|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 1
| Issue : 1 | Page : 20-24 |
|
An observational study of endocrine disorders in HIV infected patients from north India
Nirdesh Jain, Madhukar Mittal, Himanshu Dandu, Shailendra P Verma, Manish Gutch, Anil K Tripathi
Department of Internal Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India
| Date of Acceptance | 12-Jan-2013 |
| Date of Web Publication | 16-Aug-2013 |
Correspondence Address:
Nirdesh Jain
Room no. E/206, Gautam Buddha Hostel, King George Medical University, Lucknow - 226 003, Uttar Pradesh
India
 Source of Support: None, Conflict of Interest: None  | Check |
 
Objective: Human immunodeficiency virus (HIV) infection is known to affect every organ system of the body, either directly or through opportunistic infections. Ours was a cross-sectional study to determine the prevalence of thyroid, adrenal, and gonadal dysfunction in HIV patients and to correlate these with stages of HIV infection, antiretroviral therapy, and with the associated wasting. Design: HIV patients aged ≥15 years were enrolled from July 2009 to June 2010. Each enrolled patient underwent through a thorough clinical evaluation, and questionnaire specifying the endocrine disorders were asked specifically to them. Thyroid function test (T3, T4, and TSH), serum cortisol, serum testosterone, LH, and FSH at 8:00 AM were estimated. Results: A total of 117 (90 males, 27 females) patients with a mean age of 34.10 ± 8.3 years were enrolled. TSH was elevated in 9% from reference cut-off value of 0.25-5.5 mIU/L. Only 2% were overtly hypothyroid because they had symptoms and TSH was >10 mIU/L in them. Serum cortisol could be estimated in 97 patients, of them 5 had definitive adrenal insufficiency (AI) (serum cortisol <100 nmol/l), 54 were indeterminate (100-500 nmol/l), and 38 were excluded for AI (>500 nmol/l). No patient had hypotension. Hypogonadism (serum testosterone <200 ng/dl) was found in 75.7% (28/37) males patients. However, only 27% (10/37) patients complained of impotency. The wasting was evident in 61.53% of the total patients and had positive correlation with only testosterone levels in males (P = 0.864). Conclusions: Hypothyroidism seen in HIV patients was predominantly subclinical. Since we excluded seriously ill patients from the study, sick euthyroid syndrome is unlikely as a cause for the abnormal thyroid function tests. Decreased levels of serum cortisol were found although with unclear clinical significance. HIV infected males had hypogonadism, probably hypogonadotropic. Keywords: Endocrinopathy, hypogonadotropic hypogonadism, HIV/AIDS
How to cite this article:
Jain N, Mittal M, Dandu H, Verma SP, Gutch M, Tripathi AK. An observational study of endocrine disorders in HIV infected patients from north India. J HIV Hum Reprod 2013;1:20-4 |
How to cite this URL:
Jain N, Mittal M, Dandu H, Verma SP, Gutch M, Tripathi AK. An observational study of endocrine disorders in HIV infected patients from north India. J HIV Hum Reprod [serial online] 2013 [cited 2017 Apr 5];1:20-4. Available from: http://www.j-hhr.org/text.asp?2013/1/1/20/116535 |
| Introduction | |  |
Human immunodeficiency virus (HIV) disease is pandemic that has already affected 33.4 million worldwide until 2008. [1] As of 2009, it was estimated that 2.4 million people were living with HIV in India alone. [2] Since antiretroviral therapy (ART) have become widely and easily available and the incidence of opportunistic infections has come down. However, other systemic disorders including endocrine disorders are still not thoroughly evaluated. High incidences of different endocrine are being noted in these patients. [3],[4] Virtually every endocrine gland (adrenal, gonadal, hypothalamus-pituitary, and thyroid) has been reported to be affected in HIV patients at varying rates in different studies. [5],[6]
In the various ways, HIV infection directly or indirectly through opportunistic infections and/or by antiretroviraldrugs can cause endocrine abnormalities. Patients not receiving ART have increased production of inflammatory cytokines due to active disease, AIDS wasting, and the presence of opportunistic infections can all contribute to development of endocrine disorders. With the initiation of treatment, immune reconstitution can precipitate autoimmune diseases such as hyperthyroidism, [7] and a case of autoimmune diabetes has also been reported. [8] The patient's underlying genetic risk and environmental factors (such as over nutrition and sedentary lifestyle) in combination with disease-related risk factors can lead to overt manifestation of latent endocrine disease.
In India, so far very few studies have conducted to understand the profile of endocrine dysfunctions in HIV patients. [9] The present study was undertaken to understand the profile of endocrine disorders, and an effort was also made to correlate these endocrine disorders with stages of HIV disease, ART status, and body mass index (BMI) in HIV patients.
| Material and Methods | |  |
This hospital-based observational study was done over a period of 1 year (July 2009 to June 2010) at tertiary care center of north India. HIV patients aged >15 years who gave informed consent were included. All studied patients were assessed clinically and were subjected to specific questions pertaining to endocrine disorders [Table 1]. All patients were categorized into AIDS and non-AIDS group on the basis of AIDS defining illness as per the WHO classification; ART and ART naïve; and also divided into three groups, i.e., A, B, and C on the basis of baseline CD4 counts <200 cells/mm 3 , 200-350 cells/mm 3 , and >350 cells/mm 3 , respectively. Wasting in HIV patients was considered at BMI <18.5 kg/m 2 .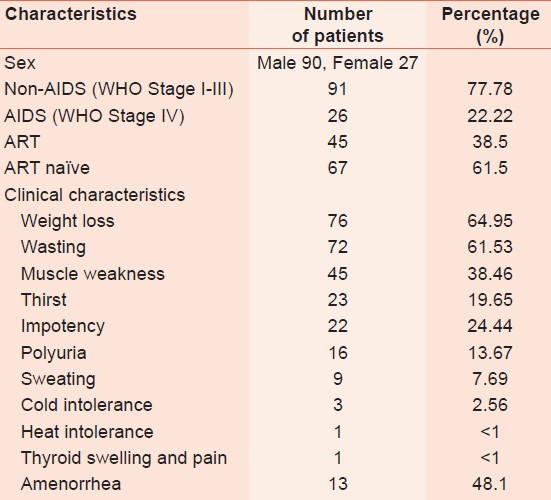 | Table 1: The description of the demographic and clinic characteristics with the frequency of patients
Click here to view |
Laboratory methods
The blood samples for different hormonal profile including thyroid function tests (T3, T4 and TSH), serum cortisol, serum gonadotrophins (LH and FSH), serum testosterone, serum estrogen, and serum progesterone were taken at 8:00 AM to avoid possible interference with circadian rhythms. In seriously ill patients, thyroid function test were not carried out to consider sick euthyroid syndrome. Radioimmunoassay kits were used for estimation of thyroid function tests (supplied by Board of Radiation and Isotope Technology, Mumbai) and serum cortisol, testosterone, LH, and FSH (Immunotech, Beckman Coulter, Inc., Villepinte, France).
Statistical analysis
Data were presented in mean (SD), median, interquartile, and percentage. The Mann-Whitney U test was used for comparison of two means. The comparison of two sequential measurements in the same patient was carried out using the Wilcoxon matched-pairs signed-ranks test. Categorical variables were compared with the chi square test. A stepwise logistic regression analysis was used to identify the independent association of diverse parameters with wasting in HIV disease (BMI). A P value < 0.05 for a two-sided test was considered statistically significant. All analyses were performed with the statistical software Stata, version 11.1 (Stat Corp Inc., College Station, Texas, USA). The study was approved by the ethics committee of our institute.
| Results | |  |
A total of 117 (90 male, 27 female) patients with a mean age of 34.10 ± 8.3 years were studied. The mean BMI was 18.07 ± 2.3 kg/m 2 , and 70 (59.8%) patients had wasting (BMI < 18.5 kg/m 2 ). The median of baseline CD4 cell counts were 207 cells/mm 3 (IQR 106-284 cells/mm 3 ). This study consisted of 75 (64.1%) patients of AIDS and 42 (35.9%) non-AIDS. ART was being used by 45 (38.5%) and they were categorized to ART group and the remaining who were not using ART were categorized to ART-naïve. In ART group, the median duration for which ART being used by subjects 3 months (IQR 2-9.5 months). ART regimens being used were of four types based on the different combination of zidovudine or stavudine with either nevirapine or efavirenz; lamivudine was common in each regimen. Patients in ART-naive group were either newly diagnosed or were those who did not fulfill the NACO criteria [10] for initiation of ART based on WHO clinical staging and CD4 counts.
In relation to endocrine disorders, the most common complaint was weight loss (64.9%), followed by amenorrhea (48.1% female), muscular weakness (38.5%), impotence (22% male HIV patients) [Table 1]. The wasting was evident in 59.8% of the total patients. The frequency of impotence (29.2% vs. 12%, P = 0.15) and amenorrhea (70% vs. 35.2%, P = 0.12) were higher in AIDS than in non-AIDS. Impotency in males (P = 0.16) and amenorrhea in females (P = 0.065) did not have frequent occurrence with HIV wasting [Figure 1].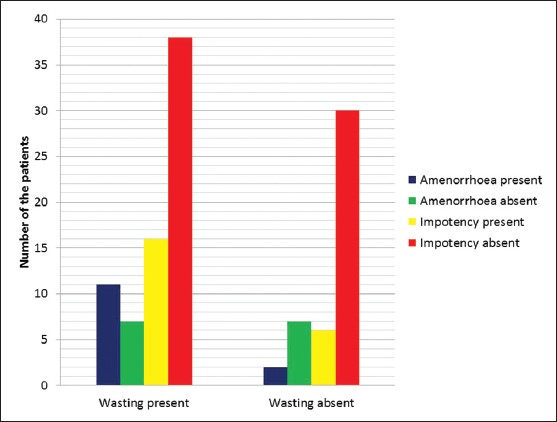 | Figure 1: Bar diagram showing number of the patients with wasting have amenorrhea and impotency
Click here to view |
Thyroid function test was done in 100 patients, of them, 9 (9%) had raised TSH; however, only 2% were overtly hypothyroid. Only 2% patients had low TSH; however, their T4 and T3 values were within normal range [Table 2].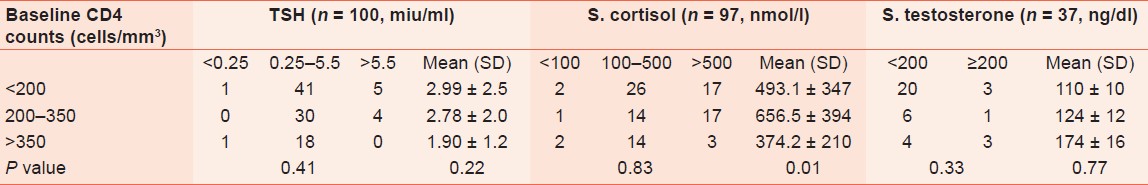 | Table 2: The distribution of the frequency of patients and the mean (SD) values of endocrine parameters done at the time of recruitment with respect to baseline CD4 cell counts
Click here to view |
Serum cortisol could be estimated in 97 patients. Serum cortisol values <100 nmol/l (definitive AI) was present in 5 (5.2%) patients, 38 (39.1%) patients had values >500 nmol/l (excludes AI), while 54 (55.6%) had indeterminate values, i.e., between 100-500 nmol/l [Table 2]. No patient had hypotension.
Serum testosterone, LH, and FSH could be estimated in 37 patients; all patients were males. The mean serum testosterone level was 124.81±117.61 ng/dl. Hypogonadism (serum testosterone <200 ng/dl) was found in 75.7% (28/37) patients. However, only 27% (10/37) of them had impotency on questioning. Three patients also had impotency despite their normal testosterone level. The mean LH was 2.55 ± 2.53 mIU/ml and mean FSH was 5.38 ± 3.97 mIU/ml. For male patients in whom LH and FSH was done, their values were found in normal range. BMI was related positively with serum testosterone level. But when their values were adjusted for regression analysis serum testosterone level, it was not independently related significantly to BMI [Table 3]. ART status of patients did have significant influence on the prevalence of various endocrinopathy [Table 4].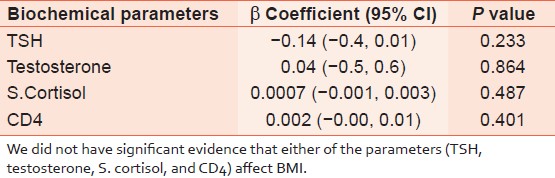 | Table 3: Regression analysis showing how BMI in HIV patients was affected by hormones levels (testosterone, serum cortisol, and TSH) and CD4 counts
Click here to view |
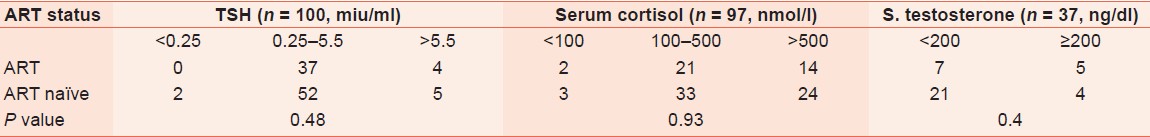 | Table 4: The distribution of the number of patients with respect to ART status for different ranges of the endocrine parameters
Click here to view |
| Discussion | |  |
It is important to diagnose endocrine metabolic disorders in HIV patients. However, they still remain neglected in HIV management. The most common clinical finding is weight loss, present in 64.9% and most of them (85.52%) belonged to AIDS category.
Most of the patients had normal T3 and T4 levels. TSH was raised in 9% patients (2% had overt hypothyroidism and 7% were subclinical cases). One patient had symptoms of constipation and dry skin, TSH-11 miu/ml, while other one had mild pericardial effusion and TSH of 20 miu/ml. Isolated low T4 was seen in 3% patients, and all of them were in AIDS category. Similar findings were described by Beltran et al., 2.6% patients had overt hypothyroidism, 6.6% had subclinical hypothyroidism, and 6.8% had isolated low T4. [11] The prevalence of subclinical hypothyroidism in both ART naive as well as in patients who were on ART were similar; this observation is also supported by Collazos et al. [12] However, in a study reported by Nelson et al., [13] a higher than expected incidence of overt hypothyroidism was found in patients receiving ART, and they recommend universal screening of subjects on therapy. Only 2% patients had low TSH, and they too were subclinical. Earlier, the prevalence of hyperthyroidism (overt and subclinical) in HIV infected patients have been reported to be <1%. [14]
We could make the diagnosis of definitive adrenal deficiency in approximately 5% patients, and around 55% patients had their serum cortisol in indeterminate range. We did not do ACTH stimulation test, therefore, the actual prevalence could not be estimated. In a study of 113 critically ill HIV infected patients, 19% prevalence of AI have been reported. [15] Whereas, in a study by Hoshino et al., [16] cortisol levels were raised in 30.14% of patients of advanced disease as compared to 20% in patients of early stages of HIV disease. Collazos et al. [17] reported reduced serum cortisol levels in 2.8% and increased levels in 12.8% in asymptomatic HIV patients. None of these patients had symptoms of hypo- or hypercortisolism. Serum cortisol levels have shown significant relationships with the CD4 cell count and the development of cachexia. [17],[18]
In the present study, a high frequency of hypogonadism was seen in males, but the serum testosterone could not be estimated in all male patients because this facility to estimate it was interrupted amid due to cost factor and unavailability of test kits. The complaint of impotency was reported more commonly in AIDS than in Non-AIDS group. The prevalence of impotency in 33% of advanced disease cases has been reported. [19] An interesting finding was that the serum testosterone levels were normal in three patients, yet they complaint of impotency; this entails that other factors, besides serum testosterone, attribute to impotency in HIV patients.
Here, the hypogonadism in males could not be ascribed to either hypogonadotrophic or hypergonadotrophic because the levels of gonadotrophins were normal in these patients. As the HIV disease progresses, secondary hypogonadism have been commonly found. [20] The study did not show any significant relationship between ART status of the patients and gonadal dysfunctions, probably due to the small number of the subjects on ART and the short duration of ART (median 3 month); therefore, its effect on hormonal dysfunction cannot be assured and we recommend a long follow-up to be made. Impotency and low levels of testosterone observed in HIV infected patients might have related to the progression of the HIV infection or as a result of compound effect of debilitating illnesses and secondary infections along with psychological effects.
In our study, around half of the female patients had amenorrhoea. Similarly, impotency and amenorrhea was seen more commonly in AIDS than in non-AIDS patients. In a retrospective study, Grinspoon et al. reported up to 20% prevalence of the amenorrhea. [21] This rate went up to 38% in women who were at <90% ideal body weight, clearly demonstrating an association between wasting and amenorrhea. However, we did not find significant association of amenorrhea with wasting present in HIV infected patients.
In the present study, wasting was evident in more than the half of HIV infected patients and was more frequent in the AIDS group. BMI did not correlate with either of endocrine functions tests that done here. Although controversial, hypogonadism may be more of a cause than effect of wasting. Therefore, wasting in HIV disease cannot be ascribed to be related with any endocrine disorder. There could have been the role of multiple factors acting in cohort, resulting in so-called debilitating state.
Although our results are limited by factors such as small sample size, unequal frequency of patients between AIDS and Non-AIDS group, and likewise between ART and ART-naïve patients, and that stipulated hormonal assay could not be performed and measured in all patients, we would like to conclude that hypothyroidism seen in HIV patients was predominantly subclinical. Decreased levels of serum cortisol were found, although with unclear clinical significance. Male patients had hypogonadism, probably hypogonadotropic type, but the frequency of symptoms of impotency did not match with the frequency of hypogonadism detected on hormonal assay. Authors recommend that a large study from this part of world is required to better elucidate the endocrine disorders in HIV infected patients and their relation with stages of the HIV infection and ART being taken.
| Acknowledgement | |  |
The authors wish to express their deepest gratitude and warmest appreciation to all HIV patients enrolled in this study, who, in any way have contributed and inspired the authors for the overall success of the undertaking
| References | |  |
| 1. | AIDS epidemic update. World Health Organization. Retrieved 29 July 2011. 
|
| 2. | UNAIDS (2010) ′UNAIDS report on the global AIDS epidemic. 
|
| 3. | Dobs AS, Dempsey MA, Ladenson PW, Polk BF. Endocrine disorders in men infected with human immunodeficiency virus. Am J Med 1988;84:611-6. 
[PUBMED] |
| 4. | Hofbauer LC, Heufelder AE. Endocrine implications of human immunodeficiency virus infection. Medicine (Baltimore) 1996;75:262-78. 
[PUBMED] |
| 5. | Lo JC, Schambelan M. Endocrine disease. In: Dolin R, Masur H, Saag MS, editors. AIDS Therapy. Philadelphia: Churchill Livingstone; 1999. p. 740-51. 
|
| 6. | Croxson TS, Chapman WE, Miller LK, Levit CD, Senie R, Zumoff B. Changes in the hypothalamic-pituitary-gonadal axis in human immunodeficiency virus-infected homosexual men. J Clin Endocrinol Metab 1989; 68:317-21. 
[PUBMED] |
| 7. | Rosenfeld CR, Calabrese LH. Progression of autoimmune thyroiditis in an HIV-infected woman on HAART. AIDS Read 1999:9:393-4. 
|
| 8. | Takarabe D, Rokukawa Y, Takahashi Y, Goto A, Takaichi M, Okamoto M, et al. Autoimmune diabetes in HIV-infected patients on highly active antiretroviral therapy. J Clin Endocrinol Metab 2010;95:4056-60. 
[PUBMED] |
| 9. | Meena LP, Rai M, Singh SK, Chakravarty J, Singh A, Goel R, et al. Endocrine changes in male HIV patients. J Assoc Physicians India 2011;59:365-71. 
[PUBMED] |
| 10. | National AIDS Control Organisation, Antiretroviral Therapy Guidelines for HIV-infected Adults and Adolescents Including Post-exposure Prophylaxis. Available from: http://www.ilo.org/aids/legislation/WCMS_117317/lang-en/index.htm [Last accessed on 5th of Jan 2013] 
|
| 11. | Beltran S, Lescure FX, Desailloud R, Douadi Y, Smail A, EI Esper I, et al. Increased prevalence of hypothyroidism among human immunodeficiency virus-infected patients: A need for screening. Clin Infect Dis 2003;37:579-83. 
|
| 12. | Collazos J, Ibarra S, Mayo J. Thyroid hormones in HIV infected patients in the highly active antiretroviral therapy era: Evidence of an interrelationship between the thyroid axis and the immune system. AIDS 2003:17:763-5. 
|
| 13. | Nelson M, Powles T, Zeitlin A, Sen P, Scourfield A, Bower M, et al. Thyroid dysfunction and relationship to antiretroviral therapy in HIV positive individuals in the HAART era. J Acquir Immune Defic Syndr 2009;50:113-4. 
[PUBMED] |
| 14. | Madge S, Smith CJ, Lampe FC, Thomas M, Johnson MA, Youle M, et al. No association between HIV disease and its treatment and thyroid function. HIV Med 2007;8:22-7. 
|
| 15. | Meya DB, Katabira E, Otim M, Ronald A, Colebunders R, Njama D, et al. Functional adrenal insufficiency among critically ill patients with human immunodeficiency virus in a resource-limited setting. Afr Health Sci 2007;7:101-7. 
[PUBMED] |
| 16. | Hoshino Y, Yamashita N, Nakamura T, Iwamoto A. Prospective examination of adrenocortical function in advanced AIDS patients. Endocr J 2002;49:641-7. 
[PUBMED] |
| 17. | Collazos J, Mayo J, Martínez E, Ibarra S. Serum cortisol in HIV-infected patients with and without highly active antiretroviral therapy. AIDS 2003;17:123-6. 
|
| 18. | Membreno L, Irony I, Dere W, Klein R, Biglieri EG, Cobb E. Adrenocortical function in acquired immunodeficiency syndrome. J Clin Endocrinol Metab 1987;65:482-7. 
[PUBMED] |
| 19. | Villette JM, Bourin P, Doinel C, Mansour I, Fiet J, Boudou P, et al. Circadian variations in plasma levels of hypophyseal, adrenocortical and testicular hormones in men infected with human immunodeficiency virus. J Clin Endocrinol Metab 1990;70:572-7. 
[PUBMED] |
| 20. | Coodley GO, Loveless MO, Nelson HD, Coodley MK. Endocrine function in the HIV wasting syndrome. J Acquir Immune Defic Syndr 1994;7:46-51. 
[PUBMED] |
| 21. | Grinspoon S, Corcoran C, Miller K, Biller B, Askari H, Wang E, et al. Body composition and endocrine function in women with AIDS wasting. J Clin Endocrinol Metab 1997;82:1332-7. 
|
[Figure 1]
[Table 1], [Table 2], [Table 3], [Table 4]
|