|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 2
| Issue : 2 | Page : 39-44 |
|
Prevalence and correlates of bacterial vaginosis among human immunodefficiency virus positive pregnant women at Aminu Kano Teaching Hospital, Kano, Nigeria
Halima Bello, Sule A Gaya, Zainab D Ahmed, Hadiza S Galadanci
Department of Obstetrics and Gynaecology, Aminu Kano Teaching Hospital, Kano, Nigeria
| Date of Acceptance | 15-Mar-2015 |
| Date of Web Publication | 3-Jul-2015 |
Correspondence Address:
Hadiza S Galadanci
Department of Obstetrics and Gynaecology, PMB 3452, Kano
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157.159964

Background: Bacterial vaginosis (BV) is one of the most prevalent causes of vaginal discharge or malodor and has been associated with several pregnancy complications including increased risk of mother to child transmission of human immunodeficiency virus (HIV) during pregnancy. Objective: To determine the prevalence of BV among HIV-positive pregnant women attending antenatal clinic at Aminu Kano Teaching Hospital (AKTH), Kano. Subjects and Methods: This is a descriptive cross-sectional study carried out on 242 HIV positive pregnant women as the study group and 242 HIV negative pregnant women as the control group. Following administration of the questionnaires, high vaginal swabs was collected and tested for PH, whiff test and microscopy to identify clue cells. The data were analyzed using Epi info version 3.5. Chi-square test was used to determine the strengths of association between exposure (HIV) and outcome (BV) variables in the study and controlled groups. Association was considered statistically significant at P < 0.05. Results: The mean ages for both groups were 28.4 (standard deviation [SD] ± 4.45) and 28.7 (SD ± 4.88) years for reactive and nonreactive groups respectively. The women's parity ranged from 0 to 7 and mean parity were 1.91 and 2.05 for the reactive and nonreactive groups respectively. The overall prevalence of BV among pregnant women attending ANC clinic at AKTH was 43.2%. The prevalence of BV among HIV-positive pregnant women (71.3%) is significantly higher than that of HIV-negative pregnant mothers (28.7%), P < 0.001. Conclusion: Pregnant HIV-positive women have a higher risk of developing BV compared with their HIV-negative counterpart. Active screening for BV among HIV-positive pregnant women is advised.
Keywords: Aminu Kano Teaching Hospital, bacterial vaginosis, human immunodeficiency virus in pregnancy
How to cite this article:
Bello H, Gaya SA, Ahmed ZD, Galadanci HS. Prevalence and correlates of bacterial vaginosis among human immunodefficiency virus positive pregnant women at Aminu Kano Teaching Hospital, Kano, Nigeria. J HIV Hum Reprod 2014;2:39-44 |
How to cite this URL:
Bello H, Gaya SA, Ahmed ZD, Galadanci HS. Prevalence and correlates of bacterial vaginosis among human immunodefficiency virus positive pregnant women at Aminu Kano Teaching Hospital, Kano, Nigeria. J HIV Hum Reprod [serial online] 2014 [cited 2018 Feb 1];2:39-44. Available from: http://www.j-hhr.org/text.asp?2014/2/2/39/159964 |
| Introduction | |  |
The prevalence of bacterial vaginosis (BV) varies between countries and also between populations. [1] Prevalence of 10-50% has been reported among pregnant women while up to 85% among commercial sex workers was noticed. [2],[3],[4],[5],[6],[7],[8],[9],[10],[11] However, a low prevalence of 1.4% among antenatal women was reported in Ghana. [12] In clinical practice, BV is diagnosed using the Amsel's criteria, which includes a thin greyish homogenous discharge, vaginal fluid PH > 4.5, release of a fishy odor on adding alkali (10% KOH), and clue cells (bacteria adherent to epithelial cells seen on microscopy). Presence of any three of these four criteria confirms the diagnosis of BV. [13],[14],[15]
There is a strong association between BV and human immunodeficiency virus (HIV) infection. [14] Pregnant patients with BV have a 50-100% increased rate of preterm labor, low birth weight delivery, amniotic fluid infection and chorioamnionitis. [16] These are risk factors for increased mother-to-child transmission (MTCT) of HIV. There are several other mechanisms through which BV and other reproductive tract infections facilitate HIV transmission. It was also documented that there was a significant decline in the concentration of HIV in genital secretions following the treatment of sexually transmitted infections (STI's) and BV. [17],[18]
An active search for BV among HIV-positive pregnant women is not practiced in our ANC clinic. This study will help to provide data for formulating a policy to routinely screen BV among HIV-positive pregnant women. Furthermore, screening for and treatment of such infections will go a long way in reducing MTCT of HIV infection among HIV-positive pregnant women.
| Subjects and methods | |  |
The study was carried out at Aminu Kano Teaching Hospital (AKTH) from July to September, 2012. The hospital is a tertiary health care institution in Kano, Kano State which serves as a referral center for neighboring states such as Jigawa, Katsina, Bauchi, Yobe and Zamfara states. The hospital antenatal clinics are run 4 times/week. An average of 40 new patients is booked daily and about 160 patients are seen as follow-up cases. The prevention of MTCT (PMTCT) program has been fully integrated into the hospital's obstetrics services. The program includes PMTCT intervention offered in the ANC and labor room and during the postpartum period. In the ANC, HIV Counseling and Testing is offered to all new clients, with a right to "opt out." HIV-positive patients are provided antiretroviral (ARV) drugs (at least 2-3 ARV drugs) according to the revised national guidelines on PMTCT. Other interventions at the hospital are a modification of obstetric practices such as delay in rupture of the placental membrane and avoidance of assisted vaginal delivery and episiotomy. An average of twenty HIV positive patients are seen at the antenatal clinic weekly with an average of 5/day and thus, a total average of eighty positive patients per month.
The study is a descriptive cross-sectional comparative study where a total of 484 selected pregnant women attending the antenatal clinic at AKTH, who consented, over the study period were studied using a designed questionnaire. These include 242 HIV-positive pregnant women as the study group and 242 HIV-negative pregnant women as the control group. The sample size was obtained using a standard formula (n = Z 2 P (1 − P)/d 2 ) and the prevalence of BV among pregnant women of 17.0% [10] was used. Each participant was enrolled once and those with genital malignancies in pregnancy were excluded. A systematic sampling technique was used whereby a sample interval was calculated following the division of the sample frame by the sample size.
Sample interval = sample frame (800 patients per week × 3 months = 9600)/484
This means that following selection of one consenting HIV positive pregnant woman, a twentieth HIV negative consenting pregnant woman was selected otherwise, the next consenting HIV-negative woman was selected for the study.
| Data collection technique | |  |
The women were counseled, to secure their consent to participate in the study. Questionnaires were structured and pretested, and this was administered to the consented clients. Two record officers were recruited to give numbers to all consenting women such that these numbers remained their permanent numbers until the end of the study. This was to avoid repetition.
The questionnaire consisted of information such as age, parity of the women, marital status, sociodemographic characteristics, history of current or previous STI's, HIV status, symptoms and complications associated with BV.
Following administration of the questionnaires, high vaginal swabs (HVS) is collected. The pH testing, using the red litmus papers, and application of KOH on the vaginal secretions gotten from the examination speculums (whiff test), were done. The HVS samples were sent to the main laboratory for microscopy, to identify clue cells. This was done by two appointed laboratory scientists.
The data were analyzed using Epi info version 3.5 June 2008, Centers for Disease Control Atlanta, USA. Data were presented in the form of tables. The Chi-square test was used to determine the strengths of association between exposure (HIV) and outcome (BV) variables in the study and controlled groups. Association was considered statistically significant at P < 0.05.
Ethical approval was obtained from the AKTH Ethical Committee.
| Results | |  |
A total of 484 participants were systematically selected and 469 responded giving a response rate of 96.8%. The data were analyzed, and the results are as follows.
The sample was divided into two groups; the study group regarded as group 1/reactive group and the control group regarded as group 2/nonreactive group, with 242 participants in each group.
The age of the participants ranged from 18 to 47 years and the mean ages were 28.4 (standard deviation [SD] ± 4.45) and 28.7 (SD ± 4.88) years for the reactive and nonreactive groups respectively. The majority of the women were within the age group of 20-29 years 56.2% and 59.5% for groups 1 and 2 respectively as shown in [Table 1]
The women's parity ranged from 0 to 7 for both groups and majority of them 166 (68.6%) and 144 (59.5%) for reactive and nonreactive groups respectively had their parities between 1 and 4. This was statistically significant at a P = 0.047. The mean parity was 1.91 and 2.05 in both groups respectively.
Almost all (96.7%) of reactive group and (97.1%) of nonreactive group were married and they came from the Hausa/Fulani tribe (52.4%/59.9%), which form the bulk of the study population. Most of them (99.5%) had a form of formal education ranging from primary, secondary to tertiary education while only 4.2% had no formal education.
Most of the husbands of the participants were either a civil servant, unemployed or private workers who worked in private organizations or go around doing their trading/business. More than half (25.3/52.3%) of the study population were private workers (nongovernmental) while only a few husbands were jobless (2.96%/0.8% respectively).
The overall prevalence of BV among pregnant women attending the antenatal clinic in AKTH, was found to be 43.2%.
However, the prevalence of BV among HIV-positive pregnant women within the study period was found to be 61.6%, which is significantly higher than that of HIV-negative pregnant women (28.7%) as shown in [Table 2].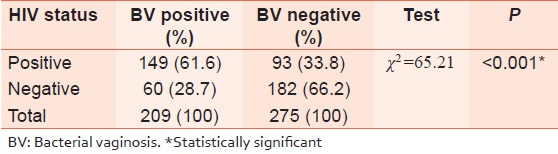 | Table 2: The prevalence of BV among the HIV positive and HIV negative women
Click here to view |
Other risk factors that are associated with BV were also analyzed, and the results were as represented in [Table 3].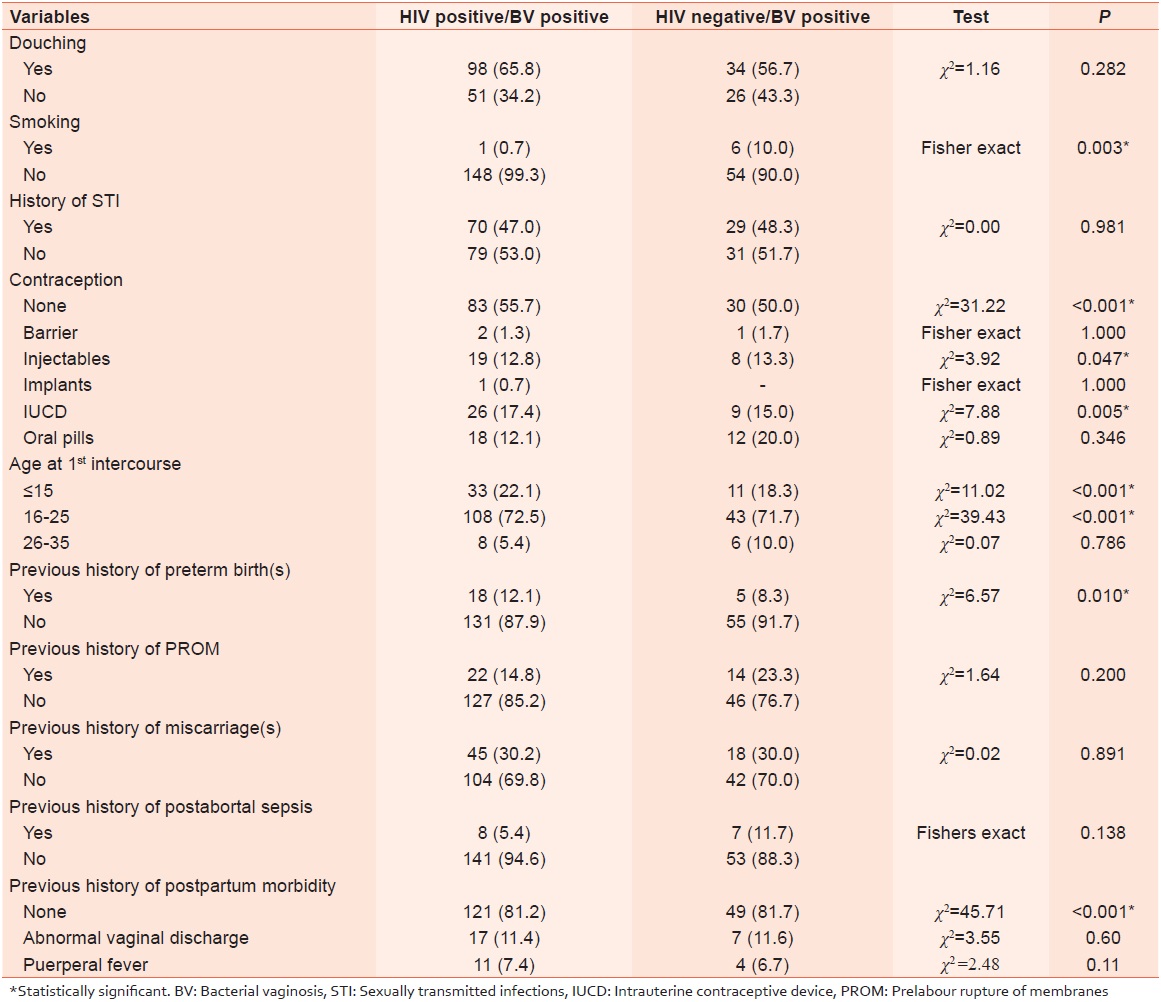 | Table 3: The influence of risk factors on the prevalence of BV among HIV positive and HIV negative women
Click here to view |
Smoking, use of contraceptives (Injectables and intrauterine contraceptive device [IUCD]), age at first intercourse <25 years and previous history of preterm births were found to be statically significant risk factors for acquiring BV.
Douching, history of STI and other risk factors were not found to be statistically significant in this study.
| Discussion | |  |
The overall prevalence of BV in this study was found to be 43.2% while that among the HIV-positive group was 61.6%. The prevalence of 43.2% found in this study is higher compared to 10.5%, [10] 17.0% [11] and 30.2% [19] reported in the Southeastern regions and Lagos respectively. This prevalence is also much higher than the very low prevalence reported in Ghana (1.4%) [12] and Ilorin (3.9%), [20] respectively. This variance in prevalence may be due to differences in the sociodemographic characteristics of the people and in the type of population studied.
However, the prevalence of BV among pregnant women had been reported in excess of 50% in sub-Saharan Africa. [21]
Only a few studies on BV in HIV-positive pregnant women have been reported compared to other population groups such as Commercial sex workers, young women of 15-59 years, HIV-positive women attending the sexually transmitted disease (STD) clinics and epidemiology research centers.
One of the largest population-based cohort study of BV in pregnancy carried out on Danish women was irrespective of HIV status and this gave a prevalence of 13.7% at enrolment only. [22]
The prevalence of 61.6% in this study among the HIV-positive women is much higher than the few similar studies available. It was reported in Malawi, to be 30% among HIV-positive women. [23]
These high prevalence may be related to the high HIV infection in sub-Saharan Africa. This suggests that HIV is a significant exposure risk factor for BV.
The Mechanisms by which BV is associated with HIV acquisition have been theoretically postulated to be by the suppression of innate mucosal immunity, weakening or breaching of intact cervico-Vaginal mucosa and alteration of normal vaginal microflora and vaginal PH, thus, leading to the subsequent secretion of the pro-inflammatory Cytokines/chemokines, which will enhance HIV survival. On the other hand, the HIV infection alters the local immune mechanism in the lower genital tract that makes the BV organisms to thrive and proliferates in the Vagina.
The increase in HIV load in the genital tract of women with BV leads to more exposure of the baby to this high viral load during the process of labor, and delivery thus, increasing the risk of MTCT of HIV. Also, other conditions such as prelabour rupture of membranes (PROM), chorioamnionitis and pretem labor associated with BV are all well known risk factors that accelerate MTCT of HIV. [24]
Other risk factors that have been associated with BV acquisition include intravaginal practices (douching), smoking, being single, previous genital infection/STD, multiple sexual partners, alcohol consumption, early age at first intercourse, postabortal/postpartum sepsis, intrauterine device (IUD) use and a prior pregnancy. The association between BV and HIV infection could not be explained by sociodemographic characteristics, douching, and STDs during pregnancy. However, smoking, use of IUD contraceptives, age at first intercourse <15 years, and previous history of preterm births were statistically associated with BV in this study.
The major risk factor reported in the study done in Urban Cities of Nigeria was unprotected sexual intercourse with multiple partners and during first sexual intercourse. [25] BV was also found to be more common among IUD users (47.2%) then non IUCD users (29.9%) such that it was recommended that Gram stain evaluation of BV be considered prior to IUD insertion. [26]
It was reported that BV was significantly associated with preterm delivery, abortions and maternal infections and that based on available evidence, screening and treatment of women at high risk of preterm delivery is recommended. [27]
The diagnosis of BV in this study was done by using Amsel's criteria though; Gram's staining of vaginal secretions is even more reliable than wet mount, with a sensitivity of 93% and specificity of 70%. [28] However, the gold standard for diagnosis of BV is microscopic criteria proposed by Nugent but the clinical criteria by Amsel's do not require laboratory facilities or specialized staff and there's no delay in obtaining the result. These made the diagnosis of BV in this study easier.
Bacterial vaginosis according to Amsel's criteria may be simplified using a combination of the two criteria; vaginal PH and amine test (KOH), in settings where microscopy or Gram staining is not available. In this study, all criteria, including microscopy were used.
In conclusion, this study showed that the prevalence of BV among HIV-positive pregnant women in AKTH is very high. BV has also been found to be significantly associated with some risk factors such as smoking, use of IUCD contraceptives and preterm births.
Routine screening and treatment of BV in antenatal women in AKTH is recommended to help reduce the MTCT of HIV infection.
Future research should include follow-up of the BV Positive HIV Pregnant women to compare the pregnancy complications with the BV Negative pregnant women and to evaluate the rates of MTCT of HIV among the HIV-positive women.
It is also possible in the future that routine screening and treatment will be the standard of practice.
| References | |  |
| 1. | Markusen TE, Barclay DL. Benign Disorders of the Vulva and Vagina. Current Obstetric and Gynaecologic Diagnosis and Treatment. 9 th ed. New York: Lange Medical Books; 2003. p. 651-76.  |
| 2. | Wiset W, Korakot S, Orawan K, Puntippa N, Ousnee W, Suratana P, et al. Bacterial vaginosis: A public health review. RCOG Br J Obstet Gynaecol 2001;108:439-50.  |
| 3. | McGregor JA, French JI. Bacterial vaginosis in pregnancy. Obstet Gynaecol Surv 2000;55 5 Suppl 1: S1-19.  |
| 4. | Bakare RA, Oni AA, Umar US, Adewole IF, Shokunbi WA, Fayemiwo SA, et al. Pattern of sexually transmitted diseases among commercial sex workers (CSWs) in Ibadan, Nigeria. Afr J Med Med Sci 2002;31:243-7.  |
| 5. | Dan M, Kaneh N, Levin D, Dan M, Kaneti N, Levin D, et al. Vaginitis in a gynecologic practice in Israel: Causes and risk factors. Isr Med Assoc J 2003;5:629-32.  |
| 6. | Poch F, Samra F. Vaginitis in a gynaecologic practice in Israel: Causes and risk factors. Isr Med Assoc J 2003;5:629-32.  |
| 7. | Riedner G, Rusizoka M, Hoffmann O, Nichombe F, Lyamuya E, Mmbando D, et al. Baseline survey of sexually transmitted infections in a cohort of female bar workers in Mbeya Region, Tanzania. Sex Transm Infect 2003;79:382-7.  |
| 8. | Behets F, Andriamiadana J, Rasamilalao D, Ratsimbazafy N, Randrianasolo D, Dallabetta G, et al. Sexually transmitted infections and associated socio-demographic and behavioural factors in women seeking primary care suggest Madagascar's vulnerability to rapid HIV spread. Trop Med Int Health 2001;6:202-11.  |
| 9. | Begum A, Nilufar S, Akther K, Rahman A, Khatun F, Rahman M. Prevalence of selected reproductive tract infections among pregnant women attending an urban maternal and childcare unit in Dhaka, Bangladesh. J Health Popul Nutr 2003;21:112-6.  |
| 10. | Laurent C, Seck K, Coumba N, Kane T, Samb N, Wade A, et al. Prevalence of HIV and other sexually transmitted infections, and risk behaviours in unregistered sex workers in Dakar, Senegal. AIDS 2003;17:1811-6.  |
| 11. | Ileogben SA, Lawrence UO, Jude U, Joshua AO. Bacterial vaginosis in antenatal patients in Abakaliki, Nigeria. Trop J Obstet Gynaecol 2006;23:100-4.  |
| 12. | Adinma JI, Okwoli RR, Agbai U, Unaeze N. prevalence of Gardnerella vaginalis in pregnant Nigerian Women. Afr J Rep Health 2001;5:50-5.  |
| 13. | Apea-Kubi KA, Sakyi B, Shinya Y, Ofori-Adjei D. Bacterial vaginosis, candida albicans and Trichomonas vaginalis infection in antenatal and gynaecological patients in Ghana. Trop J Obstet Gynaecol 2005;22:108-12.  |
| 14. | McDonald HM, Brocklehurst P, Gordon A. Antibiotics for treating bacterial vaginosis in pregnancy (Review). Cochrane Collab 2011. Published online on 19 January 2011. Available from: http://summaries.cochrane.org/CD000262/antibiotics -for treating bacterial vaginosis in pregnancy. [Last accessed on 2013 Mar 12].  |
| 15. | Oduyebo OO, Anorlu RI, Ogunsola FT. The effects of antimicrobial therapy on bacterial vaginosis in non-pregnant women. Cochrane Database Syst Rev 2009;3:CD006055.  |
| 16. | Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach DA, Holmes KK. Non-specific vaginitis: Diagnostic criteria and microbial and epidemiological associations. Am J Med 1983;74:14-22.  |
| 17. | Decena DC, Jennifer TC, Manalastas RM Jr, Palaypayon EP, Padolina CS, Sison JM, et al. Metronidazole with Lactacyd Vaginal gel in bacterial vaginosis. J Obstet Gynaecol Res 2006;32:243-51.  |
| 18. | Sewankambo N, Gray RH, Wawer MJ, Paxton L, McNaim D, Wabwire-Mangen F, et al. HIV-1 infection associated with abnormal vaginal flora morphology and bacterial vaginosis. Lancet 1997;350:546-50.  |
| 19. | Royce RA, Seña A, Cates W Jr, Cohen MS. Sexual transmission of HIV. N Engl J Med 1997;336:1072-8.  |
| 20. | Abudu DO, Odugbemi TO. Garnerella Vaginalis vaginitis in pregnancy. West Afr J Med 1985;4:5-8.  |
| 21. | Aboyeji AP, Nwabuisi C. Prevalence of sexually transmitted diseases among pregnant women in Ilorin, Nigeria. J Obstet Gynaecol 2003;23:637-9.  |
| 22. | Govender L, Hoosen AA, Moodley J, Moodley P, Sturm AW. Bacterial vaginosis and associated infections in pregnancy. Int J Gynaecol Obstet 1996;55:23-8.  |
| 23. | Thorsen P, Vogel I, Molsted K, Jacobsson B, Arpi M, Møller BR, et al. Risk factors for bacterial vaginosis in pregnancy: A population-based study on Danish women. Acta Obstet Gynecol Scand 2006;85:906-11.  |
| 24. | Taha TE, Gray RH, Kumwenda NI, Hoover DR, Mtimavalye LA, Liomba GN, et al. HIV infection and disturbances of vaginal flora during pregnancy. J Acquir Immune Defic Syndr Hum Retrovirol 1999;20:52-9.  |
| 25. | MOH. Riks factors for MTCT of HIV. In: National Guidelines on prevention of mother-to-child transmission (PMTCT) of HIV. F. Abuja, Nigeria: MOH; 2007. p. 2-3.  |
| 26. | Olawuyi O. The prevalence of Bacterial vaginosis among young women in Urban Areas in Nigeria and its major risk factor. Sex Trasm Infect 2011;87:A299-300.  |
| 27. | Joesoef MR, Karundeng A, Runtupalit C, Moran JS, Lewis JS, Ryan CA. High rate of bacterial vaginosis among women with intrauterine devices in Manado, Indonesia. Contraception 2001;64:169-72.  |
| 28. | Dadhwal V, Hariprasad R, Mittal S, Kapil A. Prevalence of bacterial vaginosis in pregnant women and predictive value of clinical diagnosis. Arch Gynecol Obstet 2010;281:101-4.  |
[Table 1], [Table 2], [Table 3]
|