| |


 |
| Year : 2016 | Volume
: 10
| Issue : 1 | Page : 37-40 |
|
|
|
|
|
CASE REPORT Type IV acromioclavicular joint dislocation associated with a mid-shaft clavicle malunion
Khalid D Mohammed, Danielle Stachiw, Alex A Malone
Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch Hospital, Christchurch, 8140, NewZealand
Correspondence Address:
Khalid D Mohammed
Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch Hospital, PO Box 4345, Christchurch 8140
NewZealand
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/0973-6042.174518
 |
|
|
|
| Date of Web Publication | 20-Jan-2016 |
 Abstract Abstract | | |
This reports presents the case of a combined clavicle fracture malunion and chronic Type IV acromioclavicular (AC) joint dislocation. The patient was seen acutely in the emergency department following a mountain bike accident at which time the clavicle fracture was identified and managed conservatively however the AC dislocation was not diagnosed. The patient presented 25 months following the injury with persistent pain and disability and was treated with clavicle osteotomy and AC stabilization. We document the clinical details, surgical treatment and outcome.
Keywords: Acromioclavicular joint dislocations, athletic injuries, osteotomy, shoulder fractures malunited
How to cite this article:
Mohammed KD, Stachiw D, Malone AA. Type IV acromioclavicular joint dislocation associated with a mid-shaft clavicle malunion. Int J Shoulder Surg 2016;10:37-40 |
 Introduction Introduction | |  |
Controversy exists regarding the optimal treatment of both clavicle fractures and of acromioclavicular (AC) joint dislocations. Clavicle fractures combined with AC dislocations are uncommon with sporadic case reports in the literature outlining the acute management of these cases. [1],[2],[3],[4],[5],[6],[7],[8] Guidelines for the management of combined injuries are not well defined. We describe a case of malunion of the clavicle with chronic type IV AC dislocation (Rockwood classification) treated with clavicle osteotomy and AC stabilization surgery. To our knowledge, this is the first case of chronic combined clavicle malunion and AC joint dislocation described. We document the clinical details, surgical treatment, and outcome. The patient was informed that the case was being submitted for publication, and written consent was obtained.
 Case Report Case Report | |  |
A 33-year-old right hand dominant manager sustained a left clavicle fracture and AC injury in a mountain bike accident. The accident involved him falling forward over the handlebars of his mountain bike onto the anterosuperior aspect of his left shoulder. He was seen in an emergency clinic, where the clavicle fracture was diagnosed with an anteroposterior (AP) X-ray. The X-ray demonstrated a clavicle fracture with mild displacement and some widening of the AC joint [Figure 1]. No orthogonal views were obtained and, to our knowledge, the AC joint injury was not diagnosed. He was treated conservatively with a sling. His fracture healed, but he had ongoing AC joint symptoms. He presented to our clinic 25 months postinjury. He was unable to participate in his recreational sports including rock climbing, kayaking, and mountain biking because of shoulder symptoms. These activities were important to him, and he wanted to be able to resume these activities, if possible. He was experiencing pain in the AC joint region and left trapezius region, above the scapular. He could not lie on his affected side. He described pain with attempted overhead activity and was aware that the clavicle moved posteriorly, accompanied by pain, when he brought his arm across his body. He stated that he was aware of the altered posture of his shoulder, and this troubled him. His visual analogue pain score (VAS) was 1/10 at rest, and American shoulder elbow score (ASES) was 69/100. He was an otherwise healthy man and a nonsmoker.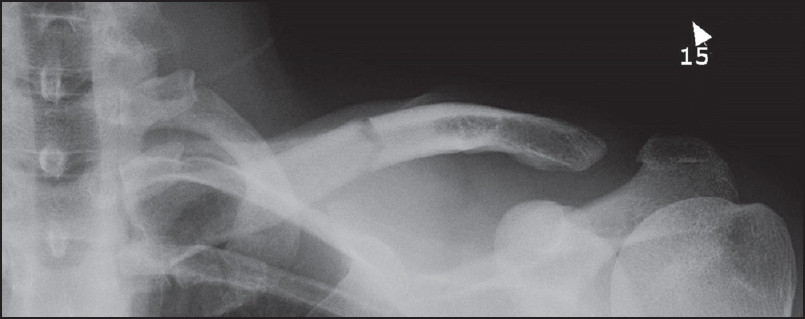 | Figure 1: Anteroposterior X-ray of left clavicle taken at time of injury showing mid-shaft clavicle fracture and widening of the acromioclavicular joint
Click here to view |
On examination, he had a bowed, anteriorly prominent appearance of the middle third of his clavicle with the lateral aspect of the clavicle displaced posteriorly consistent with type IV dislocation of the AC joint [Figure 2]. The AC joint was tender to palpation and translated further posteriorly with cross body flexion. The AC joint was stable to stressing in the vertical plane. Shoulder examination was otherwise normal. We obtained computed tomography scans of both clavicles and AC joints with three-dimensional reconstructions to further define the pathoanatomy. These demonstrated malunion of the clavicle with anterior bowing, and type IV dislocation of the AC joint [Figure 3]. There were no radiological features of distal clavicle osteolysis or arthrosis. | Figure 2: Appearance of the clavicle and type IV acromioclavicular dislocation prior to surgery
Click here to view |
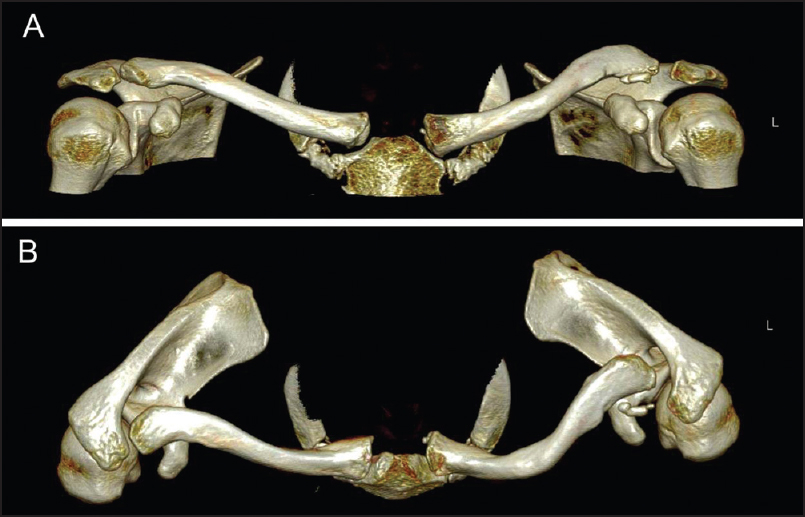 | Figure 3: Preoperative computed tomography anterior (a) and superior (b) three-dimensional views showing marked anterior bowing of the L mid-clavicle and posterior dislocation of the acromioclavicular joint with a well-defi ned ossicle at the anterior aspect of the lateral clavicle
Click here to view |
We diagnosed chronic, symptomatic left shoulder grade IV AC joint instability in the context of clavicle malunion. We discussed the case with national and international shoulder surgeons and searched the literature, but were unable to find any previous experience with this diagnosis. We felt it was unlikely the patient would improve further and be able to participate in his preferred recreations without surgical treatment and offered the patient surgery, with clavicle osteotomy and internal fixation of the clavicle, and AC joint stabilization with a synthetic coracoclavicular sling Surgilig™ AC ligament (Surgicraft, England). Our rationale was the Surgilig™ device would correct the posterior instability of the lateral clavicle but that the clavicle osteotomy was required to correct the malunion of the clavicle in the sagittal plane and prevent excessive anterior prominence of the medial clavicle and subsequent increased stresses on the sternoclavicular joint. The patient was advised of the risks of surgery including that the outcome was uncertain, given this was uncommon injury and treatment. Other risks included nonunion of the osteotomy and the general risks of surgery. The patient elected for surgery.
Surgical technique
The patient was positioned semi-inclined in the beach chair position. Examination under anesthesia demonstrated full shoulder range of motion and glenohumeral stability. The clavicle rested in a posteriorly displaced position and could be translated anteriorly. There was no vertical instability of the AC joint.
Two incisions were used, one for the clavicle osteotomy and one for the AC stabilization. An incision was made over the middle third of the clavicle to perform the clavicular osteotomy. A precontoured 6-hole LCP 3.5 mm Reconstruction Plate (DuPuy Synthes Trauma, Pennsylvania, USA) was used as a guide to estimate the location and amount of the anterior wedge resection osteotomy. The plate was temporarily applied laterally, and the osteotomy site estimated and marked. The plate was then removed and the anterior wedge resection osteotomy performed with an oscillating saw. The closing wedge osteotomy was then fixed with the 6-hole contoured reconstruction plate with locking screws as this could be made to fit better than the precontoured clavicle plate. The bone adjacent to the osteotomy was petalled, and local bone graft from the wedge osteotomy was morcellized and placed around the osteotomy.
A vertical strap incision was made that was centered over the coracoid extending to the AC joint for the AC joint reconstruction. The AC joint reconstruction was performed with the Surgilig™ implant device in accordance with the manufacturer's surgical technique. The distal clavicle was exposed, and the anterolateral aspect of the clavicle was minimally trimmed. The curved introducer was passed around the base of the coracoid from medial to lateral. The length gauge was passed and tightened around the coracoid and brought over the posterior edge of the clavicle to the planned position of the screw with the clavicle in a reduced position. An 11 mm graft was chosen. Using the length gauge, the Surgilig™ implant was passed around the coracoid and secured at its base as described in the surgical technique. The implant was brought up posterior to the clavicle at the region of the conoid ligament insertion (lateral to the reconstruction plate) and secured to the anterior clavicle with one 3.5 mm cortical screw and washer. This reduced the distal clavicle effectively. Local bone graft from the distal clavicle was placed underneath the clavicle in the region of the Surgilig™ surgical mesh to encourage biological healing in the region of the synthetic graft.
Fluoroscopy was used to confirm good osteotomy reduction, AC joint reduction, and the placement of hardware. The wounds were closed in a routine manner. Postoperatively, he was in a sling for 6 weeks. Pendulum exercises started at 2 weeks postoperatively. At 6 weeks, range of motion exercises were started followed by a gradual increase in strengthening. The patient had postoperative and follow-up X-rays [Figure 4].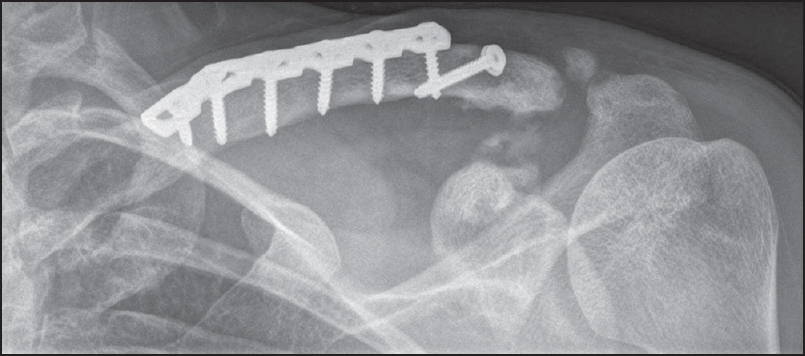 | Figure 4: X-ray at 6 months postoperatively showing union of the clavicle osteotomy, satisfactory position of the acromioclavicular joint with some coracoclavicular ossifi cation
Click here to view |
 Results Results | |  |
Final follow-up was 22 months postoperatively at which time the patient reported no pain and was able to participate fully in his recreational activities including advanced rock climbing, where he is required to suspend and swing his entire body weight through the affected arm. The appearance of his clavicle and AC joint was symmetrical with the other side [Figure 5]. The shoulder range of movement was normal and equal to his other side [Figure 6] and his AC joint was nontender and clinically stable. X-rays were taken, 6 months following surgery and these demonstrated union of the osteotomy and satisfactory appearance of the AC joint [Figure 4]. | Figure 5: Symmetrical postoperative appearance of the clavicle and acromioclavicular joint
Click here to view |
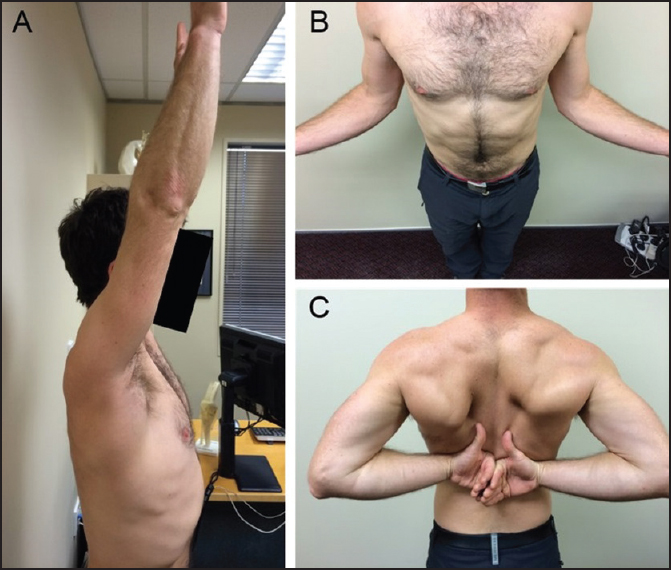 | Figure 6: Range of motion at 22 months postoperatively: (a) Elevation, (b) external rotation, and (c) internal rotation
Click here to view |
The patient's ASES score improved from 69/100 preoperatively to 100/100. His VAS score was 0/10, Oxford Shoulder Score 48/48, and Constant Score 93/100 (subjective 34/35 and objective 59/65).
 Discussion Discussion | |  |
We consider there to be a number of learning points from this case. Concurrent AC joint injury may occur with a clavicle fracture, and clinical and radiological assessment is required, if suspicious of this combined injury. Type IV injury may be present as reported in other case reports, [6],[8] and AP X-rays may not clearly show a type IV injury. If there is clinical suspicion of AC joint injury, axillary X-ray views should be obtained at presentation or soon after. This injury can be treated late with osteotomy and AC reconstruction, as we have described, but acute surgical management of the clavicle fracture may be preferable if a significant combined injury is recognized.
We found the temporary application of a precontoured clavicle plate useful as a guide for the location and amount of anterior wedge resection osteotomy. Care should be taken to preserve vascularity of the clavicle with minimal soft tissue stripping and cooling of the bone ends with irrigation during osteotomy with an oscillating saw.
The Surgilig™ device does tend to bring the outer end of clavicle forward, which was an advantage, in this case, where we were aiming to correct posterior displacement. The treatment, we have outlined was successful in improving high-demand overhead function in this patient, and we recommend it is considered as an option if other surgeons encounter this unusual combination of injuries.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/ their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Beytemür O, Adanir O, Dinçel YM, Baran MA, Güleç MA. Clavicle diaphyseal fracture, ipsilateral type 3 acromioclavicular joint dislocation stabilized with double plate. Int J Shoulder Surg 2013;7:153-4.  |
| 2. | Heinz WM, Misamore GW. Mid-shaft fracture of the clavicle with grade III acromioclavicular separation. J Shoulder Elbow Surg 1995;4:141-2.  |
| 3. | Juhn MS, Simonian PT. Type VI acromioclavicular separation with middle-third clavicle fracture in an ice hockey player. Clin J Sport Med 2002;12:315-7.  |
| 4. | Lancourt JE. Acromioclavicular dislocation with adjacent clavicular fracture in a horseback rider. A case report. Am J Sports Med 1990;18:321-2.  |
| 5. | Psarakis SA, Savvidou OD, Voyaki SM, Beltsios M, Kouvaras JN. A rare injury of ipsilateral mid-third clavicle fracture with acromioclavicular joint dislocation. Hand (N Y) 2011;6:228-32.  |
| 6. | Woolf SK, Valentine BJ, Barfield WR, Hartsock LA. Middle-third clavicle fracture with associated type IV acromioclavicular separation: Case report and literature review. J Surg Orthop Adv 2013;22:183-6.  |
| 7. | Wurtz LD, Lyons FA, Rockwood CA Jr. Fracture of the middle third of the clavicle and dislocation of the acromioclavicular joint. A report of four cases. J Bone Joint Surg Am 1992;74:133-7.  |
| 8. | Yeh PC, Miller SR, Cunningham JG, Sethi PM. Midshaft clavicle fracture and acromioclavicular dislocation: A case report of a rare injury. J Shoulder Elbow Surg 2009;18:e1-4.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6]
|
