| |


 |
| Year : 2016 | Volume
: 10
| Issue : 2 | Page : 89-91 |
|
|
|
|
|
CASE REPORT Osteochondritis dissecans on the medial aspect of the humeral head
Yuichiro Mima1, Noboru Matsumura2, Kiyohisa Ogawa3, Takuji Iwamoto1, Kensuke Ochi1, Kazuki Sato1, Yoshiaki Toyama1
1 Department of Orthopedic Surgery, Keio University School of Medicine, Tokyo, Japan
2 Department of Orthopedic Surgery, Keio University School of Medicine, Tokyo; Department of Orthopedic Surgery, Saiseikai Utsunomiya Hospital, Utsunomiya, Japan
3 Department of Orthopedic Surgery, Saiseikai Utsunomiya Hospital, Utsunomiya; Department of Orthopedic Surgery, Eiju General Hospital, Tokyo, Japan
Correspondence Address:
Noboru Matsumura
Department of Orthopedic Surgery, Keio University School of Medicine, 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582
Japan
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/0973-6042.180722
 |
|
|
|
| Date of Web Publication | 20-Apr-2016 |
 Abstract Abstract | | |
The case of a 29-year-old man who had osteochondritis dissecans on the medial aspect of the humeral head is reported. Repetitive micro-trauma at a low elevated arm position was thought to have induced the osteochondral lesion.
Keywords: Humeral head, osteochondral lesion, osteochondritis dissecans
How to cite this article:
Mima Y, Matsumura N, Ogawa K, Iwamoto T, Ochi K, Sato K, Toyama Y. Osteochondritis dissecans on the medial aspect of the humeral head. Int J Shoulder Surg 2016;10:89-91 |
 Introduction Introduction | |  |
Osteochondritis dissecans (OCD) occurs rarely in the humeral head [1],[2],[3],[4],[5],[6],[7],[8],[9],[10],[11],[12] and OCD on the medial aspect of the humeral head has never been reported. A case with OCD on the medial aspect of the humeral head where it contacted the glenoid surface in the hanging arm position is described. Fixation of the osteochondral fragment with poly-L-lactic acid pins led to a good clinical result. The patient was informed that data concerning the case would be submitted for publication, and he consented.
 Case report Case report | |  |
A right-hand-dominant 29-year-old man was employed in a car repair shop and was assigned the work of tightening screws of tires using torque wrenches. Three months after starting this work, he felt right shoulder pain during shoulder motion. He changed his job to light labor in the next month and stopped all sports activities. Nevertheless, his shoulder pain lasted for a further 6 months during his daily activities. He visited our department complaining of right shoulder pain 10 months after his first episode. He had no relevant medical history and no history of trauma to the shoulder girdles.
The patient was 168 cm tall and weighed 100 kg. Physical examination showed the absence of swelling and tenderness in his right shoulder, and there was no restriction of range of shoulder motion. However, shoulder pain was induced during shoulder internal rotation in the abducted and flexed shoulder position. Because of the severe pain, he was restricted from sports activities and heavy labor. His American Shoulder and Elbow score was 63.3 points.
Plain radiograms showed a radiolucent lesion on the medial aspect of the right humeral head [Figure 1]a. Computerized tomography (CT) scans also showed the 2-cm lucent lesion in the humeral head surrounded by osteosclerotic changes, whereas its subchondral bone appeared to keep its continuity above the lucent lesion [Figure 1]b. On T2-weighted images of magnetic resonance imaging (MRI), an osteochondral fragment at the medial aspect was separated from the humeral head with the continuation of the articular cartilage [Figure 1]c. The imaging findings were consistent with OCD on the medial aspect of the humeral head.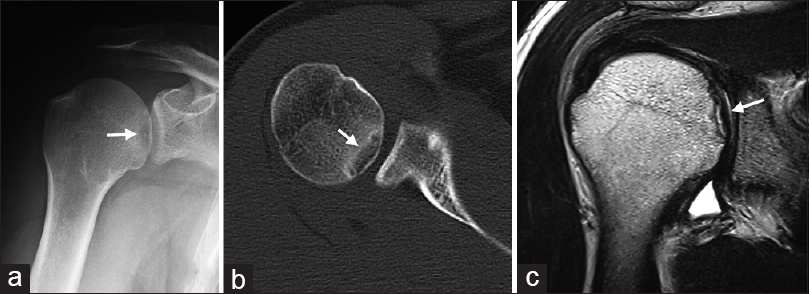 | Figure 1: Preoperative imaging findings. (a) Antero-posterior plain radiogram shows the radiolucent lesion in the medial aspect of the right humeral head (white arrow). (b) Axial computed tomography scans show the 2-cm radiolucent lesion surrounded by osteosclerotic change, whereas the subchondral bone maintains its continuity above the lesion (white arrow). (c) Magnetic resonance imaging shows an osteochondral fragment, which is separated from the humeral head, on T2-weighted images. The articular cartilage maintains its continuity (white arrow)
Click here to view |
Since his symptoms worsened despite the 10-month interval, surgical intervention was selected. Under general anesthesia, arthroscopic examination of the glenohumeral joint was performed in the left lateral decubitus position. Arthroscopic examination from the posterior viewing portal showed a 2-cm osteochondral lesion that could be easily distinguished from the other normal cartilage [Figure 2]a. The lesion was obviously softened compared to the other area, and the 2-cm softened area could be identified as the osteochondral lesion with a careful palpation. The articular cartilage of the lesion maintained its continuity. It was consistent with stage 2 OCD of the International Cartilage Repair Society classification. [13] During shoulder internal rotation in flexion and abduction, which had induced his shoulder pain, the lesion appeared to cause friction with the glenoid surface or anterior capsule. The osteochondral fragment was blindly fixed to the humeral head to preserve the continuity of the articular cartilage. In the internally rotated shoulder position, four absorbable 2-mm-diameter threaded pins made from poly-L-lactic acid (Fixsorb® , DePuy Synthes, Johnson and Johnson, New Brunswick, NJ, USA) were inserted into the center area of the abnormal lesion through the posteroinferior portal [Figure 2]b and c. His right arm was placed into a sling for 2 weeks after the surgery. Two weeks later, he could move his shoulder in daily activities. Since the osteochondral fragment united successfully on radiographic examination, he was allowed to start heavy labor and sports activities from 6 months after surgery. | Figure 2: The arthroscopic findings. (a) The 2-cm osteochondral lesion can be distinguished from the other site, but the articular cartilage of the lesion maintains its continuity with the surrounding cartilage. (b) The lesion is obviously softened compared to the other area. Four absorbable threaded pins are inserted into the center area of the abnormal lesion. (c) The osteochondral fragment is fixed to the humeral head
Click here to view |
At the final follow-up of 4 years after the surgery, he did not feel any shoulder pain during all motions in his activities. The American Shoulder and Elbow score improved from 63.3 preoperatively to 89.2 at the final follow-up. Radiograms and CT scans showed the bone union of the fragment without a radiolucent lesion [Figure 3]a and b. MRI showed that the osteochondral lesion healed with the same intensity as the humeral head [Figure 3]c. | Figure 3: The imaging and arthroscopic findings at final follow-up. (a and b) The anteroposterior plain radiogram and axial computed tomography scan show bony union of the fragment. (c) The osteochondral lesion has healed with the same intensity as the humeral head on T2-weighted images of magnetic resonance imaging
Click here to view |
 Discussion Discussion | |  |
OCD is common in the distal femur, humeral capitulum, and talar dome, but it rarely occurs in the humeral head. Only 12 cases with humeral head OCD have been reported. [1],[2],[3],[4],[5],[6],[7],[8],[9],[10],[11],[12] Most of them occurred in young men in the dominant shoulder. The anterosuperior aspect [4],[9],[10],[11] and the superior aspect [1],[2],[3],[7] of the humeral head were reported as the predominant sites of involvement. However, the medial aspect has never been reported as a site of humeral head OCD.
The etiology of OCD remains controversial. Acute trauma, [14] repetitive micro-trauma, [15],[16] sports activity, [17] ossification abnormality, and genetic factors have been suggested as causes of the pathology. Moreover, the subchondral injury is generally recognized to be provoked with vascular compromise. [17] The blood supply to the humeral head is supposed to be poor in the superior aspect, which is the predominant site of avascular necrosis. [18] The superior aspect of the humeral head would face the glenoid cavity in the elevated arm position, and acute or micro-trauma at that position might increase the mechanical load to the area in the previously reported cases with humeral head OCD. In the present case, however, the patient repeatedly used a tire torque wrench with slight arm abduction from 0° to 30°. With the arm at the side, the medial aspect of the humeral head would face toward the glenoid cavity. Thus, repetitious sheer and rotation stresses to the medial aspect of the humeral head appeared to induce the osteochondral lesion despite the good blood supply in the present case. The present case is the first report of OCD on the medial aspect of the humeral head, but this kind of mechanism is bound to occur frequently. Some cases of OCD on the medial aspect of the humeral head may be missed because of the uncertainty about the radiographic findings and the relatively slight clinical symptoms.
Avascular necrosis of the humeral head, Hill-Sachs lesion, bone bruise, and primary glenohumeral osteoarthritis can be considered in the differential diagnosis of osteochondral lesions. Avascular necrosis is typically caused by trauma, corticosteroid therapy, alcoholism, or systemic diseases. [18] However, the present case did not have these factors, and the affected area was different from the site of humeral head necrosis. Hill-Sachs lesion is defined as an osteochondral defect of the posterolateral aspect of the humeral head following glenohumeral dislocation. [19] Thus, it can be excluded in the present case because of the patient's history and the involved location. A bone bruise shows a similar MRI pattern to that of the present case, but a diffuse high-intensity area on T2-weighted images should be found with a bone bruise. Moreover, nonsurgical treatment usually relieves the symptoms in cases with a bone bruise. [20] Although the location of the lesion was the same as the predominant area of primary glenohumeral osteoarthritis, the present case showed radiographic findings different from osteoarthritis. However, osteochondral lesions could possibly develop to secondary osteoarthritis in the future. [21] Thus, missed OCD on the medial aspect of the humeral head can cause arthritic changes, and there may be cases where it has been regarded as primary glenohumeral arthritis. The present case was finally diagnosed as OCD based on the arthroscopic findings.
In the past literature, humeral head OCD has been treated with rest, curettage, drilling, removal of loose bodies, and allograft transfer. In two past cases, nonoperative treatment was reported to be ineffective, and that additional treatments would be needed. [8],[12] Johnson and Warner stated that curettage was also insufficient, and they performed additional allograft transfer. [6] In the present case, the articular cartilage of the OCD lesion maintained its continuity with the normal area. Thus, the osteochondral lesion was fixed using absorbable poly-L-lactic acid pins. No case with humeral head OCD has been treated with osteosynthesis, but it achieved bone union with a satisfactory clinical result. However, all of the reported treatment options lack long-term results. Since this kind of osteochondral pathology could possibly result in future arthritis, this case requires long-term follow-up.
 Conclusion Conclusion | |  |
A case of OCD on the medial aspect of the humeral head in which fixation of the osteochondral fragment achieved a good clinical result was described. OCD on the medial aspect of the humeral head is rare, but it could develop to secondary glenohumeral arthritis. Thus, long-term follow-up will be needed for the present case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Anderson WJ, Guilford WB. Osteochondritis dissecans of the humeral head. An unusual cause of shoulder pain. Clin Orthop Relat Res 1983;173:166-8.  [ PUBMED] |
| 2. | Debeer P, Brys P. Osteochondritis dissecans of the humeral head: Clinical and radiological findings. Acta Orthop Belg 2005;71:484-8.  |
| 3. | Ganter M, Reichelt A. Osteochondrosis dissecans of the humeral head. Z Orthop Ihre Grenzgeb 1996;134:73-5.  |
| 4. | Hamada S, Hamada M, Nishiue S, Doi T. Osteochondritis dissecans of the humeral head. Arthroscopy 1992;8:132-7.  |
| 5. | Ishikawa H, Ueba Y, Yonezawa T, Kurosaka M, Ohno O, Hirohata K. Osteochondritis dissecans of the shoulder in a tennis player. Am J Sports Med 1988;16:547-50.  |
| 6. | Johnson DL, Warner JJ. Osteochondritis dissecans of the humeral head: Treatment with a matched osteochondral allograft. J Shoulder Elbow Surg 1997;6:160-3.  |
| 7. | Lunden JB, Legrand AB. Osteochondritis dissecans of the humeral head. J Orthop Sports Phys Ther 2012;42:886.  [ PUBMED] |
| 8. | Mahirogullari M, Chloros GD, Wiesler ER, Ferguson C, Poehling GG. Osteochondritis dissecans of the humeral head. Joint Bone Spine 2008;75:226-8.  |
| 9. | Miller LF, Hilkevitch A. Osteochondritis dissecans of the shoulder. Am J Roentgenol Radium Ther 1950;63:223-7.  [ PUBMED] |
| 10. | Park TS, Kim TS, Cho JH. Arthroscopic osteochondral autograft transfer in the treatment of an osteochondral defect of the humeral head: Report of one case. J Shoulder Elbow Surg 2006;15:e31-6.  |
| 11. | Petrini A, Grassi G, Pranzo Zaccaria C. Osteochondritis dissecans of the humeral head. Chir Organi Mov 1984;69:83-5.  [ PUBMED] |
| 12. | Pydisetty RV, Prasad SS, Kaye JC. Osteochondritis dissecans of the humeral head in an amateur boxer. J Shoulder Elbow Surg 2002;11:630-2.  |
| 13. | Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 2003;85-A Suppl 2:58-69.  |
| 14. | Aichroth P. Osteochondritis dissecans of the knee. A clinical survey. J Bone Joint Surg Br 1971;53:440-7.  [ PUBMED] |
| 15. | Fairbank HA. Osteo-chondritis dissecans. Br J Surg 1933;21:67-82.  |
| 16. | Smillie IS. Treatment of osteochondritis dissecans. J Bone Joint Surg Br 1957;39-B:248-60.  [ PUBMED] |
| 17. | Cahill BR. Osteochondritis dissecans of the knee: Treatment of juvenile and adult forms. J Am Acad Orthop Surg 1995;3:237-47.  |
| 18. | Gruson KI, Kwon YW. Atraumatic osteonecrosis of the humeral head. Bull NYU Hosp Jt Dis 2009;67:6-14.  |
| 19. | Hill HA, Sachs MD. The grooved defect of the humeral head: A frequently unrecognized complication of dislocations of the shoulder joint. Radiology 1940;35:690-700.  |
| 20. | Bicknell RT, Cikes A, Boileau P. Humeral head bone bruise in anterior glenohumeral instability: A case report. J Shoulder Elbow Surg 2009;18:e10-3.  |
| 21. | Twyman RS, Desai K, Aichroth PM. Osteochondritis dissecans of the knee. A long-term study. J Bone Joint Surg Br 1991;73:461-4.  |
[Figure 1], [Figure 2], [Figure 3]
|
