|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 1
| Issue : 2 | Page : 77-83 |
|
Assessment of sexual behavior and serostatus disclosure among people living with HIV/AIDS (PLWHAs) attending antiretroviral therapy center in tertiary care Hospital, Baroda
Kedar G Mehta1, Rajendra K Baxi2, Sangita V Patel2, Parag D Chavda1, Vihang S Mazumdar2
1 Department of Community Medicine, GMERS Medical College, Gotri, Gujarat, India
2 Department of Community Medicine,Government Medical College, Baroda, Gujarat, India
| Date of Acceptance | 27-Dec-2013 |
| Date of Web Publication | 6-Feb-2014 |
Correspondence Address:
Kedar G Mehta
Department of Community Medicine, GMERS Medical College Gotri, Baroda, Gujarat
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157 .126636

Introduction: As more and more people with human immunodeficiency virus (HIV) live longer and enjoy healthier lives because of antiretroviral therapy, there are an increasing number of sexual transmissions of HIV. It is exceedingly important to assess the proportion of unsafe sexual practices among people living with HIV/AIDS (PLWHAs) and their disclosure status so that behavioral intervention can be designed optimally for them in order to curb secondary HIV transmission and potential reinfection with different or drug resistant strain of HIV. Aim: To assess sexual behavior and serostatus disclosure of PLWHAs attending antiretroviral therapy (ART) center in Vadodara. Settings and Design: The current cross-sectional study was carried out at ART center of a tertiary care hospital - Shree Sayaji General (SSG) Hospital, Vadodara after taking necessary permissions and approval from institutional review board (IRB). Materials and Methods: A semistructured questionnaire was used for interview with PLWHA who are on ART after taking written and informed consent. Data was entered and analyzed using Epi Info software. Results: A total of 175 PLWHAs were enrolled in this study. Forty-three percent of the PLWHAs practiced premarital sex, while 15% of them practiced extramarital sex (EMS). Nearly 90% of these sexual practices were unsafe. Fifty-eight percent of the PLWHAs continued these unsafe sexual practices even after HIV diagnosis. Nearly 20% of the PLWHAs did not receive any counseling regarding sexual behavior. Ninety-five percent of respondents had disclosed their serostatus to their spouse. Conclusions: Still a remarkable proportion of PLWHAs indulge in unsafe sexual practices and the most common reason encountered among them was desire for child. Although majority of the participants had disclosed their serostatus to their spouse, many respondents did not mention their serostatus to other sexual partners. There is a need to stress on the importance of safe sex among PLWHAs not only to prevent transmission to their partners, but also to help them avoid receiving potentially resistant HIV strains in case of seroconcordant couples. A need-based sexual behavior-related motivational counseling needs to be focused on. Keywords: Baroda, PLWHAs, serostatus disclosure, sexual behavior
How to cite this article:
Mehta KG, Baxi RK, Patel SV, Chavda PD, Mazumdar VS. Assessment of sexual behavior and serostatus disclosure among people living with HIV/AIDS (PLWHAs) attending antiretroviral therapy center in tertiary care Hospital, Baroda. J HIV Hum Reprod 2013;1:77-83 |
How to cite this URL:
Mehta KG, Baxi RK, Patel SV, Chavda PD, Mazumdar VS. Assessment of sexual behavior and serostatus disclosure among people living with HIV/AIDS (PLWHAs) attending antiretroviral therapy center in tertiary care Hospital, Baroda. J HIV Hum Reprod [serial online] 2013 [cited 2017 Mar 5];1:77-83. Available from: http://www.j-hhr.org/text.asp?2013/1/2/77/126636 |
| Introduction | |  |
India has the third largest number of human immunodeficiency virus (HIV) cases in the world (after South Africa and Nigeria), with an estimated 23.9 lac infected individuals. [1] The most common mode of transmission of HIV in India is through unprotected sex with infected person, and this contributes about 87.4% route of HIV transmission. [2]
Until recently, the focus of HIV prevention effort worldwide was largely on people uninfected with HIV and for a long time, the sexual behavior of HIV-infected persons did not receive any serious attention for a variety of reasons. Initially, diagnosis of HIV-infection appeared to imply a death sentence. In this context, the sexual life of those infected seemed a secondary issue making prevention focused on sexual behavior hard to imagine. Furthermore, the conviction that stigmatization should be avoided also precluded an interest in the sexual behavior of HIV infected persons. [3],[4]
As more and more people with HIV live longer and enjoy healthier lives because of antiretroviral therapy, an increasing number of sexual transmissions of HIV may stem from those who know they are infected and engage in unprotected sex. [5] Moreover, disclosure of the HIV status to one's sexual partner is an important prevention goal emphasized by the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) in their protocols for HIV counseling and testing. [6]
With the rollout of antiretroviral therapy in India, where about 3.84 lac people are on antiretroviral treatment [2] and has potential to prolong the lives of HIV-infected individuals, it is exceedingly important to understand the factors responsible for risky sex among the HIV positive persons, so that behavioral intervention can be designed optimally for them in order to curb secondary HIV transmission and potential reinfection with different or drug resistant strain of HIV.
In Gujarat, there is currently a paucity of data regarding the prevention needs of HIV-infected persons. The current study tries to assess the sexual behavior and status disclosure among people living with HIV/AIDS (PLWHAs) attending antiretroviral therapy (ART) center in Shree Sayaji General (SSG) Hospital, Vadodara, Gujarat.
| Objective | |  |
To assess sexual behavior and serostatus disclosure of PLWHA attending ART center in Vadodara.
| Materials and Methods | |  |
The current descriptive cross-sectional study was carried out at ART center of a tertiary care hospital-SSG Hospital, Vadodara-affiliated to Medical College Baroda, from November 2011 to November 2012. Before starting enrolment of the participants, necessary clearances and permissions were obtained from concerned authorities including Gujarat State AIDS Control Society (GSACS), Institutional Ethics Committee for Human Research (IECHR), Nodal Officer of ART center and Hospital Superintendent.
The proportion of inconsistent condom use from a previous qualitative study carried in the same set up was 0.2, keeping the confidence interval (CI) at 95% and the width of CI at 0.10 (on either side) and based on these estimates, the sample size calculated was 246. [7],[8] Assuming a 5% refusal rate, finally the sample size came to 260 participants. Since the proportion of pre-ART to ART patients was 1:2, so it was decided to enroll 85 pre-ART patients and 175 ART patients. The current study presents the findings among patients on ART. An interview schedule was used for collection of information on the variables of interest with study participants. They were given the information sheet containing the information regarding this research study in brief in English/Gujarati (the vernacular language) as preferred by interviewee. Then written and informed consent in English/Gujarati was taken from the participants. A semistructured questionnaire was used for interview. The questionnaire was first prepared in English, and then translated to Gujarati, and finally Gujarati version was translated back to English to check the validity. The interview schedule was designed to last approximately 30 min and was administered in Gujarati or English based on the language preferences of the individual. All interviews were conducted providing sufficient privacy in SSG Hospital, Vadodara.
Data was entered and analyzed in Epi Info software (version 6.04d). [9] The primary outcome, inconsistent condom use, was measured on the basis of frequency of correct and consistent condom use in the preceding 3 months. The main outcome was measured as a dichotomous variable, based on whether condoms were used 100% of the time (defined as "consistent condom use" or "safe sex") or not (defined as "inconsistent condom use" or "unsafe sex"). Data safety and confidentiality was also given due consideration.
| Results | |  |
A total of 175 respondents attending ART center at SSG Hospital participated in the study. Sociodemographic profile of these respondents is shown in [Table 1]. Two-third of participants were in age group of 26-40 years, followed by close to 23% in age group of > 40 years and only half a quarter in the age group of ≤ 25 years. Majority (92.6%) of the respondents followed Hindu religion, 71% of the respondents were married, and 16% were illiterate. Forty-four percent belonged to lower socioeconomic class and nearly half of the participants came from urban area. | Table 1: Sociodemographic characteristics of the respondents registered at ART Center at Shree Sayaji general hospital, Vadodara
Click here to view |
As shown in [Table 2], majority (62%) of the participants were diagnosed at Integrated Counseling and Testing Centers (ICTCs) of government hospitals. The median time since HIV diagnosis and initiation of ART among participants was 24 and 18 months, respectively. Seventy-eight percent of PLWHAs were counseled regarding sexual behavior and among them almost one-third participants were also provided counseling by doctors apart from counselors. Almost all (96.3% in both groups) were demonstrated the correct method of condom use during counseling and were also counseled about use of new condoms during each sexual act. Seventy percent of PLWHAs were offered counseling with spouse.
Regarding their sexual behavior, close to 43% of PLWHAs practiced premarital sex and nearly 97% of them did not use condoms during premarital sex as presented in [Table 3]. Close to two-thirds had it with friend, fiancé, or a relative; whereas, almost 25% had it with a commercial sex worker (CSW). Among those who had premarital sex with friend, fiancé, or relative, majority cited the reason for the same to be friendship or love. Whereas the reasons cited for having premarital sex with CSWs were fun or curiosity. People practicing premarital MSM (men who have sex with men) type of sex cited the reason to be fun; whereas, the reason for premarital sex with employer or colleague was cited to be love or fun. Forced or threatened premarital sex or premarital sex under the influence of alcohol was not cited by anyone.
Moreover, 15% of the respondents reported that they were having extramarital sex (EMS) and 90% of them did not use condoms during EMS. Majority had friends, CSW, or an employer/colleague as partners. Major reasons cited were friendship, love for EMS with friends; fun or dissatisfaction with spouse for EMS with CSW; and love or fun for EMS with employer/colleague.
Looking at the current sexual practices by the respondents, it was observed that almost two-thirds of PLWHAs had only one sexual partner. A quarter of respondents also reported no sexual activity. However, around 6% respondents reported having more than one partner. Similarly, around 80% of the respondents reported having sexual activity less than three times a week. Nearly 60% of PLWHAs indulged in unsafe sexual practices and 60% of them did not communicate regarding safe sexual practices with their partners.
As shown in [Figure 1], reasons for unsafe sex among PLWHAs, before HIV diagnosis were: Lack of awareness about HIV/condoms (85%), desire for child (10%), more fun/pleasure (4%), and husband disliking condoms (1%). While after HIV diagnosis, the reasons for not using condom were: Desire for child (40%); husband disliking condoms (16%); more fun/pleasure (11%); non-disclosure to partner (10%); while others were forgetfulness, nonavailability of condoms, starting of ART, and both husband-wife being seropositive.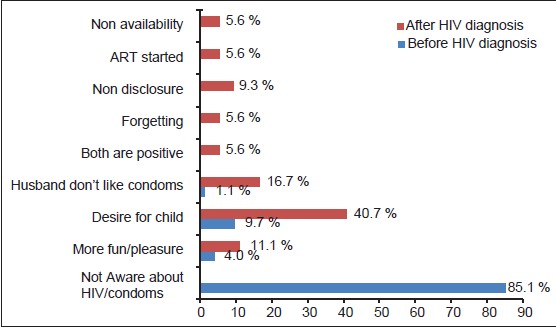 | Figure 1: Reasons for unsafe sex before and after HIV diagnosis among PLWHA
Click here to view |
In case of more than 90% of our respondents, their serostatus was known to the spouse or the regular partner. However, almost 90% of such disclosures were involuntary. Close to 90% of the respondents had their spouse tested for HIV and among them almost two-thirds had a seropositive spouse.
| Discussion | |  |
Majority of the participants were in sexually active and productive age group. These findings are very much similar to the national level statistics by National AIDS Control Organization (NACO). NACO has reported that 89% of the cases are in the age group of 15-44 years. This section of the population is more affected because they are economically productive, sexually more active, and the social structure is patriarchal. [2] With regard to the level of education, nearly 80% of the participants were literate and these findings were more or less similar to a study conducted by Joshi et al. [10] Close to 60% participants were employed and nearly 10% participants reported loss of job after HIV diagnosis. More than half of the participants belonged to lower socioeconomic class (Class IV and V) as per modified Prasad classification. [11] Sircar et al., also reported in their study that majority of patients (80%) were from lower socioeconomic class. [12] These findings are in agreement with contention that HIV spread is "fastest and farthest" in conditions of poverty and lack of information. The World Bank analysis of 72 countries also showed that at the national level, both low per capita income and unequal distribution of income are associated with high rates of HIV infection. [13] Majority of the participants were from urban areas, while still nearly 40% were from rural area. Similar place distribution of PLWHAs was also noted in a study by Jayarama et al., in south India. [14]
Almost two-thirds of the patients came to avail ART during the first and second stage of the disease which can be taken as a sign of quality referral from ICTC centers and the impact of large scale IEC campaigning at state and national levels. However, the remaining one-third PLWHA came late in the course of disease which could negatively affect treatment outcome.
Among other investigations, CD4 count is one of the most reliable investigations for clinical staging of PLWHA. It is used to make decision on treatment initiation along with opportunistic infections. ART is started when CD4 count goes below 350/mm 3 . [15] The median CD4 count was 305/mm 3 and the median duration since starting on ART was 18 months. Three-fourth of participants reported having received counseling regarding sexual behavior. This is particularly worrisome since the program guideline expects all the PLWHAs to be offered counseling on continual basis. Our experience at the ART center shows that looking at the patient load for ART, the counselors at the ART center are also hard-pressed against time to provide counseling to ART patients. Further, since these patients are coming to the ART center every month, it may be taken for granted that they would have already been counseled on sexual behavior and hence such counseling on safe sex practices may be taken lightly during subsequent visits. The program needs to respond to such challenges in the form of strengthening the counseling during follow-up visits since counseling on sexual behavior is equally important after starting ART as the risk of transmission of HIV continues after starting of ART. This is particularly important in the backdrop of unfavorable attitudes among PLWHAs in the form of reducing safe sex after starting ART.
Majority of the participants recalling being provided with counseling on correct and consistent condom use was a welcome finding. Correct and consistent condom use would go a long way in prevention of further transmission of HIV to their discordant partners. The program guideline encourages providing such counseling with spouse and defines it as partner notification. However, partner notification has not been made mandatory as of now as per program guidelines. [16] Yet, majority of the respondents receiving such counseling with spouse is again a welcome finding.
Relatively fewer numbers of respondents (15%) reported having EMS as compared to premarital sex (43%). It is important to note that more than 90% of such premarital and extramarital sexual encounters were unprotected. Similarly nearly two-third of the respondents had current unsafe sexual practice. A recent multicenter Indian study by Venkatesan et al., also reported about one-third (30.9%) of men and one quarter (26.5%) of women PLWHAs showing inconsistent condom use for vaginal or anal sex with regular partners. [17] Such figures are very high in the context where we are now focusing on the PLWHAs to prevent further transmission of HIV to their partners apart from raising awareness among general population on safer sex practices.
Poor partner communication regarding safe sex was noted. Although the proportion of those who could not raise the discussion of safer sex with their partners was slightly higher among female respondents as compared to males; however, the difference was not statistically significant. Among those who had discussed safer sex with partners, as high as two-thirds could not convince them for safer sex.
A range of reasons were mentioned by the respondents for not using a condom. Before HIV diagnosis majority of them reported that they were unaware about HIV/AIDS so they did not use a condom during sexual activity; while after HIV diagnosis, the desire for a child was the common reason cited for not using a condom.
Some other important reasons which were mentioned are partner disliking condoms; both partners being seropositive, and nonavailability of condoms. A study conducted by Wig et al., in tertiary healthcare center in north India among PLWHAs found that the reasons for an infrequent condom use among PLWHA were males feeling uncomfortable using it (83%), condoms being not available when needed (42%), the reduced sexual pleasure on using condoms (64%), and a wrong belief about no need for condoms for seroconcordant couples. [18]
Still there is a gap in providing correct knowledge to PLWHAs regarding safer sex because still many PLWHAs believe that there is no need of condom usage as their partner is also seropositive. However, the major issue which is of concern here is that many PLWHAs had correct knowledge regarding consistent condom usage, yet this did not translate into practice among them. Majority of the reasons mentioned here for unsafe sexual practices can be focused upon in their counseling sessions. To make condoms available at the ART centers should be taken care of by the providers.
Disclosure offers a number of important benefits to the infected individual and to the general public. Disclosure may lead to improved access to HIV prevention, treatment, opportunities for risk reduction, and planning for the future. It also enables couples to make informed reproductive health choices, which may ultimately lower the number of unintended pregnancies among HIV/AIDS positive women. [19]
We enquired about disclosure of serostatus in three distinct environments; spouse, other people in immediate environment, and sexual partners other than spouse. Almost 90% of such disclosures were involuntary. This highlights the fact that our sociocultural environment is yet not conducive enough to empower PLWHAs to go for voluntary disclosure of their serostatus to their spouse and family members. Venkatesan et al., in their multicenter study from India also reported that most participants (87.6% of males and 94.9% of females) disclosed their HIV status to their regular partners of which in more than 80% of participants it was involuntary. [17] Taraphdar et al., in her study among PLWHA attending a tertiary care center in India found 70% disclosure rate which was mainly by the healthcare professionals. [20] Serostatus of the spouse was not found to have any effect on the disclosure by respondents.
Earlier, a range of various benefits and consequences of disclosure as perceived by the PLWHAs had been enquired qualitatively in the same set up in Vadodara by Patel et al. [7] Major perceived benefit of disclosure that came out from our respondents was more care taken by the spouse as reported by almost half of those who had disclosed their status. The most common problems after disclosure reported by our respondents was child bearing issues (wherein there is a conflict of opinion between the partners regarding the decision whether to have a child or not) as reported by close to a quarter of ART respondents. Around one-fifth also reported family breakdown and divorce as negative consequences after serostatus disclosure.
Whereas disclosure to spouse was found in more than 90% of respondents, only 60% PLWHAs had their serostatus known to some other person than spouse. In this category close to 90% of the respondents had disclosed their serostatus to a family member. Nearly 13% had disclosed to friends, while few had disclosed their serostatus to neighbors or to someone in the community or at workplace.
Among those who had sexual relations with partners other than spouse, more than 95% had not disclosed the serostatus to such partners. Similarly, they also were unaware about the serostatus of these other-than-spouse-partners. It is important to note that a substantial proportion of those respondents that had multiple sexual partners had reduced the number of sexual partners to single or none after HIV diagnosis. This may be the reason for nondisclosure to and unknown serostatus of such partners.
| Conclusion | |  |
Nearly 20% of PLWHAs did not receive counseling regarding sexual behavior. The proportion (58%) of those practicing unprotected sex was still higher among PLWHAs even after HIV diagnosis. Premarital and extramarital sexual practices were seen among 43% and 15% of respondents, respectively. Majority (> 95%) of these practices were unprotected.
Reasons encountered for unsafe sex before HIV diagnosis was lack of awareness about HIV/AIDS for majority (80%) of PLWHA; whereas, after HIV diagnosis, desire for child (40%) followed by condom dislike by partners (20%) were reasons given by PLWHAs.
More than 95% of respondents had disclosed their serostatus to their spouse, more than 90% of such disclosures being involuntary. Nearly 44% of them had positive consequences after disclosure. There were also a considerable number of respondents who did not mention their serostatus to other partners and had unprotected sex with HIV negative and unknown serostatus partners.
| Recommendation | |  |
In view of the large proportion (almost half) of the study respondents engaging in unsafe sexual practices, it is imperative to stress the importance of using condoms for safer sex among PLWHAs not only to prevent transmission to their partners but also to help them avoid contracting sexually transmitted infections and potentially resistant HIV strains in case of seroconcordant couples.
In light of the fact that almost one-fifth of the PLWHAs reported not having received counseling, it becomes important to strengthen the counseling session during follow-up visits as the risk of transmission of HIV continues even after initiation of ART. At the partnership level, voluntary serostatus disclosure to the partner and communication with the partner about safer sex needs to be encouraged; while at the programmatic level, emphasis on need-based sexual behavior-related motivational counseling is required.
| References | |  |
| 1. | National AIDS Control Organization (NACO) 2010. HIV sentinel surveillance and HIV estimation in India 2008-2009: A technical brief. 
|
| 2. | National AIDS Control Organisation (NACO). Department of AIDS Control, Ministry of health and Family Welfare Annual Report; 2010-2011. 
|
| 3. | Zekan S, Novotny TE, Begovac J. Unsafe sexual behavior among HIV-infected patients in Croatia, 2006: Prevalence and associated factors. AIDS Behav 2008;12:S86-92. 
[PUBMED] |
| 4. | Kalichman SC. Psychological and social correlates of high risk sexual behavior among men and women living with HIV/AIDS. AIDS Care 1999;11:415-27. 
[PUBMED] |
| 5. | Vittinghoff E, Scheer S, O'Malley P, Colfax G, Holmberg SD, Buchibinder SP. Combination antiretroviral therapy and recent declines in AIDS incidence and mortality. J Infec Dis 1999;179:717-20. 
|
| 6. | Counseling and HIV/AIDS. UNAIDS Best Practices Collection. Geneva: UNAIDS; 1997. 
|
| 7. | Patel S, Baxi RK, Mehta M, Patel SN, Golin CE, Bakshi H, et al. Sexual behavior among persons living with HIV/AIDS (PLWHA) in Gujarat, India: A qualitative study. Indian J Soc Work 2012;73:177-93. 
|
| 8. | Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. Designing Clinical Research. 3 rd ed. Philadelphia: Lippincott Williams and Wilkins; 2007. 
|
| 9. | Epi_Info, Version 6.04_d. A word processing, database, and statistical programme for public health on IBM-compatible microcomputers. Atlanta: Centers for Disease Control and Prevention; 2001. 
|
| 10. | Joshi H, Rabindranath D, Arun KA. Clinicoepidemiological profile of HIV/AIDS patients in western India- A study from a teaching hospital. Indian J Prev Soc Med 2004;35:69-76. 
|
| 11. | Prosad BG. Changes proposed in the social classification of Indian families. J Indian Med Assoc 1970;55:189-99. 
|
| 12. | Sircar AR, Tripathi AK, Choudhary SK, Misra R. Clinical profile of AIDS: A study at a referral hospital. J Assoc Physicians India 1998;46:775-8. 
[PUBMED] |
| 13. | Katz J, Rosenberg A, Demery L, Shetty S, Yalamanchili S, Schafer H, et al. Towards new aid relationships to reduce poverty. Washington D. C.-The Worldbank, 2002 Available from: http://www.documents.worldbank.org/curated/en/2000/01/5108907/spa-5-2000-2002-towards-new-aid-relationships-reduce- poverty [Last accessed on 2013 Jun 22]. 
|
| 14. | Jayarama S, Shenoy S, Unnikrishnan B, Ramapuram J, Rao M. Profiles of attendees in voluntary counseling and testing centers of a medical college hospital in coastal Karnataka. Indian J Community Med 2008;33:43-6. 
[PUBMED]  |
| 15. | Antiretroviral Therapy Guidelines for HIV-Infected Adults and Adolescents Including Post-exposure Prophylaxis. National AIDS Control Organization, Ministry of Health and Family Welfare, New Delhi; 2007. 
|
| 16. | Operational Guidelines for Integrated Counseling and Testing Centres. New Delhi: National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India; 2007. 
|
| 17. | Chakrapani V, Newman PA, Shunmugam M, Dubrow R. Prevalence and contexts of inconsistent condom use among heterosexual men and women living with HIV in India: Implications for prevention. AIDS Patient Care STDS 2010;24:49-58. 
|
| 18. | Wig N, Sakhuja A, Agarwal SK, Khakha DC, Mehta S, Vajpayee M. Multidimensional health status of HIV-infected outpatients at a tertiary care centre in north India. Indian J Med Sci 2008;62:87-97. 
[PUBMED]  |
| 19. | Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: Implications for prevention of mother to child transmission programmes. Bull World Health Organ 2004;82:299-307. 
[PUBMED] |
| 20. | Taraphdar P, Dasgupta A, Saha B. Disclosure among people living with HIV/AIDS. Indian J Community Med 2007;32:121-7. 
|
[Figure 1]
[Table 1], [Table 2], [Table 3]
|