adduction angle. Moreover, the authors found that inferior scapula contact occurred earliest when the epiphysis was placed in 40° of retroversion and occurred later with 20° and 10° of humeral retroversion. The influence of the scapula neck anatomy was not investigated in this study.
De Wilde et al. [16] described the negative influence of a short horizontal scapular pillar on the adduction deficit of the reverse shoulder arthroplasty in a 2D computer model. In accordance, the length of the horizontal pillar of the scapula showed a significant impact on inferior impingement in our biomechanical study. In the presence of a short scapular pillar length significantly larger adduction deficits were observed. This effect was pronounced when inferior glenosphere overlap was not achieved. Therefore, regarding the notching conflict, lateralization created by the glenosphere implant design or BIO RSA might be beneficial in the presence of a short horizontal pillar of the scapula. [25],[26] Biomechanically, however, lateralized glenosphere implant design may create rocking horse forces, potentially leading to implant loosening. [14],[16],[19],[20],[27] Furthermore, in our study, a small angle between the lateral angulated pillar of the scapula and the vertical plane increased the adduction deficit in the presence of a short horizontal pillar, and lacking inferior overlap of the glenosphere pronounced this effect.
There are limitations to this study. Since only 13 shoulder specimens were investigated, further relevant anatomical variants of the scapula might not have been detected. Furthermore, the investigated scapulae were obtained from healthy shoulders. Glenoid bone loss and humeral pathologies, such as osteophytes and deformities could influence the inferior impingement of the reverse shoulder arthroplasty. During our biomechanical investigation, the scapula was placed in a fixed position. Therefore, this model could not investigate the influence of the natural scapulothoracic motion and scapular tilt. Furthermore, the position of the scapula on the thorax and muscle loading forces of the deltoid and rotator cuff muscles might influence the inferior impingement. Our model did not consider the effect of glenosphere tilt in the coronal and horizontal plane. In the present study, the humeral component was implanted in 0° of retroversion in order to standardize the protocol, modification of the humeral version might influence inferior scapular impingement. Furthermore, one single Grammont style reverse shoulder implant was investigated. Other company specific design modifications are likely to influence inferior scapular impingement.
However, our study confirms the importance of inferior placement of the glenosphere to decrease the adduction deficit of the reverse shoulder arthroplasty previously described in the literature. Furthermore, critical preoperative radiological analysis of the scapular anatomy and good intraoperative exposure of the horizontal pillar of the scapula can be helpful to prevent inferior scapular impingement.
 Conclusion Conclusion | |  |
This study demonstrates the importance of inferior glenosphere placement to decrease inferior scapular impingement of the reverse shoulder arthroplasty. Furthermore, eccentric glenosphere and shallow humeral cup design can reduce the adduction deficit. The presence of a short horizontal pillar of the scapula can have a negative prognostic effect on inferior impingement during adduction of the arm.
Financial support and sponsorship
Nil.
Conflicts of interest
The study was funded by DePuy Synthes.
 References References | |  |
| 1. | Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am 2005;87:1697-705.  |
| 2. | Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am 2006;88:1742-7.  |
| 3. | Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am 2007;89:292-300.  |
| 4. | Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br 2007;89:189-95.  |
| 5. | Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 2004;86:388-95.  |
| 6. | Wall B, Nové-Josserand L, O′Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: A review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85.  |
| 7. | Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005;87:1476-86.  |
| 8. | Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: Design, rationale, and biomechanics. J Shoulder Elbow Surg 2005;14 1 Suppl S:147S-61.  |
| 9. | Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the delta III reverse total shoulder replacement. J Bone Joint Surg Am 2007;89:588-600.  |
| 10. | Nyffeler RW, Werner CM, Simmen BR, Gerber C. Analysis of a retrieved delta III total shoulder prosthesis. J Bone Joint Surg Br 2004;86:1187-91.  |
| 11. | Vanhove B, Beugnies A. Grammont′s reverse shoulder prosthesis for rotator cuff arthropathy. A retrospective study of 32 cases. Acta Orthop Belg 2004;70:219-25.  |
| 12. | Wellmann M, Struck M, Pastor MF, Gettmann A, Windhagen H, Smith T. Short and midterm results of reverse shoulder arthroplasty according to the preoperative etiology. Arch Orthop Trauma Surg 2013;133:463-71.  |
| 13. | Levigne C, Boileau P, Farvard L, Garaud P, Mole D, Sirveaux F, et al. Scapular notching in reverse shoulder arthroplasty. In: Reverse shoulder arthroplasty: Clinical Results, Complications, Revision. Montpellier: Sauramps medical, 2006; 353-72.  |
| 14. | Gutiérrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE 3 rd . Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg 2007;16 3 Suppl:S9-S12.  |
| 15. | Gutiérrez S, Levy JC, Frankle MA, Cuff D, Keller TS, Pupello DR, et al. Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elbow Surg 2008;17:608-15.  |
| 16. | de Wilde LF, Poncet D, Middernacht B, Ekelund A. Prosthetic overhang is the most effective way to prevent scapular conflict in a reverse total shoulder prosthesis. Acta Orthop 2010;81:719-26.  |
| 17. | Middernacht B, De Roo PJ, Van Maele G, De Wilde LF. Consequences of scapular anatomy for reversed total shoulder arthroplasty. Clin Orthop Relat Res 2008;466:1410-8.  |
| 18. | Wellmann M, Petersen W, Zantop T, Herbort M, Kobbe P, Raschke MJ, et al. Open shoulder repair of osseous glenoid defects: Biomechanical effectiveness of the Latarjet procedure versus a contoured structural bone graft. Am J Sports Med 2009;37:87-94.  |
| 19. | De Wilde LF, Audenaert EA, Berghs BM. Shoulder prostheses treating cuff tear arthropathy: A comparative biomechanical study. J Orthop Res 2004;22:1222-30.  |
| 20. | Roche C, Flurin PH, Wright T, Crosby LA, Mauldin M, Zuckerman JD. An evaluation of the relationships between reverse shoulder design parameters and range of motion, impingement, and stability. J Shoulder Elbow Surg 2009;18:734-41.  |
| 21. | Gerber C, Pennington SD, Nyffeler RW. Reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2009;17:284-95.  |
| 22. | Gutiérrez S, Keller TS, Levy JC, Lee WE 3 rd , Luo ZP. Hierarchy of stability factors in reverse shoulder arthroplasty. Clin Orthop Relat Res 2008;466:670-6.  |
| 23. | Oh JH, Shin SJ, McGarry MH, Scott JH, Heckmann N, Lee TQ. Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:1091-8.  |
| 24. | Berhouet J, Garaud P, Favard L. Evaluation of the role of glenosphere design and humeral component retroversion in avoiding scapular notching during reverse shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:151-8.  |
| 25. | Chou J, Malak SF, Anderson IA, Astley T, Poon PC. Biomechanical evaluation of different designs of glenospheres in the SMR reverse total shoulder prosthesis: Range of motion and risk of scapular notching. J Shoulder Elbow Surg 2009;18:354-9.  |
| 26. | Kalouche I, Sevivas N, Wahegaonker A, Sauzieres P, Katz D, Valenti P. Reverse shoulder arthroplasty: Does reduced medialisation improve radiological and clinical results? Acta Orthop Belg 2009;75:158-66.  |
| 27. | Harman M, Frankle M, Vasey M, Banks S. Initial glenoid component fixation in "reverse" total shoulder arthroplasty: A biomechanical evaluation. J Shoulder Elbow Surg 2005;14 1 Suppl S:162S-7.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9]
|
