|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 1
| Issue : 2 | Page : 64-69 |
|
Decentralization of prevention-of-mother-to-child transmission services in Nigeria: Aminu Kano teaching hospital's experience
Hadiza S Galadanci1, Sule A Gaya1, Sanusi Abubakar2, Zubairu Iliyasu1
1 Department of Obstetrics and Gynaecology, Aminu Kano Teaching Hospital, Kano, Nigeria
2 Department of Community Medicine, Aminu Kano Teaching Hospital, Kano, Nigeria
| Date of Acceptance | 25-Dec-2013 |
| Date of Web Publication | 6-Feb-2014 |
Correspondence Address:
Hadiza S Galadanci
Aminu Kano Teaching Hospital, Kano
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157 .126633

Introduction: Human Immune deficiency virus infection is a major public health issue in Sub-Saharan Africa with Nigeria having one of the highest burden of human immunodeficiency virus (HIV) disease among pregnant women and children. Since 2003, Aminu Kano Teaching Hospital (AKTH) has been providing prevention-of-mother-to-child transmission (PMTCT) services. This study examined the pattern of HIV counseling and testing (HCT) uptake among antenatal clients at the hospital during a 6-year period. This includes the period when decentralization of PMTCT services occurred in Nigeria. Materials and Methods: This is a hospital-based prospective study that included all pregnant women attending antenatal clinic (ANC) at AKTH, from January 2007 to December 2012. Since October 2003, data are prospectively recorded in registers and later entered into a database. The registers captured information on clients' age, parity, occupation and gestational age at time of registering; they also noted voluntary counseling and testing (VCT)/HCT uptake, HIV sero-status and partner's HIV status. The study obtained data from the hospital registers and subsequently analyzed it using the EPI-Info; version 3.2.2 (released in 2004) statistical software package. Results: The mean maternal age was 27.2 5.3 years and the median parity is 1 with a range of 1-14. Of the 23,378 new attendees at ANC, 23,078 (98.7%) accepted testing for HIV. Acceptance of HIV test stayed at 100% from 2007 to 2011 and only dipped slightly to 93.3% in 2012. Overall HIV prevalence was 5.5%. HIV prevalence stabilized at between 8.1% and 8.4% in 2007 and 2008 respectively, before rising to peak at 10.0% in 2009 and started declining to 5.8% in 2010 before reaching its lowest values of 1.7% and 1.1% in 2011 and 2012 respectively. This trend was statistically significant with a P < 0.000. Conclusions: There is a high uptake of VCT among ANC clients and HIV prevalence has decreased significantly in the last 3 years in AKTH, probably as a result of decentralization of PMTCT services. Keywords: Decentralization of prevention-of-mother-to-child transmission services, human immunodeficiency virus counseling and testing uptake, human immunodeficiency virus seroprevalence, Nigeria, prevention-of-mother-to-child transmission
How to cite this article:
Galadanci HS, Gaya SA, Abubakar S, Iliyasu Z. Decentralization of prevention-of-mother-to-child transmission services in Nigeria: Aminu Kano teaching hospital's experience. J HIV Hum Reprod 2013;1:64-9 |
How to cite this URL:
Galadanci HS, Gaya SA, Abubakar S, Iliyasu Z. Decentralization of prevention-of-mother-to-child transmission services in Nigeria: Aminu Kano teaching hospital's experience. J HIV Hum Reprod [serial online] 2013 [cited 2017 Feb 4];1:64-9. Available from: http://www.j-hhr.org/text.asp?2013/1/2/64/126633 |
| Introduction | |  |
Sub-Saharan Africa is home to approximately 69% of the estimated 34.0 million persons worldwide who are living with human immunodeficiency virus (HIV) infection by the end of 2011; in this region, women represent about 60% of those infected. [1] As at 2009, Nigeria ranked second only to South Africa among countries with the highest total burden of HIV infection globally. It also has the highest burden of HIV disease among pregnant women and children (30% of the global burden). The number of persons living with HIV infection in Nigeria was estimated to be 2.95 million with 323,000 new adult and 57,000 new childhood infections. [2] Based on the Nigerian National Strategic Plan projections it is estimated that in 2010, there will be 6,286,861 pregnant women among whom 215,001 HIV positive women will require antiretrovirals (ARVs), while 222,300 will require ARVs in 2011. Estimated annual total acquired immunodeficiency syndrome (AIDS)-related deaths in 2010 were 181,774 (males 81,728 and females 100,046). Furthermore, the number of children orphaned by HIV will be about 2.23 million and the AIDS attributable under five mortality 5%. [3] In 2009, the World Health Organization estimated that 370,000 children were newly infected with HIV globally, with the majority dying before the 2 nd year of life. [4],[5] More than 90% of these children acquire the infection during pregnancy, birth, or breastfeeding- the vast majority of which are preventable with ARV prophylaxis. [4] The situation is particularly acute in Nigeria, a country with limited resources and a high burden of HIV disease among pregnant women. [4] Although estimates vary, between 4% and 12% of pregnant women are infected with HIV in Nigeria. [5],[6],[7],[8] Data further suggest that mother-to-child transmission (MTCT) rates approach 30-45% without intervention in Nigeria, and the Federal Ministry of Health estimates that between 67,000 and 125,000 children are infected through MTCT each year. [9],[10] Most recently, 240,000 children were reported to be living with HIV in Nigeria in 2009, among the highest numbers reported in the world. [9],[11] The HIV pandemic has eroded hard-won gains in infant and child survival. For instance, it was speculated that an estimated 600,000 infants were becoming infected with HIV annually; almost all these infections occur in developing countries and more than 90% are the result of MTCT of HIV during pregnancy, labor or breastfeeding. [12] Without intervention, there is a 20-45% chance that a baby born to an HIV-infected mother will become infected. [12] By implication, most infant HIV infections could be averted. The core of the problem is that relatively few of the world's pregnant women are being reached by prevention-of-mother-to-child transmission (PMTCT) services.
Earlier clinical trials demonstrated that 37-50% reduction in MTCT of HIV-1 can be achieved through a short course of zidovudine (AZT) [13],[14] or nevirapine. [15] Subsequently, pilot programs in support of PMTCT were begun in 1999 in several African countries, [16] and such interventions were implemented as part of public health programs in some developing countries. [17] At about the same time, it was also found that breastfeeding by an HIV-infected mother increased the risk of transmission by 5-20%. [12] In 2001, the United Nations General Assembly declared as one of its goals the reduction of the proportion of infants infected with HIV: by 20% by 2005 and 50% by 2010. This was to be achieved by ensuring that at least 80% of pregnant women accessing antenatal care have access to information, counseling and other HIV-prevention services. [18] Pursuant to these goals, the Nigerian Government established centers providing PMTCT services, including voluntary counseling and testing (VCT) for HIV, ARV prophylaxis/treatment and counseling on infant feeding options. Aminu Kano Teaching Hospital (AKTH) in northern Nigeria has provided PMTCT services since October 2003. However in response to the global call for elimination of mother to child transmission (eMTCT) of HIV, Nigeria in 2010 recognized the need to decentralize and integrate PMTCT services to the Secondary and Primary Health care centers. This study examines the pattern of HTC uptake among antenatal clients there during a 6-year period including the period of decentralization and describes the HIV sero-positivity of clients in terms of maternal age, parity and infant's gestational age.
| Materials and Methods | |  |
AKTH is a 500-bed hospital established in 1988. It is located in Kano, the largest commercial center of northern Nigeria. The hospital receives clients from within Kano and the neighboring states of Jigawa, Katsina, Kaduna, Bauchi and Zamfara. The majority of patients are Hausa or Fulani, although substantial numbers are Igbo or Yoruba. Most are traders, farmers, businessmen or civil servants. The hospital operates a specialist antenatal clinic (ANC) 4 times/week, attending to an average of 120 clients/day; other services offered by the ANC include family planning, postnatal care, immunization and screening for cervical cancer.
The PMTCT program has been fully integrated into the hospital's obstetrics services. The program includes PMTCT intervention offered in the ANC and labor room and during the postpartum period. In the ANC, HIV Counseling and Testing (HCT) is offered to all new clients, with a right to "opt out". HIV-positive patients are provided ARV drugs; initially this was only nevirapine (during labor), but, since 2005, combined therapy (at least 2-3 ARV drugs) has been offered in the antenatal period, following the revised national guidelines on PMTCT. Other interventions at the hospital are modification of obstetric practices (e.g. delay in rupture of the placental membrane and avoidance of assisted vaginal delivery and episiotomy). This is a hospital-based prospective study that included all pregnant women attending antenatal care at AKTH, from January 2007 to December 2012. We have already published our data from 2003 to 2006. [19] Approval for the study was obtained from the institutional review board at the hospital. The National PMTCT Task Team of the Federal Ministry of Health (in Abuja) and other stakeholders had developed data collection instruments, including registers and summary forms, based on the indicators needed to best evaluate the national PMTCT program. These data collection instruments were distributed to the participating Centers, including AKTH. Since commencement of the hospital's PMTCT program in October 2003, data are prospectively recorded in registers and later entered into a database. The registers captured information on clients' age, parity, occupation and gestational age at time of registering; they also noted VCT/HCT uptake, HIV sero-status and partner's HIV status. Thus, data for women attending antenatal care were obtained from the hospital registers and subsequently analyzed using the EPI-Info® 6.0 statistical software package. [20] HIV seroprevalence was estimated, with corresponding 95% confidence intervals and a Chi-square test was used to determine significance of the observed trends; level of significance was set at P < 0.05.
| Results | |  |
Between January 2007 and December 2012, 23,378 new attendees presented at the ANC of AKTH; all were pre-test counseled. The mean maternal age is 27.2 ± 5.3 years and similarly the median parity is 1 with a range of 1-14 as shown in [Table 1]. Out of the total new attendees, 23,078 (98.7%) accepted testing for HIV. The proportion of pregnant women accepting HIV test stayed at 100% from 2007 to 2011 and only dipped slightly to 93.3% in 2012 [Table 2]. For the overall period, HIV prevalence was 5.5% as 1275 women tested HIV-positive. Considered annually, HIV prevalence stabilized at between 8.1% and 8.4% in 2007 and 2008 respectively, before rising to peak at 10.0% in 2009 and started declining to 5.8% in 2010 before reaching its lowest values of 1.7% and 1.1% in 2011 and 2012 respectively. This trend was statistically significant [Figure 1] (χ2 trend = 378.9; P < 0.000). | Table 1: Socio-demographic variables of pregnant women attending antenatal clinic at Aminu Kano teaching hospital during the period under review
Click here to view |
 | Table 2: Voluntary counseling and testing uptake among antenatal clients at Aminu Kano teaching hospital, Nigeria (2 trend=378.9; P<0.0000)
Click here to view |
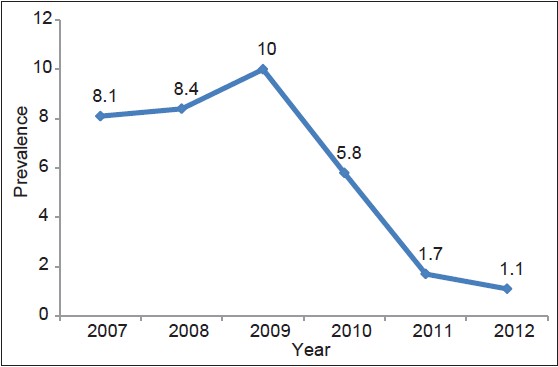 | Figure 1: Trend of human immunodeficiency virus prevalence among women attending antenatal clinic at Aminu Kano teaching hospital
Click here to view |
HIV sero-prevalence for the overall 6-years period was 5.5% and regardless of the outcome of HIV testing, all women received post-test counseling and HIV-positive mothers were offered PMTCT interventions, including ARV prophylaxis and treatment, modification of obstetric services and infant feeding counseling.
| Discussion | |  |
The uptake of HCT among antenatal clients at AKTH during the study period was relatively high (98.7%). The trend of HCT uptake has been increasing from 93.5% in 2004 [19] to 100% in 2006 [21] and remained at 100% from 2007 to 2011. The uptake then fell to 93.3% in 2012. This could be due to increased awareness about HIV/AIDS and PMTCT services among pregnant women in the study area, although that does not explain the decline in 2012. There is the need to investigate this decline further.
For the overall period, HIV prevalence was 5.5%. HIV prevalence stabilized at between 8.1% and 8.4% in 2007 and 2008 respectively, before rising to peak at 10.0% in 2009 and started declining to 5.8% in 2010 before reaching its lowest values of 1.7% and 1.1% in 2011 and 2012 respectively. This clearly shows a reduction in HIV prevalence from 2009 to 2012. This may be as a result of many more centers now offering PMTCT services in the state including secondary health care facilities and Primary Health Centers and therefore less positive patients are referred to AKTH. Initially AKTH was serving not only Kano state but also the neighboring North Western States. As from 2010, Nigeria in response to the global call for eMTCT of HIV, with the goal of reducing the MTCT rate to < 5% and reduce new pediatric infections by 90% from baseline by 2015, identified the need to "rapidly accelerate" the provision of quality PMTCT services across the country, the necessity of decentralizing PMTCT services to primary health care level and the importance of successful integration of PMTCT services into routine maternal and child health services. [22] This may therefore explain the reduced number of positive patients in AKTH as more PMTCT service centers were established.
The prevalence of 5.5% is higher than the reported national estimate of HIV sero-prevalence among pregnant women in Nigeria (4.1%); [23] and also higher than 1.5%, 2.1% and 2.7% HIV prevalence reported for Jigawa, Yobe and Osun states, respectively. [23] These figures are also higher than those reported for Kano during sentinel surveys conducted in 2001 (3.3%), 2003 (4.3%) and 2005 (4.3%) but lower than that of the last sentinel survey (11.2%) conducted in 2010. [23] The difference may be related to the fact that sentinel surveys are point-prevalence estimates, obtained bi-annually and are subject to the effect of fluctuations in patient flow, whereas this was a period-prevalence study, involving all consenting ANC attendees over the entire 6-year study period. Furthermore, as a referral center providing free PMTCT services, the ANC at AKTH receives many clients from other facilities within and outside Kano State.
The mean maternal age of 27.2 ± 5.3 years has not changed significantly from the findings in the previous report at the same center. [19] This pattern is of great concern, as many young mothers who are just joining the reproductive age group are already HIV infected. HIV prevalence among 15-24-year-old is used as a proxy for measuring the rate of new infections in the general population, since those persons represent new entrants into the reproductive age group. Unstable premarital sexual relationships could be predisposing young women to HIV infection, since, in most developing countries, HIV is predominantly transmitted through hetero-sexual contact. [24] This observation was similar to other findings in Africa. [25],[26],[27] This suggests that most HIV infections in women occur at a relatively young age, during the first few years after sexual debut. [27] An immature genital tract and cervical ectopy, which is common in young women, might increase the risk of infection with HIV [28] and untreated STIs may magnify an individual's biological. [29] Furthermore, African women tend to have older partners at sexual debut or later, thus they may experience higher risk by being exposed to partners who are already HIV infected. [27],[30],[31],[32] HIV prevention programs should therefore continue to target young people, especially women, with the aim of empowering them to delay sexual debut and to improve their negotiating skills, especially regarding condom use. There is also the on-going need to encourage partner testing and disclosure.
Similarly the median parity is 1, which shows that the prevalence is still higher among women of low parity as documented in the previous study at the same center. [19] This concurs with the findings of the last national sentinel survey. [24]
The most worrying observation made during the research was that the HCT uptake fell to 93.3% in 2012 after it had stabilized at 100% for years. This is worrisome because while celebrating for a success there are still some women attending AKTH that did not use the opportunity to be tested for HIV and therefore they lost the benefit of receiving PMTCT services if they had been HIV-positive. Although testing in labor is done, some women may still miss these opportunities. All babies born to HIV-positive mothers at AKTH are given a single dose of nevirapine syrup within 72 h of delivery and for 6 weeks afterwards, according to the national guidelines on PMTCT. [10] Mothers are given the option of exclusive breast feeding for the first 6 months, then breast feeding with supplementary feeding for the next 6 months while the mother is on HAART during infant feeding counseling. The site is being supported by IHVN where we implement option B plus in which all the mothers will continue on HAART for the rest of their life irrespective of their CD4 count or stage of the disease.
The study had several limitations. First, as a hospital-based study, we recognize that attendance at ANCs is dependent on literacy level, cultural factors and socio-economic factors. Secondly, we note that high-risk pregnancies are usually pooled at such referral centers. Therefore, the HIV seroprevalence estimate obtained for the women for the 6-year period may overestimate the level rate in the population. HIV infection can also decrease fertility in women, both as a result of sub-fertility or increased early pregnancy loss. [33] Likewise, HIV-infected women also have higher rates of tubal infertility secondary to pelvic inflammatory diseases. [34] Therefore, the prevalence estimate presented will fail to include those who are not able to become pregnant.
| Conclusions | |  |
HIV is a major public health problem among women of reproductive age. There is a high uptake of VCT among pregnant women using the ANC at AKTH. The HIV prevalence has decreased significantly in the last 3 years in AKTH, which could be due to actual reduction of prevalence of HIV or due to decentralization of PMTCT services to secondary health care and primary health care facilities.
| Acknowledgments | |  |
We wish to acknowledge the invaluable support that the PMTCT program at Aminu Kano Teaching Hospital in Kano receives from the Federal Ministry of Health (Nigeria) and funding from the United States President's Emergency Plan for AIDS Relief (PEPFAR), implemented by the Institute of Human Virology, Nigeria, an affiliate of the Institute of Human Virology, University of Maryland in Baltimore, Maryland. Likewise, we wish to thank all our hospital clients for giving us the opportunity to offer them our services.
| References | |  |
| 1. | UNAIDS Report on the Global AIDS Epidemic. Geneva: UNAIDS; 2012. 
|
| 2. | WHO, UNAIDS and UNICEF. Towards Universal Access: scaling up Priority HIV/AIDS Interventions in the Health Sector. Geneva: World Health Organization; Progress Report 2009. 
|
| 3. | Nigerian National HIV/AIDS Strategic Plan 2010-2015. Abuja: NACA; 2010. 
|
| 4. | WHO. PMTCT Strategic Vision 2010-2015: Preventing Mother-to-child Transmission of HIV. Geneva: World Health Organization; 2010. Available from: http://www.who.int/hiv/pub/mtct/strategic_vision/en/index.html. [Last accessed on 2012 Dec 16]. 
|
| 5. | UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic. Geneva: UNAIDS; 2010. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2010/20101123_globalreport_en.pdf. [Last accessed on 2012 Dec 16]. 
|
| 6. | Adeyi O, Kanki P, Odutolu O, Idoko J. (Eds.) AIDS in Nigeria: a Nation on the Threshold. Cambridge: Harvard University Press; 2006 
|
| 7. | Chama CM, Audu BM, Kyari O. Prevention of mother-to-child transmission of HIV at Maiduguri, Nigeria. J Obstet Gynaecol 2004;24:266-9. 
[PUBMED] |
| 8. | WHO. Epidemiology Fact Sheet on HIV/AIDS- Nigeria 2008. Geneva: World Health Organization; 2008. Available from: http://www.apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_NG.pdf. [Last accessed on 2013 Jun 27]. 
|
| 9. | Audu RA, Salu OB, Musa AZ, Onyewuche J, Funso-Adebayo EO, Iroha EO, et al. Estimation of the rate of mother to child transmission of HIV in Nigeria. Afr J Med Med Sci 2006;35:121-4. 
[PUBMED] |
| 10. | Federal Ministry of Health - Nigeria. National PMTCT and HIV and Infant Feeding Guidelines. Abuja: NACA; 2009. 
|
| 11. | Office of Inspector General. Audit of USAID/Nigeria's PEPFAR Funded Activities and Commodities for the Prevention of Mother-to-Child Transmission of HIV. Report No. 7-620-10-002-P: Dakar, Senegal; 2010. 
|
| 12. | De Cock KM, Fowler MG, Mercier E, de Vincenzi I, Saba J, Hoff E, et al. Prevention of mother-to-child HIV transmission in resource-poor countries: Translating research into policy and practice. JAMA 2000;283:1175-82. 
[PUBMED] |
| 13. | Wiktor SZ, Ekpini E, Karon JM, Nkengasong J, Maurice C, Severin ST, et al. Short-course oral zidovudine for prevention of mother-to-child transmission of HIV-1 in Abidjan, Côte d'Ivoire: A randomised trial. Lancet 1999;353:781-5. 
[PUBMED] |
| 14. | Shaffer N, Chuachoowong R, Mock PA, Bhadrakom C, Siriwasin W, Young NL, et al. Short-course zidovudine for perinatal HIV-1 transmission in Bangkok, Thailand: A randomised controlled trial. Bangkok Collaborative Perinatal HIV Transmission Study Group. Lancet 1999;353:773-80. 
[PUBMED] |
| 15. | Guay LA, Musoke P, Fleming T, Bagenda D, Allen M, Nakabiito C, et al. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomised trial. Lancet 1999;354:795-802. 
[PUBMED] |
| 16. | UNICEF. Prevention of Mother-to-Child Transmission of HIV/AIDS. UNICEF Support for Pilot Projects in Sub-Saharan Africa, 2007. Available from: http://www.unicef.org/programme/hiv/mtct/proj.htm. [Last accessed on 2007 Feb 23]. 
|
| 17. | Dabis F, Newell ML, Fransen L, Saba J, Lepage P, Leroy V, et al. Prevention of mother-to-child transmission of HIV in developing countries: Recommendations for practice. The Ghent International Working Group on Mother-To-Child Transmission of HIV. Health Policy Plan 2000;15:34-42. 
[PUBMED] |
| 18. | United Nations UNGASS Declaration of Commitment on HIV/AIDS. Resolution Adopted by the United Nations General Assembly Special Session on HIV/AIDS. New York: United Nations; 2001. p. 25-7. 
|
| 19. | Galadanci HS, Iliyasu Z, Tukur J, Muktar-Yola M, Adeleke SI. Uptake of voluntary counselling and testing for HIV by pregnant women in a prevention-of-mother-to-child-transmission programme at Aminu Kano Teaching Hospital, Nigeria. Afr J AIDS Res 2008;7:143-8. 
|
| 20. | Dean AG, Burton AH, Dicker RC. Epi-Info Version 6. A Word Processing, Database and Statistics Program for Epidemiology on Microcomputers. Stone Mountain, Georgia: USD Incorporated; 1999. 
|
| 21. | Iliyasu Z, Kabir M, Galadanci HS, Abubakar IS, Aliyu MH. Awareness and attitude of antenatal clients towards HIV voluntary counselling and testing in Aminu Kano Teaching Hospital, Kano, Nigeria. Niger J Med 2005;14:27-32. 
[PUBMED] |
| 22. | Federal Ministry of Health National scale up plan towards elimination of mother to child transmission of HIV in Nigeria 2010-2015. 
|
| 23. | Federal Ministry of Health (FMoH)/National Action Committee on AIDS (NACA). 2009 National HIV Sero-Prevalence Sentinel Survey, Technical Report. Abuja, Nigeria: FMoH and NACA; 2009. 
|
| 24. | Federal Ministry of Health (FMoH)/National Action Committee on AIDS (NACA). 2005 National HIV Sero-Prevalence Sentinel Survey, Technical Report. Abuja, Nigeria: FMoH and NACA; 2005. 
|
| 25. | Glynn JR, Caraël M, Auvert B, Kahindo M, Chege J, Musonda R, et al. Why do young women have a much higher prevalence of HIV than young men? A study in Kisumu, Kenya and Ndola, Zambia. AIDS 2001;15 Suppl 4:S51-60. 
|
| 26. | Mwaluko G, Urassa M, Isingo R, Zaba B, Boerma JT. Trends in HIV and sexual behaviour in a longitudinal study in a rural population in Tanzania, 1994-2000. AIDS 2003;17:2645-51. 
[PUBMED] |
| 27. | Tanzania Commission for AIDS (TACAIDS). National Bureau of Statistics (NBS) and ORC Macro. Tanzania HIV/AIDS Indicator Survey 2003-04. Calverton, Maryland: TACAIDS, NBS and ORC Macro; 2005. 
|
| 28. | Plourde PJ, Pepin J, Agoki E, Ronald AR, Ombette J, Tyndall M, et al. Human immunodeficiency virus type 1 seroconversion in women with genital ulcers. J Infect Dis 1994;170:313-7. 
[PUBMED] |
| 29. | Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: The contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect 1999;75:3-17. 
[PUBMED] |
| 30. | Laga M, Schwärtlander B, Pisani E, Sow PS, Caraël M. To stem HIV in Africa, prevent transmission to young women. AIDS 2001;15:931-4. 
|
| 31. | Gregson S, Nyamukapa CA, Garnett GP, Mason PR, Zhuwau T, Caraël M, et al. Sexual mixing patterns and sex-differentials in teenage exposure to HIV infection in rural Zimbabwe. Lancet 2002;359:1896-903. 
|
| 32. | Mocumbi P, Amaral E. Reproductive rights and HIV/AIDS. Best Pract Res Clin Obstet Gynaecol 2006;20:381-93. 
[PUBMED] |
| 33. | Gray RH, Wawer MJ, Serwadda D, Sewankambo N, Li C, Wabwire-Mangen F, et al. Population-based study of fertility in women with HIV-1 infection in Uganda. Lancet 1998;351:98-103. 
[PUBMED] |
| 34. | Kamenga MC, De Cock KM, St Louis ME, Touré CK, Zakaria S, N'gbichi JM, et al. The impact of human immunodeficiency virus infection on pelvic inflammatory disease: A case-control study in Abidjan, Ivory Coast. Am J Obstet Gynecol 1995;172:919-25. 
|
[Figure 1]
[Table 1], [Table 2]
|